5 Treating facet joint generated pain
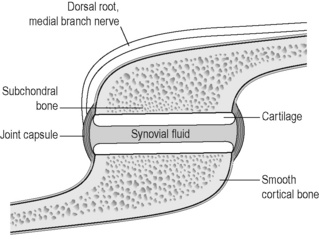
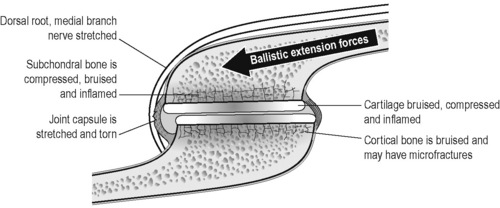
Facet joints are the posterior articulating joints in the spine. They carry most of the compressive load when the spine is in extension and guide motion during flexion, extension and rotation. High and low threshold mechanoreceptors and mechanically sensitive pain receptor nerves fire as the joint capsule is stretched and the cartilaginous joint surface compressed during joint movement. Proprioceptive nerve endings in the joint capsule fire during normal range of motion of the joint. Abundant free and encapsulated nerve endings and small nerve fibers capable of secreting substance P and calcitonin gene-related peptide (CGRP) enervate the capsule and joint surfaces. During trauma the joint approaches end range extension stretching the joint capsule and compressing the cartilage to the point of injury. Injury and inflammation of the facet joint and surrounding muscles excite and sensitize the nerves at the joint (Cavanaugh 1996). Excessive capsule stretch, seen in whiplash and hyperextension injuries, activates nociceptors in the joint capsule, leads to prolonged neural after-discharges and can cause damage to the capsule and to the axons in the capsule and is a probable cause of persistent neck and back pain. Facet joints have been implicated as a major source of low back and neck pain (Cavanaugh 2006).
Facet joints become painful as the joint tissues degenerate and become inflamed (Beaman 1993). The cartilage surface becomes irregular, frayed and calcified. The periosteum and subchondral bone becomes inflamed and calcified. Nerve fibers infiltrate the inflamed and degenerated tissues and secrete substance P in the eroded areas sending pain signals to the brain via the nerves and spinal cord. The nerves at the facet joint capsule transmit proprioceptive information in normal joints and pain information in inflamed or injured joints. Chen found more c-fiber receptors on the dorsolateral aspect of the facet joint where muscles and tendons were attached (Chen 2006). Inflammation leads to decreased firing thresholds and elevated baseline discharge rates of nerve endings in facet capsules (Cavanaugh 2006). Chronic inflammation leads to fibrosis between the nerves and soft tissues such as the capsule, the muscles and the fascia (Lewis 2004). These adhesions can make even normal motion painful as the nerves are stretched by the movement of the soft tissues to which they are adhered.
The reduced firing threshold, increased baseline neural discharge and perineural fibrosis in the injured and degenerated facet joint tissues feeds constant neural input into the spinal cord which feeds back to the muscles around the joint contributing to the formation of taut bands and myofascial trigger points in the paraspinal and postural muscles (Gerwin 2004). The myofascial trigger points compound the pain (Travell 1983, 1992) and the taut bands complicate joint function when the shortened sensitized muscle fibers contribute to joint compression and sensitized neural input and help perpetuate joint inflammation. This interaction between the nerve, joint and muscle forms a feed-back–feed-forward neuro-mechanical cycle that is very difficult to break once it becomes established and is the reason that chronic low back and neck pain is so pervasive and difficult to treat. To interrupt it effectively, all three aspects of dysfunction should be addressed at once. FSM makes this possible in most cases.
Identifying which pathologies in which tissues are creating the pain becomes important when treating with FSM because the frequency choices are specific to the tissue and pathology. FSM has been shown to decrease COX and LOX mediated inflammation, inflammatory cytokines and CGRP (McMakin 2005, 2007, Phillips 2000). FSM has been shown to decrease scar tissue and to reduce the pain associated with myofascial trigger points (McMakin 1998, 2004, Huckfeldt et al 2003). FSM has frequencies for calcium deposits and calcium influx into soft tissues, for nerve pain and for myofascial trigger points in the involved muscles.
Diagnosing facet joint pain
The pain will be worse with extension and sitting which compress the posterior joints and better with flexion which gaps the joints and relieves the pressure. The patient will state that they cannot lay prone at all and if laying supine must have the knees and hips flexed at 90 degrees. The pain will be worse with rotary motions that compress the joint on one side and move soft tissues that are adhered to nerves and the joint capsule. Movements that use trigger point laden muscles will create both local and referred pain from the myofascial trigger points. Inflammation in the facet joints can trigger neural pain and create dermatomal nerve pain although this is less common. The same injuries that traumatize and damage the facet joints can also damage the discs and the patient may have pain with flexion or rotation caused by disc inflammation (see Chapter 4).
Physical examination
Most practitioners reading this text have been trained to perform a physical examination to evaluate spine and facet joint pain. This brief description is meant to be a reminder rather than a comprehensive or definitive instruction. The reader who desires more complete instruction is referred to Hoppenfeld (1976) or Souza (2009) or a similar resource.
Treating chronic facet joint pain
• The patient must be hydrated to benefit from microcurrent treatment.
• Hydrated means 1 to 2 quarts of water consumed in the 2 to 4 hours preceding treatment
• Athletes and patients with more muscle mass seem to need more water than the average patient.
