CHAPTER 181
Tinea Pedis, Tinea Cruris, Tinea Corporis
(Athlete’s Foot, Jock Itch, Ringworm)
Presentation
Patients usually seek medical care for “athlete’s foot,” “jock itch,” or “ringworm” when pruritus is severe or when secondary infection causes pain and swelling. Worrisome spreading of the rash, along with an unsightly and annoying appearance, will also motivate these patients to seek medical treatment.
Tinea pedis: There are three general clinical presentations: interdigital, moccasin, and vesicobullous. Interdigital disease is most common. Often there is fissuring, scaling, and maceration of the interdigitial or subdigital areas, particularly the fourth-to-fifth toe web space (Figure 181-1, A and B). Moccasin-type tinea is characterized by fine silvery scales, with underlying pink to red skin that most commonly affects areas of the soles, heels, and sides of the feet (moccasin distribution) (Figure 181-1, C). Vesicobullous tinea pedis is the least common form. There may be acute and highly inflammatory vesicular or bullous lesions that are pruritic and commonly found at the instep of the foot; however, inflammation may spread over the entire sole (Figure 181-1, D).

Figure 181-1 A, Interdigital tinea pedis. B, White macerated web between fourth and fifth toes. C, Moccasin distribution of tinea pedis. D, Bullous tinea. (From White G, Cox N: Diseases of the skin, ed 2. St Louis, 2006, Mosby.)
Tinea cruris: This is a dermatophyte infection of the inguinal folds, inner thighs, perineum, and buttocks that usually spares the scrotum and penis (unlike Candida intertrigo). There is an erythematous scaling eruption that is often annular in appearance (Figure 181-2). Pruritus is a common symptom, and pain may be present if the involved area is moist and macerated or secondarily infected. More commonly seen in men, tinea cruris often occurs in patients with tinea pedis and onychomycosis (dermatophyte infection of the toenails) and is thought to spread to the groin from contaminated underpants.

Figure 181-2 Tinea cruris. (From Bolognia J, Jorizzo J, Rapini R: Dermatology. St Louis, 2003, Mosby.)
Tinea corporis: This dermatophyte infection of the glabrous (hairless) skin elsewhere on the body typically presents as an erythematous, scaling, annular eruption with central clearing on the extremities or trunk (Figure 181-3). The classic ringworm pattern is a flat scaly area with a raised border that advances circumferentially. Vesicles or pustules may form as the lesion becomes inflamed.

Figure 181-3 Tinea corporis. (From White G, Cox N: Diseases of the skin, ed 2. St Louis, 2006, Mosby.)
What To Do:
 When microscopic examination of skin scrapings in potassium hydroxide (KOH) is readily available, definite identification of the lesion can be made by looking for the presence of hyphae or spores. Using a No. 10 scalpel blade, scrape flakes or scales from the active leading edge of the lesion (or from the web space) onto a glass slide. Sweep the particles toward the center of the slide and add a drop of 10% to 20% KOH and a cover slip. Warm with a flame, and then view under low (100×) magnification with the microscope light condenser lowered. Branching fungal filaments (hyphae and myceliae) identify superficial dermatophytes (Figure 181-4). Budding cells and pseudohyphae (“spaghetti and meatballs”) suggest yeast, particularly Candida organisms. Fungal cultures are rarely necessary for acute uncomplicated lesions. Treatment can be started presumptively when microscopic examination is not easily accomplished, but always consider the “herald patch” of pityriasis rosea (see Chapter 175), nummular dermatitis, secondary and tertiary syphilis, lichen planus, seborrheic dermatitis, psoriasis, impetigo (see Chapter 172), and neurodermatitis in the differential diagnosis.
When microscopic examination of skin scrapings in potassium hydroxide (KOH) is readily available, definite identification of the lesion can be made by looking for the presence of hyphae or spores. Using a No. 10 scalpel blade, scrape flakes or scales from the active leading edge of the lesion (or from the web space) onto a glass slide. Sweep the particles toward the center of the slide and add a drop of 10% to 20% KOH and a cover slip. Warm with a flame, and then view under low (100×) magnification with the microscope light condenser lowered. Branching fungal filaments (hyphae and myceliae) identify superficial dermatophytes (Figure 181-4). Budding cells and pseudohyphae (“spaghetti and meatballs”) suggest yeast, particularly Candida organisms. Fungal cultures are rarely necessary for acute uncomplicated lesions. Treatment can be started presumptively when microscopic examination is not easily accomplished, but always consider the “herald patch” of pityriasis rosea (see Chapter 175), nummular dermatitis, secondary and tertiary syphilis, lichen planus, seborrheic dermatitis, psoriasis, impetigo (see Chapter 172), and neurodermatitis in the differential diagnosis.
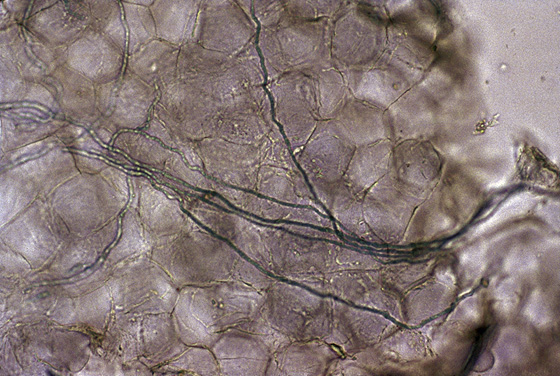
Figure 181-4 Potassium hydrochloride (KOH) preparation of a dermatophyte demonstrating branching hyphae. (From Bolognia J, Jorizzo J, Rapini R: Dermatology. St Louis, 2003, Mosby.)
 Terbinafine (Lamisil AT cream or spray), clotrimazole (Lotrimin or Lotrimin Ultra 1% cream, solution, or lotion), and miconazole (Micatin) 2% cream, spray, lotion, or powder, as well as butenafine (Mentax) 1% cream applied qd to bid are available over the counter and can be applied bid. Naftifine (Naftin 1% cream applied qd or 1% gel applied qd to bid) requires a prescription. If applied to the rash, they will cause involution of most superficial lesions within 1 to 2 weeks but may need to be continued for up to 4 weeks. They should be continued for 7 to 14 days beyond symptom resolution to prevent relapse. Advise the patient to apply the topical medication 2 cm past the border of the skin lesion.
Terbinafine (Lamisil AT cream or spray), clotrimazole (Lotrimin or Lotrimin Ultra 1% cream, solution, or lotion), and miconazole (Micatin) 2% cream, spray, lotion, or powder, as well as butenafine (Mentax) 1% cream applied qd to bid are available over the counter and can be applied bid. Naftifine (Naftin 1% cream applied qd or 1% gel applied qd to bid) requires a prescription. If applied to the rash, they will cause involution of most superficial lesions within 1 to 2 weeks but may need to be continued for up to 4 weeks. They should be continued for 7 to 14 days beyond symptom resolution to prevent relapse. Advise the patient to apply the topical medication 2 cm past the border of the skin lesion.
 Sertaconazole nitrate (Ertaczo) cream 2% [30, 60 g] is a newer imidazole agent that possesses both fungicidal and fungistatic properties to eradicate existing infections. In addition to antifungal properties, it exhibits anti-inflammatory and antipruritic effects. Apply bid (not approved for children younger than 12 years of age).
Sertaconazole nitrate (Ertaczo) cream 2% [30, 60 g] is a newer imidazole agent that possesses both fungicidal and fungistatic properties to eradicate existing infections. In addition to antifungal properties, it exhibits anti-inflammatory and antipruritic effects. Apply bid (not approved for children younger than 12 years of age).
 Rarely, more severe or extensive lesions can be treated with oral antifungals. Terbinafine (Lamisil), 250 mg qd × 2 weeks; ketoconazole (Nizoral), 200 mg qd × 4 weeks; or fluconazole (Diflucan), 150 mg weekly for 2 to 4 weeks, can be used. (See the Physicians’ Desk Reference [PDR] for adverse side effects and interactions.)
