(1)
Trauma and Critical Care, R Adams Cowley Shock Trauma Center, Baltimore, MD, USA
Keywords
TracheaBronchusEsophagusTracheobronchialPenetrating injuryBlunt injuryNational Trauma Data BankInjury severity score (ISS)BronchoscopyAirway pressure release ventilation (APRV)Collar incisionThoracotomyEsophagoscopyContrast-enhanced esophagographyIntroduction to the Problem
Injuries to the tracheobronchial tree and esophagus are relatively rare in even the busiest urban trauma centers. They most commonly occur in the neck, as the thoracic cage provides protection in the chest. Injuries in the neck tend to lend themselves to easier diagnosis, whereas those contained within the thorax may elude diagnosis for prolonged periods of time and lead to adverse outcome.
Tracheobronchial
Because many patients with tracheobronchial injury expire before arrival to the hospital, the true incidence of the injury burden remains unknown [1]. Several autopsy studies estimate the incidence to be approximately 3 % [2, 3]. Prompt recognition and management of tracheobronchial injury remains paramount because of the physiologic impact that such injuries can cause. Compromise of the major airways can restrict oxygenation and ventilation and thus lead to physiologic collapse. Any sign of major airway injury should lead the trauma team to rapidly search for the anatomic lesion and initiate treatment.
Blunt injuries to the trachea and bronchus are believed to occur as direct impact to the neck, deceleration injuries suffered at fixed anatomic locations (carina and cricoid), or increased pressure within the tracheobronchial tree from blunt force applied to the thorax or abdomen. Blunt injury to the thoracic trachea most commonly occurs within 1 cm of the carina. Due to the high degree of energy necessary to injure tracheobronchial structures, these injuries are typically only a small part of a larger injury burden.
Penetrating injuries to the trachea in the neck are often the result of stab wounds (Fig. 8.1). Stab wounds are typically lower energy and are frequently associated with vascular and esophageal injuries. Attention to exsanguinating vascular injury takes priority in a patient with a stable or protected airway. Penetrating injury to the trachea and bronchus within the thorax is typically due to gunshot wounds and may be associated with cardiac, pulmonary, major vascular, or esophageal injury. Iatrogenic penetrating injury may also occur during invasive tests, tracheostomy, and orotracheal intubation.


Fig. 8.1
External injuries after stab wound to neck.
Esophagus
Penetrating injury is the predominant cause of esophageal trauma. In a recent series, 26 patients with esophageal trauma were identified over a 15-year time period. Twenty-two of those were penetrating and four blunt, with all blunt injuries occurring in the region of the cervical esophagus [4]. Blunt injuries to the esophagus remain are rare and are often associated with concomitant thoracic injury. Blunt injury occurs as a result of direct force to the cervical esophagus in conjunction with a hyperextended neck, or rarely as result of intraluminal distention secondary to blunt force trauma [5].
A 2013 review of the National Trauma Data Bank sought to better describe the current state of penetrating esophageal injury in the United States. Over a 2-year time period, 227 patients with penetrating injuries to the esophagus were treated at either level I or level II trauma centers. The overall mortality was 44 % and the overwhelming majority of deaths occurred within 24-h. Deaths occurring in the initial 24-h period were the result of concomitant injury, not the esophageal injury alone. In patients surviving greater than 24-h; 62 % had primary repair, 13 % underwent drainage, and 4 % underwent resection. The only predictor of death, in those surviving greater than 24-h, was injury severity score (ISS) [6].
Iatrogenic injury remains the leading cause of penetrating esophageal injury [7]. Nasogastric tube insertion, trans-esophageal echocardiography, flexible and rigid esophagoscopy and various procedures are all potential injurious agents. Therapeutic dilation of the esophagus for various strictures and achalasia remains the predominant cause of iatrogenic esophageal perforation [8].
History of Care
Given the rare nature of tracheobronchial and esophageal injuries, the majority of discussion consists of case reports and single-institution series. Thus, the principles of treatment remain the same and have not changed in the past 50 years. Diagnostic adjuncts have continued to improve and assist in earlier identification of tracheobronchial and esophageal injury, which may allow more timely surgical intervention.
Tracheobronchial
Kiser and colleagues performed a meta-analysis of the literature from 1873 to 1996, looking specifically at blunt intra-thoracic tracheobronchial injuries. They identified 256 injuries, of which 59 % were the result of motor-vehicle collisions and 27 % were the result of crush injury. The median time to diagnosis was 9-days with 47 % of cases involving the right bronchus and 32 % involving the left bronchus (52 % of patients with right bronchial injuries and 14 % with left sided bronchial injuries were diagnosed within 24-h) [9].
Investigators at the Ratchaburi Hospital in Thailand reported on 11 tracheobronchial injuries in 10 years (7 penetrating and 4 blunt). Pneumothorax was present in two patients, subcutaneous emphysema was present in three patients, and dyspnea was in four. The authors concluded that a delay in diagnosis was the leading factor resulting in increased morbidity [10]. Similarly, Cassada et al., found that a delay in diagnosis was the single most important factor leading to poor outcome [11].
Esophagus
As diagnostic modalities have advanced, the identification of injury to the esophagus has become easier to accomplish in an expeditious and noninvasive manner. A 1977 report from the Journal of Trauma describes the case of a young man status-post motorcycle collision with multiple injuries, which on the fourth day of his hospitalization manifested with mediastinitis and empyema. Surgical exploration revealed the presence of an esophageal perforation, which was successfully treated with drainage [12]. In the current era of enhanced imaging techniques and the wide availability of invasive procedures for diagnosis, clinicians are able to more quickly recognize and intervene with such lesions.
The management of esophageal injury has remained largely unchanged for the past five decades. Some have sought to define the role of endoscopic stenting in esophageal perforation, finding a greater risk of death with stenting than with surgery [13]. This led the authors to conclude that operative therapy is preferred. Thus, the primary goals of treatment remain: primary repair, wide drainage, and possible diversion if anatomic repair is impossible or physiology is exceedingly altered [14].
Technique with Personal Tips
Attention to maintenance of the airway, breathing, and circulation is mandatory. Exsanguinating injuries must be rapidly identified and treated and neurologic insults must be addressed expeditiously. Tracheobronchial and esophageal injuries should be addressed next.
Tracheobronchial
Clinical examination can lead the astute physician to suspect injury based on physical findings. Stridor, subcutaneous emphysema, pneumothorax with air leak, and bubbling from epidermal lacerations should increase suspicion of major airway injury.
An adequate airway is essential. A 1999 series from The University of Tennessee Medical Center at Knoxville showed 55 % of patients with tracheobronchial injury were stable on supplemental oxygen alone and did not require urgent intubation [11]. Great caution must be exercised as partial or complete transection of proximal airways can make the procedure difficult or impossible, leading to adverse outcomes. Liberal usage of laryngoscopy and fiberoptic bronchoscopy in this situation will ensure good visualization and assist with placement of a secure airway.
If transection of the trachea occurs in the neck, one may see two visible lumens. In this instance, intubation of the distal lumen with any available endotracheal tube or devise is wise (Fig. 8.2). A surgical airway remains an option in the unstable patient or in patient’s unable to be successfully intubated. After ensuring temporary airway, definitive airway management can be established when the patient is stable.
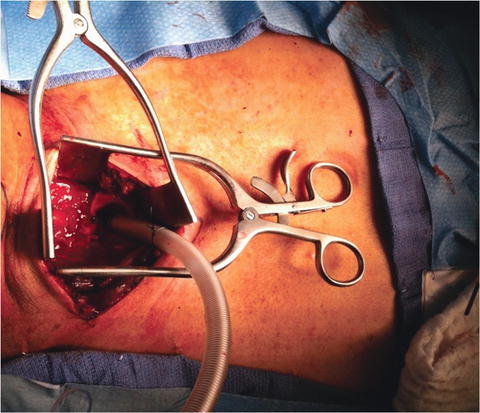
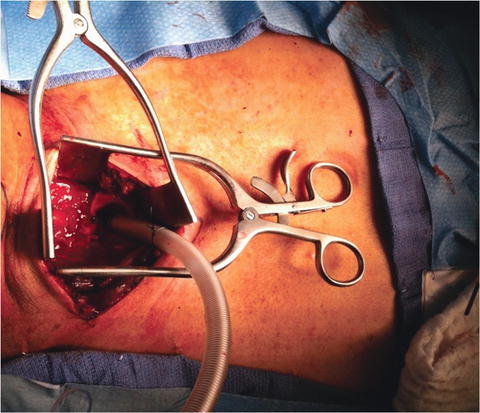
Fig. 8.2
Placement of tubing into distal trachea to facilitate ventilation and oxygenation.
Bronchoscopy and direct visualization of a mucosal defect remain the optimal study for diagnosis of tracheobronchial injury (Fig. 8.3). If bronchoscopy is performed under general endotracheal anesthesia, the clinician must withdraw the endotracheal tube over the bronchoscope to visualize the entirety of the proximal trachea. Bronchoscopy can be performed in either a trauma resuscitation area or an operating room; however, the operating room gives the surgeon the option of additional adjunctive measures as deemed necessary, including operative therapy. Distance from the incisors should be recorded, along with proximity to the carina.
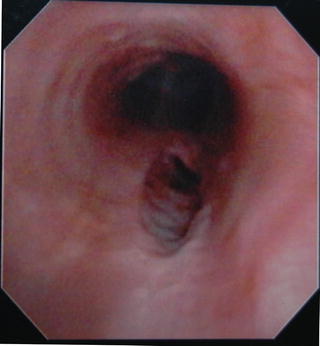
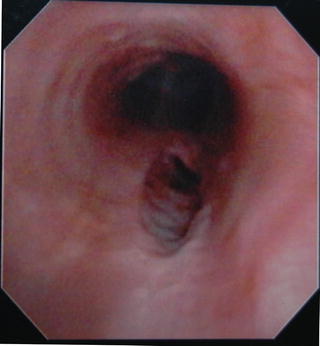
Fig. 8.3
Bronchoscopic view of mucosal injury to trachea.
In the patient with major airway injury that requires mechanical ventilation, decreased pressures will lessen the air leak and assist in oxygenation and ventilation. Airway pressure release ventilation (APRV) is a mode of ventilation frequently employed, which allows the patient to comfortably breathe and avoid dis-synchrony with the ventilator. Maintaining the lowest possible pressures to maintain oxygenation is wise.
CT imaging can be utilized as an adjunct to evaluate for tracheal injury [15] (Fig. 8.4). CT imaging of the neck offers the advantage of evaluating the vasculature and esophagus, in addition to the central airways. In a retrospective review, Chen et al. found CT to be 85 % sensitive in identification of tracheal injury, and the authors concluded that CT can aid in selecting patients that require bronchoscopy for definitive diagnosis [16]. In penetrating injury, the added advantage of assessing trajectory and determining structures at risk of injury makes axial imaging attractive [17]. In the rare case of suspected tracheal transection after blunt injury, axial imaging in a stable patient with CT may be an adjunct to direct visualization with bronchoscopy [18].
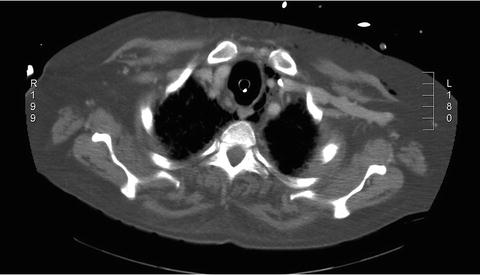
Fig. 8.4
CT showing extra-luminal air and tracheal mucosal abnormality suggesting tracheal injury.
Nonoperative approaches to tracheobronchial injury have been described [19, 20], but operative therapy remains the preferred method of definitive treatment. Initial operative management of tracheobronchial injuries begins with appropriate setup of the operating room and operating equipment. A sternal saw, vascular instruments, and a variety of endotracheal and tracheostomy tubes should be available. Fiberoptic bronchoscopy and appropriately trained anesthesia providers are mandatory. The surgeon should be prepared to perform intra-operative bronchoscopy to assist in identification of the injury. A double-lumen endotracheal tube may be required if single-lung ventilation is desired for a thoracic approach to a bronchial injury.
Cervical injuries involving the trachea are most easily approached via a collar incision performed in approximately 2-fingerbreadths above the sternal notch. This incision is carried down through the platysma and sub-platysmal flaps are created. The strap muscles are divided in the midline. The thyroid isthmus can then be retracted cephalad to further increase exposure of the trachea as it enters the mediastinum. Alternatively, the thyroid isthmus can be divided. If the injury extends into the mediastinum, a partial sternal split can be performed without performing a full sternotomy (Fig. 8.5). In the face of a concomitant vascular or esophageal injury, the collar incision can be extended superiorly or inferiorly in the plane anterior to the sternocleidomastoid muscle.
