Fig. 1.1
Prototypical trajectories of distress
Resilience tends to be the most frequent response to trauma exposure. Individuals in the resilient category may experience some transient stress reactions in the form of anxiety or sleep disturbance but experience little to no disruption in day-to-day function (Bonanno, 2004) . Recovery pertains to moderate-to-severe symptoms of posttraumatic stress that gradually decrease over the course of time. This is evidenced by the finding that nearly half of all cases of PTSD resolve in approximately 3 months following diagnosis (American Psychiatric Association, 2013). Chronic stress is marked by severe levels of PTSD symptoms that remain high and cause significant disruption in function and quality of life. Delayed onset of PTSD is marked by moderate symptoms that increase over time. With regard to total prevalence, delayed onset PTSD is relatively uncommon with few meeting criteria beginning 6 months post trauma, and even fewer reporting an onset 1 year following the trauma.
Although resilience often emerges as a common response to trauma, evidence suggests that patterns of distress vary across context. Patterns of chronic distress are particularly common in the presence of risk factor caravan passageways. In the case of citizens of the Palestinian Authority where repeated exposure to political violence is high, and access to valued resources is more limited, the modal response to trauma is trajectory of moderate distress that recovers over time (Hobfoll, Mancini, Hall, Canetti, & Bonnano, 2011) . In this context, individuals who fared better tended to have less exposure to political violence and loss.
Long-Term Correlates of Trauma
Although the general trajectory of trauma is that of recovery, evidence suggests that the impacts of varied traumas may persist throughout the lifetime (Layne et al., 2014; Polusny & Follette, 1995) , particularly when losses are not recoupable as in the case of physical disability, geographical displacement, and the death of loved ones. Survivors of the Jewish Holocaust following exposure to torture, death of immediate family, isolation, and other traumatic loss experienced high rates of PTSD and had continued heightened sensitivity to loss and trauma 58 years following the end of World War II (Dekel & Hobfoll, 2007; see also Chap. 23, this volume) . The long-term impacts of trauma have also been demonstrated in World War II and Korean War veterans. Approximately 50 years post war, over one third reported significant war-related stress (Hunt & Robbins, 2001) . These symptoms are explained in part by the long-term impacts of war-related injury (i.e., a risk factor caravan of disability and daily trauma reminders) and illness along with ongoing intrusion and avoidance symptoms.
The long-term impacts of trauma are also evident among survivors of childhood sexual abuse who experience increased risk of anxiety, borderline personality disorder, and other negative psychological outcomes in adulthood (Hillberg, Hamilton-Giachritsis, & Dixon, 2011) . Risk factor caravans are especially salient in the co-occurrence of childhood abuse, as sexual and physical abuses are frequently accompanied by psychological maltreatment that further impacts adjustment and well-being (Spinazzola et al., 2014) . The detrimental effects of childhood abuse are multiplicative such that psychological maltreatment may amplify the effects of co-occurring abuse and trauma.
Less is known about the long-term impacts of isolated mass trauma. Consistent with the resilience literature, many acute psychological symptoms resolve for many individuals in the aftermath of mass trauma, but risk for substance abuse, physical distress, and greater medical utilization may remain elevated (Galea, 2007).
Impact on Physical Health and Morbidity
Whereas the presentation of traumatic stress in the form of PTSD and related symptoms is salient, research conducted in the field of health psychology continues to reveal the insidious impacts of trauma on long-term physical health and functional status (see Chap. 9, this volume). PTSD is significantly associated with an array of debilitating physical conditions such as pain and cardiovascular disease (Galea, 2007; McFarlane, 2010; Taylor-Clift et al. 2015). Moreover, PTSD is associated with cardiovascular-related mortality and all-cause mortality (Boscarino, 2006, 2008) .
There are a number of biobehavioral mechanisms that may explain the associations between trauma, PTSD, and physical morbidity. Chronic inflammation and risky health behaviors are two particularly plausible passageways that may explain the associations between trauma and disease. Inflammatory markers including C-reactive protein (CRP) are elevated among individuals exposed to a host of traumatic stressors including interpersonal violence (Heath et al., 2013) and terrorism (Canetti, Russ, Luborsky, Gerhart, & Hobfoll, 2014) . Trauma and PTSD may also indirectly impact health status through behavioral mechanisms such as smoking, overeating, sedentary behavior, and poor medical compliance (see Chap. 9, this volume, for related discussion). To some extent, these behaviors may function to assuage psychological distress at the cost of long-term health (Weiss, Tull, Viana, Anestis, & Gratz, 2012) .
Untangling the Web: Trauma Types, Risk Factors, and Mechanisms
The heterogeneity in reactions to trauma begs the question of why some individuals decompensate in the face of traumatic stress , when many remain resilient. From the perspective of COR theory , these differences can be explained by the complete field of resource and risk factor caravan passageways (Hobfoll, 2004; Hobfoll et al., 2009; Layne et al., 2014) . Figure 1.2 depicts the multilevel model of trauma and resource loss. As can be seen, trauma impacts intrapersonal, interpersonal, and community resources (one-way arrows), and the negative impacts of trauma may spiral across levels (two-way arrows). Although individuals and social structures are highly motivated to preserve and enhance resources through resource caravan passageways of education, financial planning, and social engagement, traumatic stress may engender multiple cycles of resource loss. Thus, some of what is called resilience is actually a reflection of the fact that the degree of personal, social, and material loss is different for different people experiencing a trauma, and what is misconstrued as more “resilient” in many cases may rather be a reflection of experience less of the trauma burden. Further, the available of external resources is not uniform. Some have more family and availability of government and emergency aid. Some circumstances may limit access to that external aid, and some environments are themselves too resource poor to provide more than a minimum of aid.
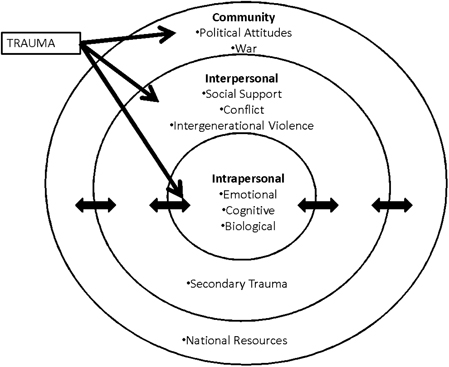
Fig. 1.2
Multilevel model of trauma and resource loss
The Nature of the Trauma
Adverse reactions to trauma are linked to the type, severity and chronicity of the initiating traumatic events (Brewin, Andrews, & Valentine, 2000). In the aftermath of trauma, individuals who reported higher levels of PTSD symptoms tend to have experienced more severe and chronic trauma exposure (Brewin et al., 2000; Hobfoll et al., 2009) . Individuals directly exposed versus witness to trauma and individuals closer in proximity to the trauma may be at increased risk for PTSD and related symptoms, because the level of objective threat is higher. Individuals exposed to the repetitive nature of combat trauma tend to report more adverse outcomes compared to individuals exposed to more isolated incidents of civilian terrorism and work-related accidents (Amir, Kaplan, & Kotler, 1996) . Ongoing warfare and natural disasters have the potential to initiate larger cycles of loss, because individuals and communities may be directly traumatized and also experience ongoing losses of key resources (Hobfoll, 2011; see Chap. 12, this volume) .
The timing and frequency of trauma are also linked to the development of PTSD symptoms. Individuals exposed to interpersonal trauma early in life tend to experience greater difficulty with emotion regulation and PTSD symptoms compared to those with trauma that occurs less frequently and later in life (Ehring & Quack, 2010) . In addition to adding to the total number of traumas likely to accumulate over the lifetime, trauma has been shown to have compounding effects with regard to sensitization and kindling (McFarlane, 2010) . With repeated exposure, individuals may become primed to be increasingly psychologically and physiologically reactive to stressful and traumatic events in the environment so that each additional trauma magnifies the risk of adverse psychological and physical reactions (McFarlane, 2010) .
The Intrapersonal Context of Trauma
Individuals’ personal characteristics may afford important coping resources for facing adversity and trauma and remaining engaged in their environment (Hobfoll & Lilly, 1993) . Engagement refers to the individual’s personal affective-motivational reserves of energy (vigor), commitment (dedication), and excitement (absorption) needed to maintain activities of living (Hobfoll, 2011; Schaufeli, Salanova, González-Romá, & Bakker, 2002) . The physical, cognitive, and emotional energy underlying engagement is often inherently valued in its own right and facilitates the ongoing development of resources in occupation and social settings (Armon, Melamed, & Shirom, 2012; Hobfoll, 2011) . Traumatic contexts tend to have punishing effects that drain engagement reserves, and other individual characteristics may potentiate this drain.
