8 Treating fibromyalgia associated with spine trauma
55% of fibromyalgia patients report gradual onset of symptoms as middle aged adults. 55% could not recall a precipitating event. 24% report onset after some physical trauma such as an auto accident, fall or surgery. 14% report onset after some psychological stressor. Various studies report that up to 88% of fibromyalgia patients are female, 92–100% are Caucasian, average age at onset is 29–37 years old, average age at presentation is 34–53 years old (Moldofsky 1975).
Fibromyalgia patients have reduced levels of the branch chain amino acids, reduced serum levels of serotonin, epinephrine, norepinephrine and growth hormone and increased levels of substance P in the spinal fluid (Juhl 1998). Fibromyalgia is 13.3 times more common in patients following cervical injuries than it is in patients who have had lower extremity injuries. A study from Israel documented a 22% prevalence of fibromyalgia 1 year after auto accidents causing whiplash injuries in comparison with 1% prevalence after accidents involving leg fractures (Buskilla 1997).
Fibromyalgia patients process pain differently from normal patients. Patients with fibromyalgia have augmented central processing of nociceptive stimuli in comparison with pain-free controls. When measured by EEG, fibromyalgia patients have changes of greater amplitude on both sides of the brain in response to painful stimuli. Pain-free controls responded on only one side of the brain with smaller evoked potentials (Mountz 1995).
The nerves respond more strongly to painful stimuli and the response lasts longer than is normal. There was an increase in late nociceptive evoked somatosensory response in 10 FMS patients as compared to 10 controls (Bennett 1994). SPECT scanning of the brain of a patient with fibromyalgia shows reduced blood flow in the caudate nucleus of the thalamus, which is a site of central pain processing. Fibromyalgia patients have the characteristic pain of allodynia in which non-noxious stimuli such as light touch are processed as painful (Kandel 1985, Bennett 1999).
There is evidence that pain perception in fibromyalgia patients is different in quality from healthy patients; fibromyalgia patients are more sensitive to pain. In normal controls the pain threshold increases gradually between 80 and 160 pressure units and spikes dramatically at 160 units of pressure. Fibromyalgia patients show a linear increase in pain intensity with pressure intensity at every level from 80 to 200 units of pressure. Animal studies show this same pattern due to central sensitization and lowered firing threshold in the dorsal horn cells (Bendtsen 1998).
Fibromyalgia diagnosis
Patients are tested with an algometer to determine the point at which they report pain with pressure. The ACR criteria say that this threshold has to be reached at 4 pounds per square inch pressure or less. Using an algometer ensures that the testing is reproducible and will allow for repeat testing to document decreases in sensitivity as the patient improves. The report of full body pain, fatigue and non-restorative sleep lasting for more than 3 months fulfills the diagnostic criteria (Moldofsky 1975, Russell 1986).
What is not fibromyalgia
• Chronic fatigue: Fatigue, cognitive problems, pharyngitis, swollen lymph nodes, low grade fever, substance P not elevated. Epstein–Barr viral titers and antibodies may be elevated.
• Depression: Check neurotransmitter profile by testing urine or using a questionnaire. Sleep disturbance with early morning awakening differs from fibromyalgia sleep disturbance and the cognitive dysfunction is different. FMS responds to smaller doses of anti-depressants. Rule out major depression.
• Hypothyroidism: Early hypothyroidism shows diffuse myalgia and fatigue. Laboratory values will be abnormal particularly TSH, T3, T4 and anti-thyroid antibodies. Body temperature is low in hypothyroidism but normal in FMS. Constipation, dry skin, and brittle hair are not characteristic symptoms of FMS. TSH is notoriously unreliable as a precise indicator of thyroid function. All parameters have to be taken into consideration.
• Primary growth hormone deficiency and/or hypogonadism (low testosterone in a male): When the complaint is muscle aches, fatigue, depression, exercise intolerance especially in a 20–40-year-old male, growth hormone and testosterone deficiency must be ruled out before a diagnosis of FMS or depression can be made. The history in growth hormone or testosterone deficiency may include a head injury, trauma or viral infection.
• Sleep apnea: Sleep apnea can cause fatigue and muscle aches. FMS can result from the stress response to sleep deprivation but if the patient has apnea the FMS can be easily resolved by correcting the apnea. Sleep apnea is at potentially fatal condition and proper diagnosis is crucial. Excessive daytime sleepiness, weight gain, reports of snoring or frequent nocturnal awakening should be followed up with a sleep study and CPAP prescription to correct the problem.
• Inflammatory muscle disease: While the symptoms of body pain and sleep disturbance (due to pain) are similar to FMS, muscle enzymes and sed rate will be elevated in this condition and are normal in FMS.
• Lyme disease: Lyme is reaching epidemic proportions in the US and is characterized by rapid symptom onset, rash, joint aches, positive antibody tests and may respond to doxycycline. The CDC diagnostic criteria requires that five out of five antibody markers be present for a definitive diagnosis but clinicians treating the condition report that if the patient has the symptoms and history characteristic of Lyme disease and have two or three of the antibody markers treatment is justified and useful.
• Parkinson’s: The patient will present with stiffness often interpreted as mildly painful but myofascial pain due to age related arthritis and sleep disturbance may confuse the picture. Patient may have tremor, loss of spontaneous movements and loss of facial expression.
• Polymyalgia rheumatica: Pain and stiffness in shoulders, trunk and pelvis usually found in patients over age 50 are characteristic. Sleep disturbance may be age related or due to pain. Sed rate will be elevated in PMR and is normal in FMS.
• Rheumatoid arthritis, lupus and systemic sclerosis: Fatigue and myalgia occur before articular symptoms and can be mistaken for FMS. RA factor, sed rate, ANA titer will be normal in FMS, abnormal in these conditions.
• Silicon breast implant reaction: History will include breast implants – even saline. Symptoms include dry eyes and mouth, painful joints. 70% have positive ANA. Symptoms can persist even after removal of the implant.
Before a patient is diagnosed with fibromyalgia the following blood work must have been ordered and values must be in the normal range: complete blood count (CBC), chemistry screen to evaluate liver and kidney function, sed rate, ANA titer, muscle enzymes, CRP, salivary or serum hormone levels including cortisol, progesterone, DHEA and testosterone, IgF1, TSH, T3, T4, anti-thyroid antibodies. A vestibular screening examination should be performed to rule out endolymphatic disorders.
Different etiologies of fibromyalgia
• Stress: One type of FMS seems to be associated with prolonged emotional or physical stress and physiologic sequelae of prolonged elevated cortisol
and other stress hormones and the subsequent adrenal depletion (Maes 1998, Adler 1999). The section below describing the physiologic effects of severe prolonged stress explains the mechanism by which stress can create fibromyalgia (Dessein 1999).
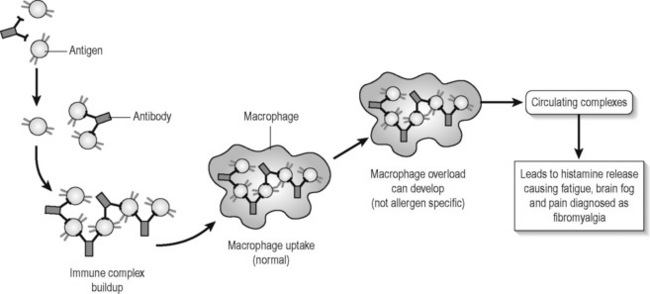
• IgG food sensitivities: FMS can be associated with “leaky gut” and IgG food or environmental allergies. Mast cell overload from elevated IgG complexes causes the release of histamine causing “brain fog” and fatigue and stimulating class C pain fibers to create widespread aching.
• Toxicity: This etiology of FMS is associated with one-time acute or long-term chronic exposure to organic chemicals, heavy metals or pesticides that change nerve membrane firing characteristics creating generalized body pain, cognitive dysfunction and fatigue. Liver enzymes, especially GGT, may be elevated. GGT is so frequently positive that many labs no longer include it in a standard chemistry screen. It is the most sensitive marker for liver inflammation and must be ordered specifically. History questions regarding previous places of employment and residence, previous job descriptions such as hair dresser, landscape maintenance, printer, or painter will reveal exposures to organic chemicals (Baker 1997).
• Genetic: This type has a genetic link, seems to run in families and may be associated with food sensitivities, especially gluten, or may represent an increased need for enzyme substrate in the liver detoxification or serotonin pathways.
• Viral: This type occurs after immunizations or viral illness. The symptoms may be from immune response to the virus or from nervous system response to the mercury preservatives in the immunizations.
• Vestibular injuries: This condition is not truly fibromyalgia but it is associated with the sleep disturbances and cognitive difficulties resulting from a vestibular injury or brain trauma. The sleep deprivation creates neuroendocrine stress eventually resulting in fibromyalgia. The patient will present with symptoms characteristic of FMS and the vestibular etiology has to be teased out during the history.
• Peri-menopause and trigger points: This type of FMS is associated with poorly managed menopause. Estrogen reductions cause sleep disturbance due to hot flashes and relative progesterone deficiency causes fatigue. Myofascial trigger points cause regional pain which can be in all four quadrants leading to central sensitization and a diagnosis of fibromyalgia. The solution for this etiology of fibromyalgia is proper hormone management and trigger point therapy using FSM (see Chapter 7) (McMakin 1998, 2004).
• Spine trauma: This type of fibromyalgia occurs after whiplash injuries, cervical or thoracic spine trauma, or after surgery and can be caused by any trauma that involves spinal flexion/rotation, spinal compression or ballistic segmental movement during a fall or impact (Bohlman 1979, Mendel 1989). The post-surgical cases are thought to occur when the neck is hyper-extended during intubation and constitute a cervical injury. Approximately 24–30% of fibromyalgia patients associate the onset of their condition with physical trauma although privately some clinicians have proposed the percentage to be closer to 50%. As a group they are the only FMS patients who complain specifically of pain in the hands and feet or describe their pain as burning.
All fibromyalgia patients, regardless of the etiology of their condition, have the same neuroendocrine and central sensitization features described in the fibromyalgia research but each etiology responds to different treatment strategies (Bennett 1999, Crofford 1998, Neeck & Reidel 1999). The model for the different types of fibromyalgia was developed when it was discovered that fibromyalgia could be successfully resolved when the treatment strategy addressed the specific cause or etiology of the pain or dysfunction.
Fibromyalgia from spine trauma – typical presentation and history
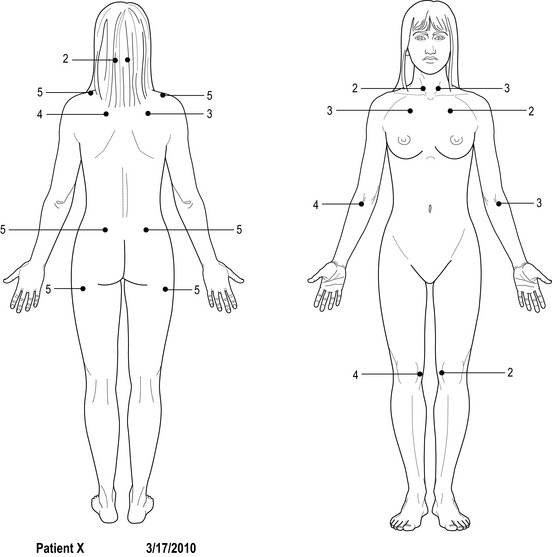
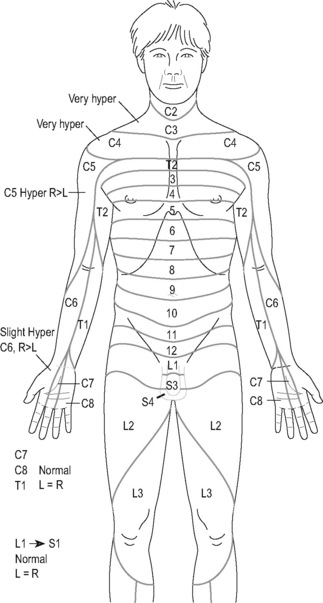
The pain diagram and symptom complaint describes aching burning midscapular pain, shoulder, neck, arm and hand pain that begins soon after the trauma and persists to varying degrees from the time of the injury to the date of presentation. Mid-scapular pain may represent referred pain from an injured cervical disc (Cloward 1959, Bogduk 1988). After some period of time, usually 1–6 months post-injury, the pain generalizes to the whole body, particularly down the thoracic and lumbar paraspinals, the gluteals and down both legs into the feet. The pain will be described as burning, aching, stabbing and sharp.
Imaging
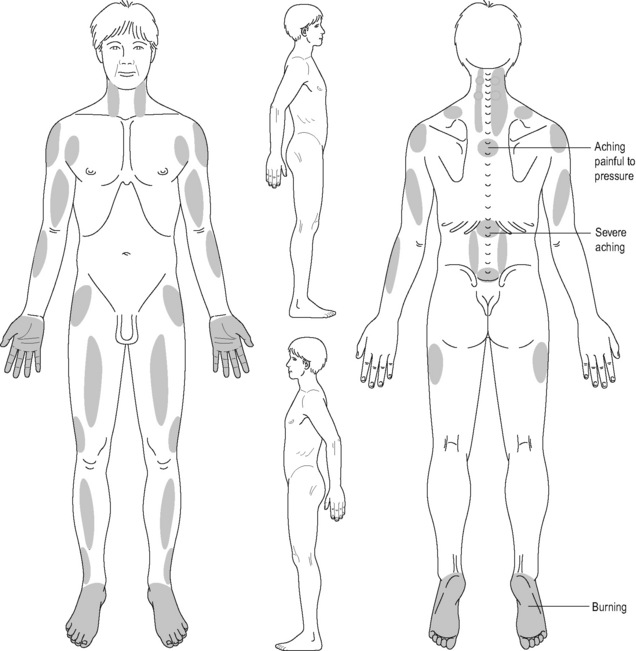
Figure 8.4 • The pain diagram for fibromyalgia associated with cervical spine trauma (CTF) differs from other fibromyalgia pain diagrams. As a group, CTF patients are the only fibromyalgia patients who describe their pain as burning and stabbing and report aching and burning in the hands and feet. This pain diagram is characteristic and predictive of a CTF diagnosis. It is virtually identical to pain diagrams characteristic of central pain except that central pain patients usually also report pain in the head and face (see Chapter 10).
small disc bulges are considered “normal” in a patient population. Many pain-free patients have disc bulges that do not produce symptoms. When the films were re-examined by a consulting radiologist specializing in spinal imaging the revised report described a central bulge or contained herniation.
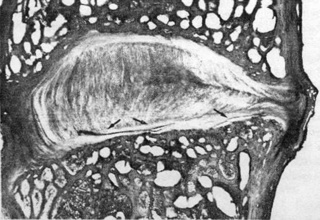
Figure 8.5 • This microscopic examination done at autopsy shows contained herniation and end plate fractures in a disc whose postmortem imaging was read as normal (reproduced with permission from Taylor & Twomey 1993). The patients in this study died from causes other than spine trauma during motor vehicle accidents.
How spine trauma leads to fibromyalgia
How could cervical spine trauma cause fibromyalgia and central pain sensitization? Trauma creates cracks in the disc annulus or the cartilaginous end plate and exposes the spinal fluid and spinal cord to the material in the disc nucleus. The disc nucleus contains neurotoxic concentrations of phospholipase A2 (PLA2) shown to cause nerve destruction in dogs, pigs and rabbits. PLA2 has been shown to be so inflammatory and neuro-toxic that it destroys nearby nerves in a dose related response (McCarron 1987, Olmarker 1993, 1995, Ozaktay 1995, 1998, Cavanaugh 1997, Chen 1997, Marshall 1997).
The damage to the discs shown by Taylor & Twomey (1993) occurs in the postero-lateral portion of the disc which is directly adjacent to the antero-lateral portion of the spinal cord. The paleospinothalamic tract is the outermost of the two tracts in the lateral column of antero-lateral cord and carries diffuse deep pain information up the spine to the thalamus, caudate nucleus and the cortex (Lombard 1983). This tract is the one closest to the portion of the disc most likely to be damaged (Netter 1991).
Trauma can cause direct mechanical disruption of the antero-lateral pathways and the spinal cord leading to deafferentation of these axonal pathways according to Taylor & Twomey (1993). Deafferentation in the antero-lateral ascending pain pathways in the spinal cord would produce what is essentially thalamic or central pain. Disruption of pain pathways in the spinal cord leads to central pain:
Treating fibromyalgia associated with spine trauma
Medical science accepts as a given that fibromyalgia is an incurable condition and the randomized controlled studies done so far have had that view as a starting point. Controlled trials by their nature can study only one intervention as it affects one or more symptoms. Since fibromyalgia is a collection of multiple symptoms affecting numerous systems each affected by multiple influences, the possibility that any one intervention will produce remission of all symptoms or cure the condition is extremely remote, especially if one starts with the presumption that the condition is incurable. The clinical strategies that have created recovery for so many patients operate within a framework in which recovery, while not inevitable, is thought possible because it has been observed to be so (Teitelbaum 2001). It is left to the reader to decide which viewpoint is most productive.
The treatment protocol in this chapter was developed by trial and error in 1999 and found to be effective in eliminating pain in over 200 FMS patients with spinal trauma onset. Pain has been reduced from an average of 7.4/10 to 1.4/10 in every patient with hyperactive patellar reflexes, dermatomal hyperesthesia, a history of trauma and pain in the hands and feet. Reducing the pain is relatively easy; achieving recovery is more involved because of the neuroendocrine and metabolic disturbances (McMakin 2005).
Neeck & Reidel (1999) proposed, and it seems a reasonable hypothesis, that the pain itself serves as a chronic stressor elevating CRH in the hypothalamus. CRH in turn modifies levels of LHRH (luteinizing hormone releasing hormone), TSH (thyroid stimulating hormone), and GHRH (growth hormone releasing hormone) centrally contributing to disruptions in circulating hormones. Progesterone, growth hormone, thyroid hormone levels and thyroid receptor sensitivity are all affected. Chronic moderate neuropathic pain would be sufficient to cause the elevations in CRH found in fibromyalgia and the alterations in central pain processing common to fibromyalgia patients (Bennett 1999).
By the time the patient has been in moderate to severe pain for 1–2 years the symptoms generalize to include the classic neuroendocrine abnormalities seen in fibromyalgia caused by any etiology (Crofford, Demitrack 1996, Crofford, Engleberg, Demitrack 1996, Crofford 1998, Neeck & Reidel 1999). Understanding the neuroendocrine abnormalities is helpful when diagnosing fibromyalgia but it becomes crucial when attempting to resolve or cure it.
Understanding stress and neuroendocrine dysfunction
All repair systems and long-term physiologic processes are put “on hold” until the threat either kills you or resolves (Sapolsky 1994). This survival strategy is perfect for short-term attacks by tigers but creates problems when the stress persists in the form of moderate to severe pain lasting years.
Stress and thyroid
CRF suppresses thyroid stimulating hormone (TSH) centrally (Neeck & Reidel 1999). Primitive survival logic dictates that the stress hormones are stimulating enough and additional thyroid hormone would be hyper-stimulatory. Elevated cortisol from the adrenal glands suppresses the peripheral conversion of the T4 storage form of thyroid hormone into the T3 active form of the hormone. Many fibromyalgia patients present as if they are clinically hypothyroid complaining of weight gain, constipation, dry skin, hair loss, fatigue and feeling cold. The patient becomes functionally hypothyroid because T4 cannot convert efficiently into T3 but TSH is almost always found to be in the normal or upper end of normal range when tested. TSH cannot rise in response to the relative peripheral insufficiency because it is suppressed centrally by CRF.
Stress and gonadal hormones
CRF suppresses FSH (follicle stimulating hormone) and LH (luteinizing hormone) centrally (Sapolsky 1994). The long-term projects of ovulation, sperm production, copulation and pregnancy are put on hold until the threat is gone. In women FSH and LH promote maturation of the corpus luteum and its increased production of progesterone to balance the estrogen produced by the ovaries during the post-ovulatory portion of the menstrual cycle. If production of progesterone by the corpus luteum is insufficient to balance estrogen the patient experiences the symptoms of premenstrual syndrome (PMS) caused by estrogen dominance. The patient complains of fatigue, irritability, water retention, sleep problems and emotional lability. These complaints are common to fibromyalgia patients.
Stress and growth hormone
CRF suppresses growth hormone releasing factor (GHRH) centrally interfering with growth hormone secretion (Bennett 1997). In an adult, growth hormone facilitates amino acid transport across the cell membrane to enhance tissue repair. Growth hormone in an adult is released during stage IV sleep and in a burst about 1 hour after vigorous exercise. Fibromyalgia patients do not experience stage IV sleep and they do not have the normal burst following exercise due to CRF suppression. Without adequate levels of growth hormone the normal exercises and activities of life and the minor tissue damage that follows are not easily repaired. This explains why fibromyalgia patients experience days or weeks of muscle pain after simple exercise or exertion.
Stress and the brain
CRF acts as a neurotransmitter and modifies cognitive processing to interfere with short-term memory and modulate long-term memory. In acute stress the only short-term information processing required is the answer to: “How do I get away from this tiger?” which leads the brain to focus on: “How did I get away from the tiger the last time?” Fibromyalgia patients complain of problems with short-term memory, processing and memory for details and sequencing of activities and information. And long-term memory is biased toward remembering unpleasant events and how they happened (Henley 2001).
Stress, digestion and IBS
The proper acidic pH of gastric contents creates the environment that supports proper bacterial flora in the intestines. Acid-loving bacteria decline and other bacteria proliferate in the more alkaline environment created by bicarbonate from the pancreas and relative decrease of acid. Intestinal bacteria help to digest food and create short-chain fatty acids that maintain intestinal health. If stomach acid and pancreatic digestive enzymes are both insufficient food may not be adequately digested or absorbed. Large undigested food particles may putrefy in the gut creating the local allergic responses and inflammation characteristic of irritable bowel syndrome commonly seen in fibromyalgia patients. Elevated cortisol levels cause thinning of the gut wall and when combined with inflammation caused by dysfunctional digestion, can contribute to the loss of gut membrane integrity sometimes called “leaky gut”. Larger food molecules could leak across the membrane and encounter the immune system, contributing to food sensitivities commonly seen in fibromyalgia patients (Guyton 1986, Sapolsky 1994, Galland 1997).