CHAPTER 157
Torn/Split Earlobe
Presentation
A patient comes to the emergency department or clinic with an earlobe torn by a sudden pull on an earring. Contributing factors might include previous lengthening of the earlobe hole because of long-term use of relatively heavy or dangling ear jewelry, or the original earring hole may have been placed in an excessively low position.
What To Do:
 Discuss the options: attempting to salvage the original piercing track (which may tend to elongate more easily) or removing the track entirely and providing for a new piercing at a later time. Inform the patient of the possibility of future inclusion cyst formation (caused by any hidden remnants of the old epithelial track) as well as the potential for postoperative scar contracture with resultant notching or scalloping of the lobe.
Discuss the options: attempting to salvage the original piercing track (which may tend to elongate more easily) or removing the track entirely and providing for a new piercing at a later time. Inform the patient of the possibility of future inclusion cyst formation (caused by any hidden remnants of the old epithelial track) as well as the potential for postoperative scar contracture with resultant notching or scalloping of the lobe.
 If cosmetic appearance is of great concern, it may be advisable to consult with a plastic surgeon before attempting the primary repair.
If cosmetic appearance is of great concern, it may be advisable to consult with a plastic surgeon before attempting the primary repair.
 Always perform a thorough evaluation based on the patient’s presentation. If there has been direct trauma to the ear, make sure to perform a thorough evaluation for signs of other clinically significant injuries, including intracranial, facial, and cervical.
Always perform a thorough evaluation based on the patient’s presentation. If there has been direct trauma to the ear, make sure to perform a thorough evaluation for signs of other clinically significant injuries, including intracranial, facial, and cervical.
 Before repair, provide anesthesia, either by infiltrating the lobe with 1% lidocaine (Xylocaine) until the lobe becomes firmer and pale or by performing a block of the greater auricular nerve. The use of anesthetic formulations that contain epinephrine in the ear is somewhat controversial because of the potential for excessive vasoconstriction, although these formulations are advocated by some authors. Once the area is anesthetized, use a No. 11 or No. 15 blade to excise and undermine the wound edges as well as to make any required incisions for a Z-plasty repair.
Before repair, provide anesthesia, either by infiltrating the lobe with 1% lidocaine (Xylocaine) until the lobe becomes firmer and pale or by performing a block of the greater auricular nerve. The use of anesthetic formulations that contain epinephrine in the ear is somewhat controversial because of the potential for excessive vasoconstriction, although these formulations are advocated by some authors. Once the area is anesthetized, use a No. 11 or No. 15 blade to excise and undermine the wound edges as well as to make any required incisions for a Z-plasty repair.
 Tears in the upper two thirds of the lobe may be excised and reapproximated. Tears in the lower third of the lobe should be converted to a full-thickness tear for easier management and better cosmetic results.
Tears in the upper two thirds of the lobe may be excised and reapproximated. Tears in the lower third of the lobe should be converted to a full-thickness tear for easier management and better cosmetic results.
 For repairs that attempt to salvage the original piercing track, excise the wound edges below the old track, including the lower segment of any elongated partial cleft (Figure 157-1, A and B). To encourage wound edge eversion, undermine the anterior and posterior skin edges to 1 mm (Figure 157-2).
For repairs that attempt to salvage the original piercing track, excise the wound edges below the old track, including the lower segment of any elongated partial cleft (Figure 157-1, A and B). To encourage wound edge eversion, undermine the anterior and posterior skin edges to 1 mm (Figure 157-2).
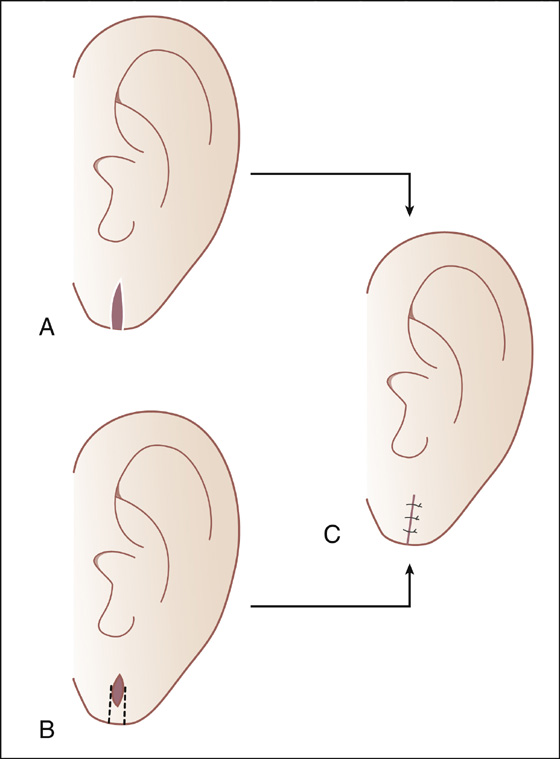
Figure 157-1 A, Incomplete excision of skin lining a full cleft. B, Excision of skin at the inferior lobe margin to convert a partial cleft to a full cleft. Apex epithelium is preserved. C, Straight-line closure of both cleft conditions, with preservation of the original hole. (Adapted from Watson D: Torn earlobe repair. Otolaryngol Clin North Am 35:187-205, vii-viii, 2002.)
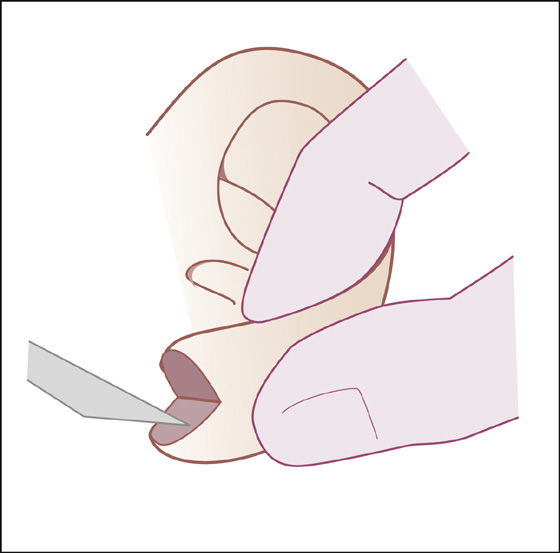
Figure 157-2 One-millimeter undermining of skin edges. (Adapted from Watson D: Torn earlobe repair. Otolaryngol Clin North Am 35:187-205, vii-viii, 2002.)
 Approximating the wound edges is crucial for a good cosmetic result. Placing 1 to 2 absorbable sutures, such as a 5-0 gut, will decrease dead space and hematoma formation as well as reduce tension on overlying skin sutures.
Approximating the wound edges is crucial for a good cosmetic result. Placing 1 to 2 absorbable sutures, such as a 5-0 gut, will decrease dead space and hematoma formation as well as reduce tension on overlying skin sutures.
 The wound can then be sutured in a simple straight-line closure (see Figure 157-1, C) using a fine monofilament suture, such as 6-0 nylon.
The wound can then be sutured in a simple straight-line closure (see Figure 157-1, C) using a fine monofilament suture, such as 6-0 nylon.
 Place a single suture at the most inferior portion of the lobe before placing the other sutures. This will ensure precise approximation and facilitate the remainder of the repair.
Place a single suture at the most inferior portion of the lobe before placing the other sutures. This will ensure precise approximation and facilitate the remainder of the repair.
 For repairs that remove the old track, excise the wound edges using an inverted V-shaped excision (Figure 157-3), removing all remnants of any cleft. Undermine the skin edges as previously (see Figure 157-2), and make a similar straight-line closure (Figure 157-4).
For repairs that remove the old track, excise the wound edges using an inverted V-shaped excision (Figure 157-3), removing all remnants of any cleft. Undermine the skin edges as previously (see Figure 157-2), and make a similar straight-line closure (Figure 157-4).
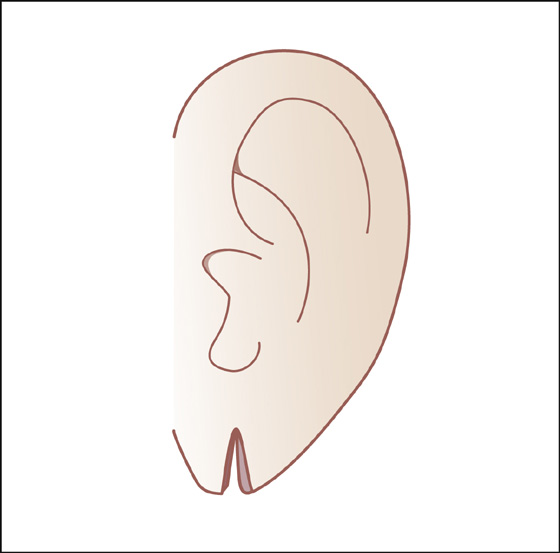
Figure 157-3 Inverted V-shaped excision of cleft. (Adapted from Watson D: Torn earlobe repair. Otolaryngol Clin North Am 35:187-205, vii-viii, 2002.)
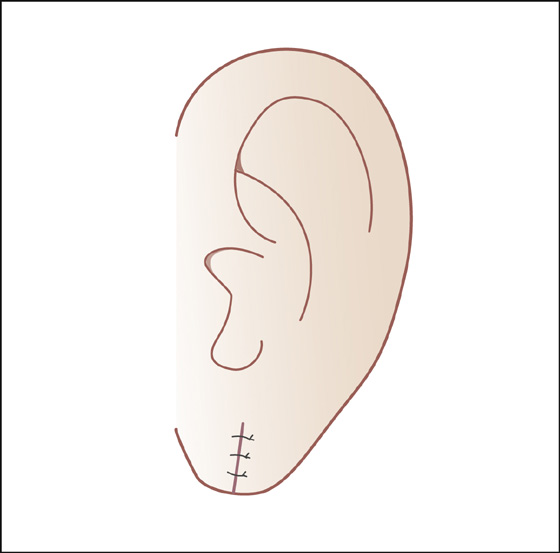
Figure 157-4 Straight-line closure. (Adapted from Watson D: Torn earlobe repair. Otolaryngol Clin North Am 35:187-205, vii-viii, 2002.)
 To reduce the risk for scar contracture with earlobe deformity, the straight-line closure can be replaced by a simple Z-plasty (Figure 157-5), closing the skin with the same fine (6-0) monofilament suture material.
To reduce the risk for scar contracture with earlobe deformity, the straight-line closure can be replaced by a simple Z-plasty (Figure 157-5), closing the skin with the same fine (6-0) monofilament suture material.
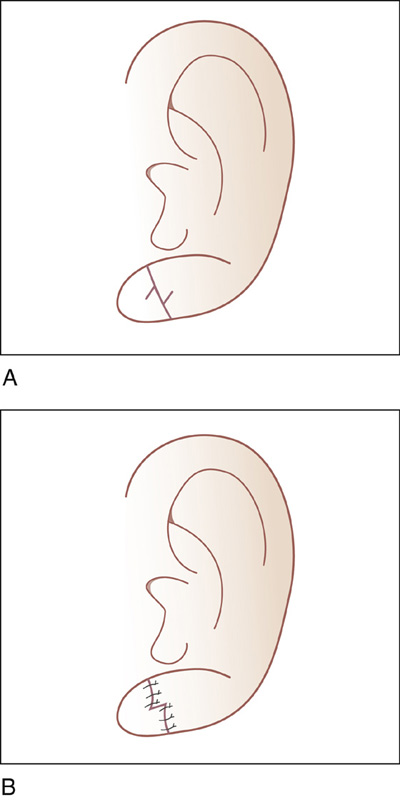
Figure 157-5 Straight-line closure with inferior rim modification by Casson. A, Incisions for a Z-plasty on inferior margin. B, Z-plasty flap transposition and closure. (Adapted from Watson D: Torn earlobe repair. Otolaryngol Clin North Am 35:187-205, vii-viii, 2002.)
 Aftercare should include daily showering and/or gentle wound cleansing with soap and water followed by application of bacitracin ointment or petroleum jelly is recommended.
Aftercare should include daily showering and/or gentle wound cleansing with soap and water followed by application of bacitracin ointment or petroleum jelly is recommended.
 Sutures should be removed in approximately 5 days. Consider using tissue adhesive (Dermabond) after the sutures are removed to reduce tension on the healing wound.
Sutures should be removed in approximately 5 days. Consider using tissue adhesive (Dermabond) after the sutures are removed to reduce tension on the healing wound.
 Patients should be instructed that repiercing, if desired, should not be done through the scar but should be placed adjacent to the repair site. This will create a stronger piercing that is less prone to cleft formation. Preferably, replacement of the earring site should be delayed by 3 months.
Patients should be instructed that repiercing, if desired, should not be done through the scar but should be placed adjacent to the repair site. This will create a stronger piercing that is less prone to cleft formation. Preferably, replacement of the earring site should be delayed by 3 months.
 Provide tetanus prophylaxis if needed (see Appendix H).
Provide tetanus prophylaxis if needed (see Appendix H).
What Not To Do:
 Do not close an earlobe tear when remnants of the old earring track are known to be inside. This old epithelial track will eventually form an inclusion cyst, which will often require excision later.
Do not close an earlobe tear when remnants of the old earring track are known to be inside. This old epithelial track will eventually form an inclusion cyst, which will often require excision later.
 Do not use ointment containing neomycin. The neomycin provides no advantage and can often produce severe contact dermatitis.
Do not use ointment containing neomycin. The neomycin provides no advantage and can often produce severe contact dermatitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 A loop of 2-0 nylon should be placed at the apex as a temporary earring site spacer, to be exchanged with an earring after being left in place for 1 month. Some authors do recommend repiercing with a sterile stud at the time of wound repair.
A loop of 2-0 nylon should be placed at the apex as a temporary earring site spacer, to be exchanged with an earring after being left in place for 1 month. Some authors do recommend repiercing with a sterile stud at the time of wound repair.