Neuroticism is a stable personality trait that refers to an individual’s overall proclivity to experience negative mood and affect in the form of anxiety, worry, anger, and sadness and lends increased sensitivity to trauma (Costa & McCrae, 2008) . To the extent that neurotic individuals are prone to the view the world as threatening, they may also experience greater draining of their vigor and engagement (Armon et al., 2012) and experience vulnerability for emotional disorders in general (Barlow, Sauer-Zavala, Carl, Bullis, & Ellard 2014) . Individuals also differ with regard to the strategies that they utilize to regulate affective distress. Emotion regulation strategies pertain to the efforts to modify or maintain the form, frequency, and impact of emotion (Gross & Thompson, 2007). Difficulties in emotion regulation may arise when individuals are unable or unwilling to identify, accept, and acknowledge negative emotional states and when individuals behave in an impulsive manner to escape uncomfortable emotions (Bond et al., 2011; Gratz & Roemer, 2004) . Experiential avoidance, the tendency to negatively evaluate, suppress, and avoid uncomfortable thought and emotion, has been shown to be a significant mediator in the relationship between neuroticism and PTSD (Goldsmith, Gerhart, Chesney, et al., 2014; Maack, Tull, & Gratz, 2012; Shenk, Putnam, Rausch, Peugh, & Noll, 2014) and may lead to generalized vulnerability to psychopathology and interpersonal problems (Gerhart, Baker, Hoerger, & Ronan, 2014; Goldsmith, Gerhart, Chesney, et al., 2014; Levin et al., 2014; Shenk, Putnam, & Noll, 2014) . Avoidance of trauma reminders may trigger social withdrawal and reduce contact with rewarding events in the external environment which trigger ongoing loss spirals (Carvalho & Hopko, 2011) to the extent that individuals ruminate with peers, and permit smaller problems to escalate (Holahan, Moos, Holahan, Brennan, & Schutte, 2005) .
Other personal characteristics including female gender, lower socioeconomic status, education, age, and intelligence have been linked to higher levels of PTSD following traumatization (Brewin et al., 2000) . To a great extent, factors such as socioeconomic status, education, and intelligence provide pathways to greater access to resources (Hobfoll et al., 2011) . As such, these individuals are less affected by stress and trauma, because they have greater reserves to fall back on. Gender differences may be explained in part by physiological differences, including hypothalamic–pituitary–adrenal (HPA) axis response to trauma (DeSantis et al., 2011) , but these associations may also be mediated by gender norm differences in cognitive appraisal such that females may be more likely to adopt self-blame and develop world views that are more threatening (Tolin & Foa, 2006) . From a life span perspective age and prior development are important for understanding reactions and recovery from trauma. Older adults may be more physically vulnerable to trauma and have fewer instrumental resources needed to recuperate from loss (Sharkey, 2007).
The Interpersonal Context
Although constructs such as neuroticism, emotion regulation, and trauma cognitions are situated within the individual, they occur in response to a much broader ecological context. Exposure to childhood trauma is significantly associated with neuroticism assessed in adulthood (Roy, 2002) . Self-efficacy tends to be positively associated with social support (Hobfoll, 2011; Karademas, 2006) , children’s self-talk increasingly tracks family, and peer assessments of their competence over the course of development (Cole, Jacquez, & Maschman, 2001) , and caregivers play important roles in shaping emotion regulation and social skills (Eisenberg, Fabes, & Murphy, 1996) . These deficits in cognitive and emotion regulation are often part of a larger constellation of risk factors that include abuse and a lack of nurturing interactions (Fruzzetti, Shenk, & Hoffman, 2005; Stevens et al., 2013) . As such, subjective psychological events within the individual are often reciprocally intertwined with their social ecology.
The social context of trauma plays a crucial role in adjustment in the aftermath of trauma as the family system or local community is often the primary vehicle for the consolidation and protection of resources through the provision of emotional support, love, and validation needed to process difficult emotion, along with instrumental and financial supports needed to navigate the world (Hobfoll, 2011; Hobfoll & Vaux, 1993) . Inversely, problems and deficits in these areas can lead to significant distress and maladjustment (Brewin et al., 2000; Hobfoll, 1989; Layne et al., 2014; Stevens et al., 2013) . These social resources are complex, dynamic, and impact posttrauma adjustment through multiple social-cognitive mechanisms (Benight & Bandura, 2004; see Chap. 11, this volume) . As noted earlier, even subjective reactions to trauma and stress may have been directly and indirectly shaped within the family system (Hobfoll, 2011).
The ability to form secure and stable attachments affords a sense of stability and safety in the face of environmental adversity (Bowlby, 1969) . The tendency to identify with and attach to others in early life has played a crucial role in survival throughout much of human history. Secure attachments enable the developing individual to acquire strategies for seeking and providing help, internalize adaptive coping strategies, and develop realistic expectations about supportive relationships (Mikulincer, Shaver, & Pereg, 2003) . Whereas caregivers may share a proclivity to positive cognitions through their communication (Donnelly, Renk, Sims, & Mcquire, 2011) , they may also pass on a proclivity to shame and negative self-evaluation through negativistic parenting styles (Alessandri & Lewis, 1993; Mills et al. 2007) . When exposed to trauma, individuals with less secure attachment styles (i.e., anxiety and avoidance) tend to report higher levels of perceived stress, and in turn experience higher levels of PTSD symptoms (Besser, Neria, & Haynes, 2009) . Attachment anxiety is also linked to poorer perceived social support in the aftermath of trauma (Besser & Neria, 2010) .
The concept of social support is broadly defined as relationships and other interpersonal interchanges that provide a sense of connection to others and provide help and assistance to the individual (Hobfoll & Stokes, 1988). Thus, social support includes close attachments and other helpful relationships. Poor positive social support is consistently linked with poor adjustment in the aftermath of trauma (Brewin et al., 2000) . This may be so as the traumatized individual has less access to emotional support in the form of validation and encouragement, less instrumental support in the form of physical assistance, and less access to models of positive coping strategies (Benight & Bandura, 2004; Hobfoll, 2004) . Although the previous examples are of positive social support, negative social support in the form of criticism, hostility, and judgment may provoke additional distress that outweighs the benefit of positive support (Hobfoll, 2004). Whereas social resources are sometimes mistakenly conceptualized as a static buffer against PTSD and related distress, social support interacts dynamically with symptoms and other resources, such that support may be eroded over time (Hobfoll & Stokes, 1988). In some instances, PTSD symptoms, depression, and poorly regulated anger may overwhelm supportive others and reduce the likelihood of helpful interactions (Gerhart, Sanchez Varela, Burns, Hobfoll, & Fung, 2014; Gerhart et al., 2014; Lane & Hobfoll, 1992) . Risk factor caravans are exemplified among individuals who are exposed to ongoing trauma, have limited social and financial resources, lack the ability to permanently escape the threatening family, home, or neighborhood environment, and as a result remain at high risk for ongoing interpersonal violence (Fleury, Sullivan, & Bybee, 2000; Stevens et al., 2013) . These escalating cycles of violence and re-traumatization may reinforce and lead to trajectories of chronic posttraumatic stress and contribute to health disparities (Layne et al., 2014; Taylor-Clift et al. 2015) .
Aftershocks: Shared Trauma, Intergenerational Violence, and War
Given that trauma occurs within dynamic social systems, there is a potential for consequences of trauma to apply at the group level . These patterns highlight that resources, losses, and PTSD cluster within social systems, and that many traumas may impact the individual and the social system through direct and indirect effects. In these cases, trauma becomes a shared experience that may limit coping resources across the group level (Tosone et al., 2003) . These events highlight the occurrence of trauma as inherently multileveled with the potential for transactions between the individual and group context (Kawachi, Subramanian, & Kim, 2008) .
Shared and Secondary Trauma
Trauma experienced at the group level can produce emergent processes. Shared trauma is a concept from the psychotherapy literature that refers to situations in which the common experience of a trauma (e.g., terrorism, war, natural disaster) among patient and therapist who reside in the same community may alter the work of therapy, as the provider may be more acutely vulnerable to stress and therefore more emotionally reactive to the content and process of psychotherapy (Baum, 2010; Saakvitne, 2002; Tosone, Nuttman-Shwartz, & Stephens, 2012) . In order to provide effective services, the clinician must monitor and address their personal reactions to trauma (Tosone et al., 2012) .
Individuals often turn first to emotional support from friends and family before larger community supports and psychotherapy (Elliott & Pais, 2006) . Although professional training, role boundaries, and support may help offset potential resource losses in the context of therapy (Tosone et al., 2012), loss spirals may persist in less structured social roles and relationships. Coping and adjustment are highly nested within a couple such that an individual’s traumatic stress is positively associated with the traumatic stress of the spouse, and patterns of reciprocal hostility, criticism, and withdrawal may emerge within couples (Dekel & Monson, 2010) . Emotion-focused coping within the dyad may be especially detrimental for both members as it is associated with distress within the individual (Gilbar, Weinberg, & Gil, 2011) . Trauma may also affect group-level processes more indirectly through secondary or vicarious traumatization . In these instances, the trauma is not necessarily shared among individuals, but one may develop posttraumatic reactions through hearing and empathizing with stories of trauma.
Intergenerational violence may also contribute to the spiraling effects of trauma throughout social systems. Growing up in abusive and traumatic environments does not entail a future trajectory of imitating abusive behavior, but there are some small-to-moderate links between witnessing and experiencing violence and abuse and later perpetration of abuse in the family system (Stith et al. 2000). From a social learning perspective, trauma-exposed individuals may learn abusive behaviors from caregivers and other role models in childhood, and mimic these learned behaviors as adults with their spouses and children (Bandura, 1977) . In the case of borderline personality disorder, risk factor caravan passageways may occur through inconsistent parenting practices that vacillate widely between hostility and disengagement (Stepp, Whalen, Pilkonis, Hipwell, & Levine, 2012) .
Impact on Political Attitudes and War
Spirals of resource loss may also occur at the national or cultural level, through cycles of retaliatory violence. In the face of trauma and particularly threat to one’s life, individuals often attempt to manage terror and threat perceptions by strengthening attitudes of support for their own cultural or national group and also becoming more committed to attitudes against their cultural out-groups (Greenberg et al. 1990) . In the areas of chronic conflict (e.g., Israel and the Palestinian Authority; Northern Ireland), direct and indirect exposure to war-related trauma is significantly associated with support for more military action and war (Hayes & McAllister, 2001) . Just as the nature of the trauma has important impacts on traumatic stress reactions, the type of trauma also impacts political attitudes. Chronic war entails repeated traumatization that may shape increasingly hostile political attitudes over time (Hobfoll, Canetti-Nisim, & Johnson, 2006) .
The mechanisms of war and terror-related trauma’s impact on political attitudes are complex, but evidence suggests that these relationships are explained in part by a desire for defensive political measures to escape existential insecurity (Canetti, Halperin, Hobfoll, Shapira, & Hirsch-Hoefler, 2009). In the face of war and trauma, core beliefs about safety and security may be drastically altered (Janoff-Bulman, 1992; Magwaza, 1999) . As a result, individuals are primed to be vigilant for ongoing threats and increasing their support for violent military action (Bonanno & Jost, 2006) . Conflict may escalate rapidly as opposing groups and nations participate in cycles of retaliation (Haushofer, Biletzki, & Kanwisher, 2010) . Addressing the impact of chronic war and terror-related trauma on political process may be crucial for healing long-standing conflict (Canetti, Hall, Greene, Kane, & Hobfoll, 2014) .
Summary
This chapter introduced the topic of traumatic stress and its long-term impacts within the context of COR theory (Hobfoll, 1989, 2004). This ecological and developmental perspective of trauma highlights that traumatic stress from the initial horror to its long-term fallouts is dynamic and multileveled. The concept of risk factor caravans is introduced to highlight the nesting and statistical covariation of risk factors and trauma sequelae within individuals and social groups. Although individuals demonstrate considerable resilience in the face of adversity, traumatic stress has the power to disrupt emotional and social lives through ongoing spirals of loss. Paradoxically, individuals in an effort to avoid and compensate for traumatic losses may inadvertently contribute to ongoing cycles of traumatization.
References
Alessandri, S. M., & Lewis, M. (1993). Parental evaluation and its relation to shame and pride in young children. Sex Roles, 29(5–6), 335–343.CrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