• The elderly tend to be chronically dehydrated and may need to hydrate for several days prior to treatment in addition to the water consumed on the day of treatment
• DO NOT accept the statement, “I drink lots of water”
• ASK “How much water, and in what form, did you drink today before you came in?”
• Coffee, caffeinated tea, carbonated cola beverages do not count as water.
3 Channel B: facet joint tissue frequencies
 Both frequencies are used when treating bone. It is presumed that one frequency is for cortical bone and one is for cancellous bone but it is not known what portion is addressed by which frequency.
Both frequencies are used when treating bone. It is presumed that one frequency is for cortical bone and one is for cancellous bone but it is not known what portion is addressed by which frequency. The periosteum lines the outside of the bone, interweaves with tendinous and ligamentous attachments and is very well innervated and pain sensitive.
The periosteum lines the outside of the bone, interweaves with tendinous and ligamentous attachments and is very well innervated and pain sensitive. Cartilage lines the facet joint and becomes damaged, degenerated, calcified and inflamed when traumatized by acute or chronic compression of the joint surface.
Cartilage lines the facet joint and becomes damaged, degenerated, calcified and inflamed when traumatized by acute or chronic compression of the joint surface. The joint capsule attaches to the periosteum, surrounds the joint and becomes fibrosed, calcified, scarred and inflamed when over stretched by trauma.
The joint capsule attaches to the periosteum, surrounds the joint and becomes fibrosed, calcified, scarred and inflamed when over stretched by trauma. The recurrent nerves innervating the joint capsule transmit proprioceptive information in the normal facet joint and pain information in the degenerated joint. They infiltrate the joint in response to chronic inflammation becoming fibrosed and scarred to the capsule and fascia as degeneration progresses. Dermatomal nerve roots may become painful as inflammatory peptides diffuse out from the inflamed facet joint tissues.
The recurrent nerves innervating the joint capsule transmit proprioceptive information in the normal facet joint and pain information in the degenerated joint. They infiltrate the joint in response to chronic inflammation becoming fibrosed and scarred to the capsule and fascia as degeneration progresses. Dermatomal nerve roots may become painful as inflammatory peptides diffuse out from the inflamed facet joint tissues. The fascia is the thin connective tissue covering surrounding the muscles and all soft tissues. The fascia becomes inflamed, calcified and fibrosed during the degenerative process.
The fascia is the thin connective tissue covering surrounding the muscles and all soft tissues. The fascia becomes inflamed, calcified and fibrosed during the degenerative process.• Artery and Elastic Tissue in the Muscle Belly: __/ 62
A/B pairs for scar tissue
The 58/’s will increase range of motion but do not change pain.

Caution: 58 / 00, 01, 02, 32
• Do not use these frequencies on injuries newer than 5 to 6 weeks old.
• Newly injured tissue must form scar tissue in order to repair itself.
• Removing the scar tissue seems to undo the healing by weeks in a new injury.
• The 58/’s can be used very briefly (15 seconds) to modify scar tissue as it is forming after the first four weeks.
• Never use this combination before the injury is 4 weeks old
Treatment protocol chronic facet pain
Channel A condition / Channel B tissue
58 / 00, 01, 02, 32
• A/B pair for Removing scar tissue and adhesions
• Treatment time: When used to treat chronic complaints the 58/’s are used in order as listed above for approximately 1 to 2 minutes each at the beginning of the treatment to soften the tissues and remove scar tissue. Facet joints have bone as a tissue so 58 / 01 is usually included in the protocol. For those practitioners who can feel the softening produced by the frequency, it is often helpful to run the frequency until the softening is reduced and the tissue becomes relatively more firm. There may be some patients in whom one or more of these frequencies will produce softening for up to 3 to 4 minutes.
40 / 396, 59, 39, 783, 157, 480, 191, 100
• Inflammation / Nerve, bone, periosteum, cartilage, capsule, tendon, ligament.
• Treatment time: Use these combinations for 2 to 4 minutes each. Research has shown 40Hz to have a time dependent response in a mouse model of inflammation. 50% of the reduction in inflammation was present at 2 minutes. The full response was present at 4 minutes. Treat the nerve first as it seems to relax the muscles and allow better palpation of the facet tissues. The periosteum is the most pain sensitive part of the bone and the nerve and the joint capsule are the most sensitive to inflammation and should respond best to this frequency. This protocol should reduce the joint pain but will not change range of motion.
91, 13 / 142, 396, 480, 783, 157, 191
• Calcium ions, scar tissue / fascia, nerve, joint capsule, periosteum, cartilage, and tendons.
• 91 / 783, 480, 157, 396 seems to reduce joint pain most effectively and softens the joint capsule dramatically.
• 13 / 142, 396, 480 usually increase range of motion most effectively. Scarring between the capsule and the nerve appear to create sharp pain with palpation and respond well to treatment. See manual technique below.
• Treat all the tissues if time allows.
• Treatment time: Use these combinations for 1 to 2 minutes each or if you are sensitive to the feel of tissue softening and time allows, use the frequency as long as the softening happens.
Treat the muscles
When treating the facet joint remember to treat the muscles and trigger points. The taut muscles act as confounding pain generators and at the same time compress the facet joint increasing the degenerative forces on both the facet joint and the disc (see Chapter 7).
Treat the psoas and lumbar paraspinals muscles in the low back.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree