10 Treating concussion, central pain and emotions
A traumatic brain injury (TBI) is associated with loss of consciousness, post-traumatic amnesia in which the patient cannot remember the events leading up to the trauma for periods up to several days and focal neurological signs (de Kruijk 2002). A mild traumatic brain injury (mTBI), the most common form of concussion, is usually defined as one in which loss of consciousness (LOC) is less than 30 minutes and the Glasgow Coma Scale (GCS) score is more than 13 at the time of injury. A GCS score of 3 signifies deep coma and a GCS score of 15 signifies a fully alert and oriented patient spontaneously conversing and following commands. In an mTBI, the patient may have incomplete memory of the traumatic event and post-traumatic amnesia (PTA) of less than 24 hours and may have been dazed and confused at the scene without loss of consciousness. An example would be the driver of the target vehicle in a rear end accident who does not remember the sound of the impact or who does not remember anything between the time she saw the impact vehicle approaching and the time several minutes later when the police officer arrived at the car window (McCrea 2002, McAllister 2002, Ropper 2007, Ryan 2003).
Incidence of traumatic brain injuries
There are 1.5 million traumatic brain injuries affecting 128 people per 100,000 in the United States every year and even though 85% are considered mild they result in significant disability and unemployment due to the cognitive, psychological and social dysfunction they cause (Ropper 2007). Sports and bicycle accidents account for the majority of cases among 5–14-year-olds and falls and motor vehicle accidents are the most common cause of concussion in adults. Post-concussive syndrome or post-concussive symptoms (PCS) refer to a constellation of signs and symptoms that may be reported after a TBI of any severity. Post-concussive symptoms affect up to 50% of mTBI patients at one month and 15–25% at one year. Some post-concussive patients never return to their pre-morbid function (Alves 1993, Middelboe 1992). Litigation and compensation factors involved in injuries sustained in the workplace or in auto accidents are thought to affect both symptom reporting and rates of recovery (Mooney 2005).
CT scans should be done to evaluate the need for neurosurgical intervention, even in the presence of a normal neurological examination, if the patient is under 16 or older than 65 years of age, has a GCS of less than 15 within 2 hours after the injury, two or more episodes of vomiting, retrograde amnesia for greater than 30 minutes prior to the trauma or is taking anticoagulants (Ropper 2007). CT and MRI scans while easily available and adequate to diagnose gross pathology such as hematoma, frank swelling or depressed skull fracture are not sensitive enough to show the subtle reductions in cortical perfusion, frontal and temporal hypometabolism and diffuse axonal injuries that have been demonstrated on PET or SPECT in mTBI patients with persistent PCS. Several studies have demonstrated abnormal frontal and temporal lobe activity with PET and SPECT scans in TBI/PCS patients whose CT and MRI scans were normal (Gross 1996, Ruff 1994, Humayun 1989, McCrea 2008).
Pathologies associated with TBI
Multifocal axonal injuries, increased permeability of the axonal membrane due to inflammation and activation of the glial system, disruption of axonal neurofilaments leading to disruption of axoplasmic flow and secondary axonal deafferentation in the areas of the brain served by the damaged axons have been observed after mild brain trauma in both human and animal studies (Oppenheimer 1968, Blumbergs 1994). Human postmortem studies have shown loss of cortical cholinergic afferents that would account for dysfunction in hippocampal cholinergic neurons and the resulting symptoms of memory loss and difficulty with information processing (Dixon 1994, Saija 1988, Murdoch 1998, Dewar 1996). Even mild brain injury has been shown to produce evidence of diffuse axonal injuries (Povlishock 1989, 1992, 1995). Sleep disturbances common in TBI patients are thought to be produced by injury to the reticular activating system that regulates sleep–wake cycles.
There are no universally effective treatments for post-concussive symptoms (Bazarian 2005). Tincture of time produces some recovery of function. Cognitive behavioral counseling for patients and their families at the time of the injury helps patients deal with the deficits, creates realistic expectations and reduces anxiety about symptoms. Medications and various strategies are used to modify post-concussive symptoms.
Dysfunction in the cholinergic, catecholaminergic and dopaminergic neurotransmitters may all contribute to cognitive impairment. It is clear that disruption in cortical cholinergic function is a primary source of cognitive dysfunction but some patients respond best to cholinesterase inhibitors and others to psychostimulants that increase catecholamine levels. Both classes of medications are intended to improve attention and working memory although it is advisable to start with low doses and titrate up in small increments (McAllister 2002).