Rarely, more severe or extensive lesions can be treated with oral antifungals. Terbinafine (Lamisil), 250 mg qd × 2 weeks; ketoconazole (Nizoral), 200 mg qd × 4 weeks; or fluconazole (Diflucan), 150 mg weekly for 2 to 4 weeks, can be used. (See the Physicians’ Desk Reference [PDR] for adverse side effects and interactions.)
 With signs of secondary infection, begin treatment first with wet compresses of Burow solution (2 packets of Domeboro powder in 1 pint water) for a half hour every 3 to 4 hours. Use mupirocin (Bactroban) 2% cream for superficial bacterial infections (impetigo). With signs of deep infection (cellulitis, lymphangitis), begin systemic antibiotics with streptococcal coverage, such as cefadroxil (Duricef), 500 mg bid × 7 to 10 days; cephalexin (Keflex) or dicloxacillin (Dynapen), 250 to 500 mg qid × 7 to 10 days; or azithromycin (Zithromax), 500 mg, then 250 mg qd × 4 days. Always consider coverage for community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) if it is prevalent in your area (see Chapter 166).
With signs of secondary infection, begin treatment first with wet compresses of Burow solution (2 packets of Domeboro powder in 1 pint water) for a half hour every 3 to 4 hours. Use mupirocin (Bactroban) 2% cream for superficial bacterial infections (impetigo). With signs of deep infection (cellulitis, lymphangitis), begin systemic antibiotics with streptococcal coverage, such as cefadroxil (Duricef), 500 mg bid × 7 to 10 days; cephalexin (Keflex) or dicloxacillin (Dynapen), 250 to 500 mg qid × 7 to 10 days; or azithromycin (Zithromax), 500 mg, then 250 mg qd × 4 days. Always consider coverage for community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) if it is prevalent in your area (see Chapter 166).
 With inflammation and weeping lesions, a topical antifungal and steroid cream combination, such as Lotrisone in addition to the wet compresses, will be most effective. Warn patients that this medication has a potent steroid that can lead to skin atrophy or striae if used for an extended period, especially in the groin. An alternative is to use the recommended antifungals and add a low-dose over-the-counter (OTC) corticosteroid (e.g., 2.5% hydrocortisone cream [Cortaid]) for the first few days.
With inflammation and weeping lesions, a topical antifungal and steroid cream combination, such as Lotrisone in addition to the wet compresses, will be most effective. Warn patients that this medication has a potent steroid that can lead to skin atrophy or striae if used for an extended period, especially in the groin. An alternative is to use the recommended antifungals and add a low-dose over-the-counter (OTC) corticosteroid (e.g., 2.5% hydrocortisone cream [Cortaid]) for the first few days.
 For tinea pedis, instruct patients to wear nonocclusive footwear, such as sandals, that allow the foot to “breathe.” Have them put on socks before underwear to avoid spreading the fungus from feet to groin. A gel formulation of naftifine may be helpful for moist web spaces.
For tinea pedis, instruct patients to wear nonocclusive footwear, such as sandals, that allow the foot to “breathe.” Have them put on socks before underwear to avoid spreading the fungus from feet to groin. A gel formulation of naftifine may be helpful for moist web spaces.
 For tinea cruris, suggest loose undergarments made of absorbent materials, such as cotton rather than synthetics. Skin should be dried well with a towel or hair dryer. Absorbent powders and drying agents, such as Zeasorb-AF and Drysol, can be applied lightly.
For tinea cruris, suggest loose undergarments made of absorbent materials, such as cotton rather than synthetics. Skin should be dried well with a towel or hair dryer. Absorbent powders and drying agents, such as Zeasorb-AF and Drysol, can be applied lightly.
 To prevent reinfection when onychomycosis is present, nail infections should be treated (see later, this chapter).
To prevent reinfection when onychomycosis is present, nail infections should be treated (see later, this chapter).
What Not To Do:
 Do not attempt to treat fungal infections of the scalp (tinea capitis) with local therapy. A boggy swelling (tinea kerion) or patchy hair loss with inflammation and scaling requires systemic antifungals, such as griseofulvin.
Do not attempt to treat fungal infections of the scalp (tinea capitis) with local therapy. A boggy swelling (tinea kerion) or patchy hair loss with inflammation and scaling requires systemic antifungals, such as griseofulvin.
 Do not use Nystatin, a drug familiar for its usefulness against Candida infections. Tinea infections are not killed by this drug.
Do not use Nystatin, a drug familiar for its usefulness against Candida infections. Tinea infections are not killed by this drug.
 Do not treat with corticosteroids alone. They will reduce signs and symptoms (tinea incognito) but allow increased fungal growth.
Do not treat with corticosteroids alone. They will reduce signs and symptoms (tinea incognito) but allow increased fungal growth.
Discussion
Tinea infections are caused by superficial fungi known as dermatophytes, which are true saprophytes that take all their nutrients from dead keratin in the stratum corneum of the skin and the keratinized tissue of hair and nails. They cannot invade live epidermis. Some of these infections cause circular lesions that result from the inflammatory reaction, forcing the dermatophytes outward to an inflammation-free area. As long as the infection persists, so does the outward migration.
Tinea pedis or athlete’s foot is the most common fungal infection. It is seen most in those who wear occlusive footwear because shoes promote warmth and sweating, which encourage fungal growth. Tinea must be differentiated from allergic and irritant contact dermatitis (see Chapter 160). In several studies, application of the allylamine terbinafine bid resulted in a higher cure rate than twice-daily application of the imidazole clotrimazole, and at a quicker rate (1 week vs. 4 weeks).
All superficial dermatophytes of the skin, except those involving the scalp, beard, face, hands, feet, groin, and nails, are known as tinea corporis, or ringworm of the body. Contact with pets is often the source of the infection. Systemic diseases (e.g., diabetes, leukemia, acquired immunodeficiency disease [AIDS]) predisposes patients to tinea corporis.
Candidiasis and erythrasma may resemble tinea cruris, but candidal lesions are usually more moist, red, and tender (see Chapter 165). Pustules may be seen within the indistinct border, and satellite lesions may be scattered over adjacent skin. Candidiasis also may involve the scrotum or penis, which are usually spared by tinea. Candida organisms may be treated topically with naftifine (Naftin), ciclopirox (Loprox), or clotrimazole (Lotrimin, Mycelex).
Erythrasma is a skin infection caused by Corynebacterium minutissimum, a gram-positive bacterium. The rash characteristically consists of asymptomatic, reddish-brown, superficial dull patches with well-defined margins and no central clearing. The peripheral edge is not usually any more raised than the center (Figure 181-5, A). When illuminated with an ultraviolet Wood lamp, the infected skin glows with coral-pink fluorescence (Figure 181-5, B). Erythrasma is treated with oral erythromycin, 250 mg qid × 14 days.
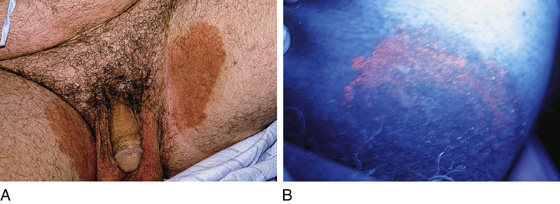
Figure 181-5 A and B, Erythrasma appears as red-brown patches of the groin or axilla that fluoresce coral-pink under Wood light examination. (From White G, Cox N: Diseases of the skin, ed 2. St Louis, 2006, Mosby.)
Tinea versicolor is a misnomer, because it is not caused by a dermatophyte fungus but by lipophilic yeast. Pityriasis versicolor is the more correct name. It is asymptomatic, and its presentation to an acute care facility usually is incidental to some other problem. There is, however, no reason to ignore this chronic superficial skin infection, which causes cosmetically unpleasant irregular patches of varying pigmentation that tend to be lighter than the surrounding skin in the summer and darker than the surrounding skin in the winter. Wood light examination sometimes reveals a white or yellow fluorescence (Figure 181-6).
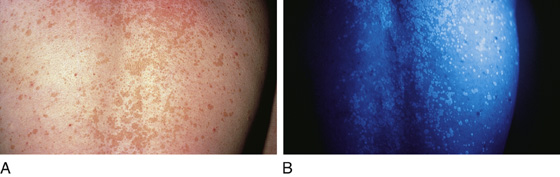
Figure 181-6 A, Tinea versicolor on the upper back of a young adult. B, Wood light examination of the same patient. (From White G, Cox N: Diseases of the skin, ed 2. St Louis, 2006, Mosby.)
Differential diagnosis includes tinea corporis, pityriasis alba, pityriasis rosea, vitiligo, leprosy, and secondary syphilis.
Prescribe a 2.5% selenium sulfide lotion (Selsun) to be applied as lather, leave on 10 to 15 minutes, then wash off daily for 10 to 14 days and then qhs monthly, or use three to five times weekly for 2 to 4 weeks (which also should be followed with monthly re-treatments). Alternatively, use terbinafine 1% solution (spray) twice daily for 1 week or ketoconazole (Nizoral) cream 2% daily for 2 weeks, or ketoconazole or fluconazole (Diflucan) as a single 300-mg oral dose to be repeated in 4 weeks. Also, itraconazole can be taken 200 mg qd × 3 to 7 days. (See the PDR for adverse side effects and interactions.) Superficial scaling should resolve in a few days, and the pigmentary changes will slowly clear over a period of several months. Tinea versicolor has a recurrence rate of 80% after 2 years; patients are therefore likely to need periodic re-treatment or preventive maintenance.
Tinea capitis is mainly a disease of infants, children, and young adolescents, usually involving black or Hispanic preschoolers. Tinea capitis presents in numerous ways: The primary lesions may be scales, papules, pustules, plaques, or nodules on the scalp. Inflammation and secondary infection lead to secondary processes, such as alopecia, erythema, exudate, and edema (Figure 181-7). A kerion forms as a result of increased cell-mediated immune response, demonstrated by an inflamed, exudative, nodular, boggy swelling with associated hair loss and cervical lymphadenopathy (Figure 181-8). Tinea capitis can be diagnosed on KOH examination of extracted hair. Culture must involve the extracted hair, not simply scales.

Figure 181-7 Tinea capitis. (From Bolognia J, Jorizzo J, Rapini R: Dermatology. St Louis, 2003, Mosby.)

Figure 181-8 Kerion with swollen regional lymph nodes. (From White G, Cox N: Diseases of the skin, ed 2. St Louis, 2006, Mosby.)
Onychomycosis (also known as tinea unguium) is an infection of the nail plate or nail bed that interferes with normal nail function (Figure 181-9). Patients with this infection often have concomitant fungal infections at other sites. Because onychomycosis requires expensive prolonged therapy (6 weeks for fingernail infections and 12 weeks for toenail infections), the diagnosis should be confirmed before treatment is initiated. This can be achieved by clipping off the distal edge of the affected nail, placing it in formalin along with attached subungual debris, and sending it for periodic acid–Schiff staining with histologic examination in a hospital or reference laboratory.

Figure 181-9 Tinea unguium or subungual onychomycosis. (From White G, Cox N: Diseases of the skin, ed 2. St Louis, 2006, Mosby.)
Terbinafine, at a dosage of 250 mg per day for 12 weeks, has a better mycologic cure rate than “pulse” therapy, in which 500 mg of terbinafine is given once daily for 7 days of each of 2 months (fingernails) or 4 months (toenails). It should be noted, though, that follow-up must be arranged with a patient’s primary doctor or dermatologist. Long-term dosage with this drug has caused some significant liver disease. Terbinafine is considered the drug of choice for dermatophyte onychomycosis, with greater mycologic cure rates, less serious and fewer drug interactions, and a lower cost than continuous itraconazole therapy. Adjunct débridement may improve the clinical and complete cure rates compared with terbinafine alone.
Newer oral antifungal agents have greatly improved the management of dermatomycoses, but not without consequence. Some are very expensive, have side effects and organ toxicity that may or may not be tolerable, and have significant adverse drug interactions. Laboratory monitoring is recommended during treatment with all oral antifungal medications. Liver function tests for itraconazole should be done at baseline, at 1 month, and if any signs or symptoms of liver dysfunction present. Terbinafine use warrants liver function tests at baseline, at 6 weeks, if signs or symptoms present, and then 4 weeks later. In general, one should monitor patients more closely if taking medications that impair renal or hepatic function.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


