Trauma Procedures in the Emergency Department
Rahim Valani MD, CCFP-EM, FRCPC, PG Dip Med Ed
Immediate and urgent vascular access when intravenous (IV) access has failed.
Can be used for any age.
Safe to administer fluids, drugs, and blood products.
IO needle can be left in place for up to 72 hours, but is generally not recommended.
Used as a temporizing measure until peripheral venous access is obtained.
Indications
Need for immediate access when IV access has failed.
Relative Contraindications
Avoid IO in a fractured limb.
Overlying infection.
Previous attempt at the same site.
Osteogenesis imperfecta or other medical conditions that are prone to fractures with minor trauma.
Complications
Improper placement of needle into subcutaneous or subperiosteal tissue (extravasation of fluid) or poor landmarks.
Bending of needle.
Through and through penetration of bone.
Infection—cellulitis, osteomyelitis.
Compartment syndrome.
Growth plate injuries.
Local hematoma.
Procedure
Use 14 to 20 G intraosseous needle with stylus.
Prepare the area in a sterile fashion and infiltrate with local anesthetic.
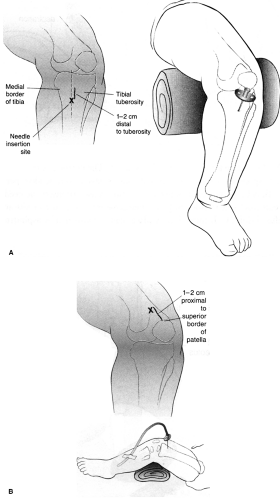
Landmark as illustrated for proximal tibial or distal femur placement (Fig. 21-1).
Needle is inserted at 90 degrees to the bony surface.
Avoid putting your other hand behind the limb where the IO needle is being inserted.
Proper location will ensure that the needle is away from growth plate.
Placement is confirmed when the cortex is infiltrated—you will feel a release (Fig. 21-2).
You may aspirate marrow, but this is not always possible or necessary.
Connect to IV tubing and infuse fluids.
Watch for signs of fluid extravasation.
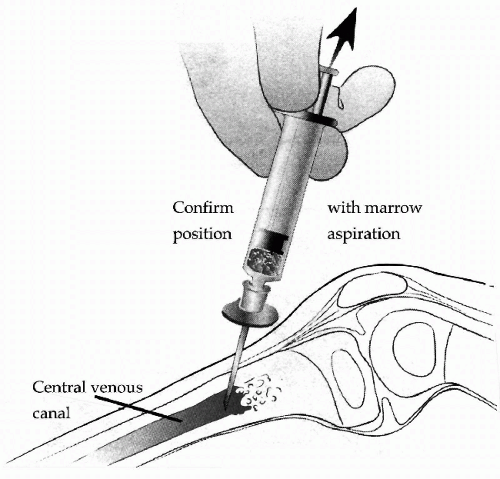 FIGURE 21-2 • Insertion of intraosseous needle. (From King C, Henretig FM. Intraosseous infusion. Pocket atlas of pediatric emergency procedures. Philadelphia: Lippincott Williams & Wilkins; 2000, Fig. 9.2C, with permission.) |
Sites for central venous line placement: femoral or subclavian (Table 21-1).
Indications
Need for central venous pressure monitoring.
Large volume infusions.
Drug infusions requiring central access such as epinephrine and norepinephrine.
Infusion of concentrated or peripherally sclerosing agents (>40 mEq/L of KCl, hypertonic saline).
Emergency dialysis.
Contraindications
Bleeding diathesis or coagulopathy.
Distorted local anatomy.
Proximal injury (e.g., avoid femoral line in pelvic fracture).
Prior injury to the vesse.
Complication rates of central line placements range from 0.3% to 18.8%.
Ultrasound guided insertion is gaining popularity, and potentially may decrease complications.
Complications
Bleeding.
Thrombosis.
Arterial puncture.
Air embolism.
Hemothorax.
Pneumothorax.
Systemic infection.
Hematoma.
Cellulitis.
TABLE 21-1 Sites for Central Venous Line Placement | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Procedure
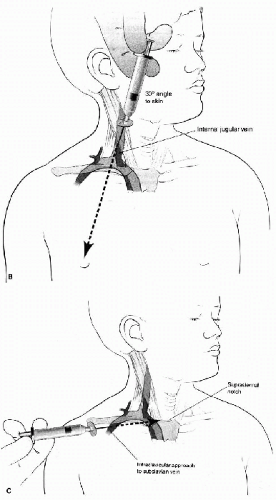
See Figure 21-3 for landmarks.
Prepare and drape the area in a sterile fashion.
Consider using a “finder needle” to locate the vein.
Infiltrate area with local anesthetic.
Seldinger technique (Fig. 21-4):
Use a 5-mL syringe connected to the entry needle.
Use specified landmarks for the central vein being cannulated (Fig. 21-3).
Insert needle while continuously drawing back. A rapid draw suggests the vessel is accessed.
Can confirm venous placement versus arterial with:
Rapid blood gas analysis.
Lack of pulsatile flow.
Transduce with short segment of IV tubing.
Color of blood is not a reliable marker.
Once vessel is accessed, remove syringe while stabilizing needle and insert guidewire. It should thread in easily.
If guidewire not threading easily, reconnect syringe and ensure the needle tip is positioned in the vessel.
Remove needle while leaving guide wire in place.
DO NOT LET GO OF THE GUIDEWIRE!
Place selected catheter over guidewire, and remove guidewire.
Secure central line.
Obtain chest x-ray for subclavian line to ensure no pneumothorax, correct placement, and location of catheter tip.
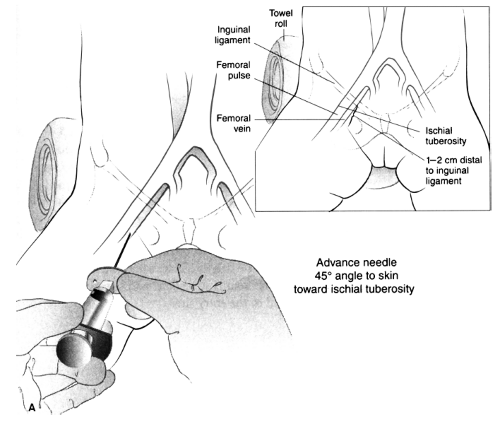 FIGURE 21-3 • Landmarks for central line placement. A. Femoral site. B. Internal Jugular Site C. Subclavian Vein (From King C, Henretig FM. Central Venous Access. Pocket atlas of pediatric emergency procedures. Philadelphia: Lippincott Williams & Wilkins; 2000, Figs. 7.2, 7.3, and 7.4, with permission.) |
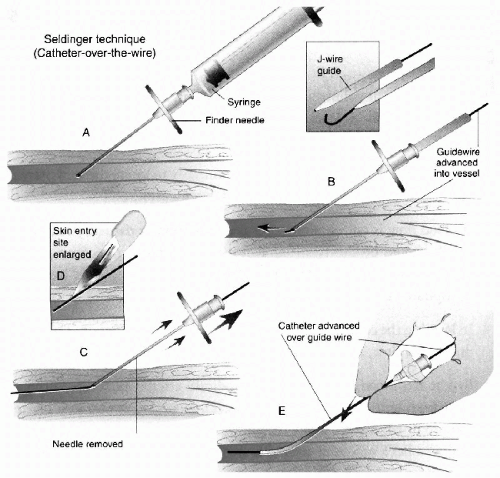 FIGURE 21-4 • Seldinger technique for insertion of central venous line over guidewire. (From King C, Henretig FM. Central venous access. Pocket atlas of pediatric emergency procedures. Philadelphia: Lippincott Williams & Wilkins; 2000, Fig. 7.1, with permission.) |
Various kits are available that aid in the Seldinger technique.
Potential sites include:
Radial (most common site).
Ulnar.
Posterior tibial.
Femoral.
Indications
Continuous monitoring of hemodynamic parameters (blood pressure and heart rate).
Frequent need for blood sampling and arterial gas sampling.
Contraindications
Hand—absence of collateral circulation. All other sites, absence of pulse.
Can cause compromise of circulation and distal ischemia.
Prior surgery over the site.
Bleeding diathesis.
Complications
Arterial spasm.
Poor waveform.
Ischemic limb/digits.
Aneurysm.
Infection.
Procedure
Palpate artery over area of maximal impulse.
Prep the area in a sterile fashion.
Insert the needle at a 10- to 20-degree angle to the skin surface.
Blood will appear in the catheter hub when the artery is punctured.
Advance the catheter slowly until the angle to the skin surface is 10 degrees.
Advance the catheter over needle into the artery.
Remove the needle while compressing the artery proximal to the tip of the catheter.
Connect the catheter to the arterial line system.
Zero the system.
Assess the waveform.
Secure the catheter.
Use heparinized solution only.