In spite of these strategies symptoms from TBI persist for years following even mild head trauma and create significant disability. In 1999 the National Institutes of Health declared mTBI and post-concussive sequelae to be a major public health problem (NIH 1999).
Van Gelder’s concussion model
The second concept of concussion is particular to one physician, a Dutch osteopath and naturopath from Australia who trained in England in the 1930s and came to practice in Vancouver, British Columbia in 1946 (Van Gelder 1985, 1989). Harry Van Gelder was mentioned in Chapter 1 of this text and it is he who bought the practice that came with the 1920s machine that came with the list of frequencies that allowed him to treat a multitude of physical conditions and complaints successfully using electromagnetic resonance along with other therapies. Although somewhat eccentric, Harry Van Gelder was beloved and acknowledged by those he treated as being superbly effective and skilled as a diagnostician and healer. He developed a more subtle concept of “concussion” to mean any shock or trauma to the system that had an impact on the medulla or brain stem. Van Gelder’s skill, reputation and clinical outcomes lead to the consideration of this more subtle condition as a treatment focus.
Concussion protocol treatment outcomes
Concussion protocol increases serotonin
The data acquired through micro-immunochromatography demonstrated that the concussion protocol produced a significant but probably temporary increase in serotonin levels. Serotonin decreased during the treatment that reduced pain in fibromyalgia patients (see Chapter 8). When the pain reached 0/10 VAS or had stopped decreasing the protocol was changed and for the next 30 minutes the patient was treated with the “concussion protocol”. The patient was blinded to the change in treatment. Serotonin levels dropped during the pain reducing portion of the treatment in every patient treated and rose with use of the concussion protocol from an average of 175.75ng/ml (± 40.20) to 244.34ng/ml (± 76.05) in each of 16 different patients whose samples were collected during the 2-month test period. The normal range for serotonin is 100–300ng/ml.
Diagnosing concussion
• History: Directed questioning may reveal symptoms the patient does not associate with the injury. Be aware that the patient may not be an accurate historian or may simply lack the self awareness to assess their own performance and cognitive function. When there is any doubt the patient’s family should be consulted.
• Memory and decision making problems: Are you having any problems with being forgetful? Are you having any unusual problems with memory for numbers, names, facts or words? Is decision making any more of a problem for you now than it was before the accident?
• Task sequencing: Is it difficult for you to accomplish projects that require multiple steps? Are you having problems performing errands in sequence, getting a meal on the table, or planning multistep projects?
• Sleep disturbance: Are you having any problems with getting to sleep or staying asleep?
• Fatigue: Are you more fatigued than you were before the injury? Do you fatigue more easily than you did before the injury?
• Mood: Are you more anxious, irritable, or depressed than you used to be? Do your moods shift more easily than they used to? Do you find yourself yelling or losing your temper more often than is normal for you?
• Balance and co-ordination: Do you have any new problems with balance? Can you walk around your home when you get up at night in the dark or do you need a light on? Do you fall or bump into things more often than usual?
• Hormones: Are you having any menstrual cycle irregularities (progesterone and estrogen balance)? Are you having any prostate symptoms (testosterone and estrogen balance)? When did you start having problems with acne (testosterone excess)? Have you had any weight gain since the trauma (insulin and blood sugar regulation)? Has your libido changed from what is normal for you (testosterone)? Do you awaken with hot flashes or have episodes of sweating since the accident (cortisol, estrogen)? Are you more fatigued than seems normal? Do you have difficulty performing or recovering from exercise? Are you depressed for no apparent reason (growth hormone)?
• Imaging: Unless the patient has severe symptoms or meets the criteria that require a CT scan acutely it is not necessary to order routine diagnostic imaging. MRI, PET and SPECT scanning are more revealing in chronic mTBI and the practitioner is encouraged to find a neurologist specializing in brain injuries as a referral resource.
Treating concussion – the concussion protocols
• The patient must be hydrated to benefit from microcurrent treatment.
• Hydrated means 1 to 2 quarts of water consumed in the 2 to 4 hours preceding treatment.