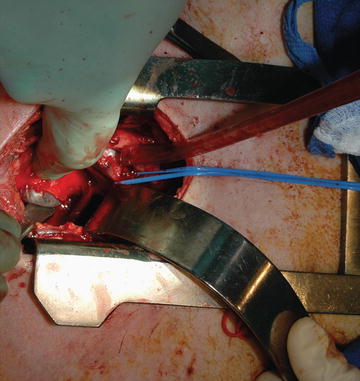
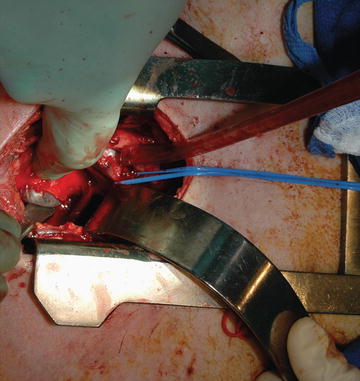
Fig. 8.5
Partial sternal split for evaluation of tracheal injury. The endotracheal tube balloon is visualized emanating from the injury.
The thoracic trachea, right mainstem bronchus, and proximal left mainstem bronchus are best approached via a right posterolateral thoracotomy performed through the fourth intercostal space (Fig. 8.6). Distal left mainstem bronchus injuries are best approached via a left posterolateral thoracotomy. Though lateral decubitus positioning provides optimal exposure of the intra-thoracic tracheobronchial structures, the surgeon must recognize that access to other body cavities is exceedingly limited.
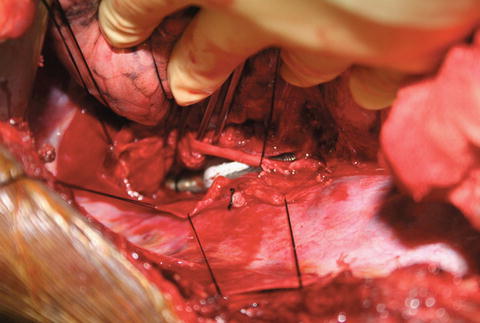
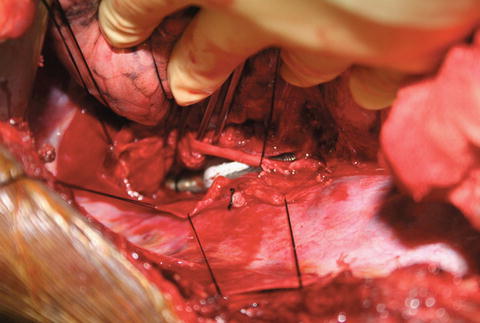
Fig. 8.6
Right posterolateral thoracotomy with mediastinal pleura opened and retracted with silk sutures. The endotracheal tube is seen within the lumen of the injured trachea. The lung is retracted upwards.
Primary repair of tracheal injury is desirable if possible. A single layer of absorbable, monofilament suture is utilized to primarily repair the injury. Running or interrupted sutures can be utilized. Smaller diameter structures are best repaired in an interrupted fashion to avoid narrowing of the airway. Stellate areas should be sharply debrided back to healthy appearing tracheal tissues. Given the mobile nature of the trachea, resection of up to 2–4 cm of trachea with primary anastomosis is feasible (Fig. 8.7) with mobilization. Multiple techniques have been described for tracheal mobilization, including: division of the inferior pulmonary ligament, cervical flexion, and mobilization of the hilum of the lung. If tension is present on the anastomosis after mobilization, the chin can be sutured to the patient’s chest. Mobilization of the trachea should proceed in the anterior and posterior planes as the blood supply comes in laterally. Suture lines are preferably buttressed with autologous and well-vascularized tissue present in the region of repair (intercostal muscle, pleura, pericardial, strap muscle (Fig. 8.8), or omental flaps). Occasionally, the tracheal injury is located only in the posterior membranous portion. Some can be managed nonoperatively. If repair is necessary, they are best approached by opening the trachea anteriorly. The injured trachea is then repaired from the inside. It is necessary to precisely define the level of injury before opening the trachea. This is best done with intraoperative bronchoscopy. The light from the bronchoscope can be seen via the anterior trachea, making the repair as simple as possible. The endotracheal tube must be withdrawn to allow for adequate visualization of the injury. The maneuver may need to be repeated to be sure adequate oxygenation and ventilation is maintained. The anterior trachea is then closed as described above.