• Athletes and patients with more muscle mass seem to need more water than the average patient.
• The elderly tend to be chronically dehydrated and may need to hydrate for several days prior to treatment in addition to the water consumed on the day of treatment.
• DO NOT accept the statement, “I drink lots of water”.
• ASK “How much water, and in what form, did you drink today before you came in?”.
• Coffee, caffeinated tea, carbonated cola beverages do not count as water.
Frequencies
Channel A/condition frequencies
| 970 / | |
| 94 / | |
| 321 / | |
| 9 / | |
| 40 / | |
| 284 / | |
| 81 / | |
| 49 / | |
| 18 / 62 | |
| 51 / | |
| 3 / | |
| 91 / | |
| 19, 43, 46 |
A / B Pairs
6.8 / 38
• Remove or reset constitutional factors.
• 6.8 / 38 is an A/B pair in which channel A is not a condition and channel B is not a tissue. The desired effect is created by the two frequencies delivered simultaneously in an interferential field. This frequency combination appears to neutralize all of the genetic factors described by Van Gelder and the physicians of the early 1900s and generally makes people feel more grounded and steadier.
35 / 102
• / 102 was the frequency on Van Gelder’s list for the pineal gland which secretes melatonin and regulates sleep wake diurnal cycles. Melatonin is a powerful antioxidant and has some anti-tumorgenic activity in preventing breast cancer and other cancers. In Van Gelder’s understanding, this frequency also resonated with the energy center at the top of the head known as the “crown center” when combined with 35 / on channel A. If the practitioner’s belief system does not include the concept of energy centers, then the frequency can be used with the intention to simply address the physical structures. This frequency combination usually makes patients feel lighter and more relaxed. The affect of the frequency combination and the outcomes achieved do not appear to be affected by the practitioner’s belief system.
Channel / B tissue frequencies
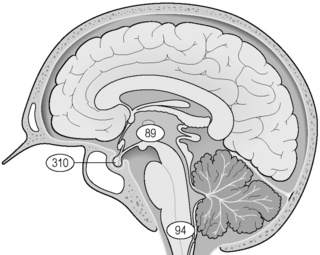
Midbrain: ___ / 89
• The “midbrain” is part of the mesencephalon and includes the tectum, the pretectum, the inferior and superior colliculi, the cerebral peduncle, the midbrain dorsal and ventral tegmental areas, the crus cerebri, the substantia nigra, and the cerebral aqueduct and may also include third ventricle, thalamus, hypothalamus, subthalamus, subcortical system, the amygdala (limbic system), hippocampus (limbic system). For the purposes of this chapter it has been found to successfully treat central pain and is assumed to address the thalamus and periventricular, responsible for central pain.
Solar plexus: ___ /200
• The solar plexus is an archaic term for the celiac nerve plexus of the vagus nerve just below the sternum in the epigastric area of the abdomen. This frequency is thought to address both the nerve plexus and the energy center located in this area. If your belief system does not include the concept of energy centers then the protocols can be used simply to address the physical structures. The frequencies used and outcomes achieved will not change.
General concussion protocol
Channel A condition / Channel B tissue
94 / 200 – Nervous tension
• Literally translated this frequency removes “trauma” from the solar plexus but Van Gelder used it to reduce nervous tension. It is observed to have a calming effect and to begin increasing serotonin levels.
• Treatment time: Use this frequency for at least 1–2 minutes depending on clinic time demands and the patient’s condition. If the patient is very tense and time allows this frequency may be used for up to 5 or 10 minutes.
970 / 200 – Emotional tension
• Literally translated this frequency combination balances the emotional component or removes emotional stress from the “solar plexus” and Van Gelder described it as reducing emotional tension. It is observed to have a calming effect and begins increasing serotonin levels.
• Treatment time: Use this frequency for at least 1–2 minutes depending on clinic time demands and the patient’s condition. If the patient is very tense and time allows this frequency may be used for up to 5 or 10 minutes.
94 / 94
• Remove concussion from the medulla.
• If the memory of some recent trauma is replayed in slow motion in the mind’s eye it will become apparent that there are two parts to any trauma. The first is the pain of the physical injury. The second is the “fact” of the trauma and the surprise or shock to the system that it represents. It is the “fact” of trauma and the shock to the system that is thought to be removed by using 94 /.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree