Fig. 20.1
Common clinical question for a patient with polytrauma: Should the patient initially undergo external fixation, (a) damage control orthopedics, or definitive reamed intramedullary nail insertion, (b) early total care?.
Technique with Personal Tips
Our general approach to femoral shaft fracture fixation has yielded good outcomes and a low rate (1.5 %) of ARDS [7] despite a relatively low rate of DCO. Only 13 % of patients with polytrauma that includes femoral fractures receive DCO, and none of the isolated femora are treated in this manner. This success has been achieved at other North American centers [7].
Patients can be grouped into three broad categories: stable, borderline, and unstable. Stable patients should receive early total care (ETC) when possible. Those unstable (or in extremis) should receive DCO. Authors have proposed multiple criteria with which to identify “borderline” patients [8], and debate continues regarding which borderline patients are best served by DCO versus ETC.
At our center, patients receive DCO for three common reasons: (1) ongoing cardiopulmonary distress, (2) traumatic brain injury (TBI), and (3) failure to respond to resuscitation as measured by parameters such as lactate [1]. Patients, on average, undergo fixation approximately 13 h from presentation at the institution [7], and emerging data indicate that fixation within 12 h, particularly for those with abdominal injuries, increases mortality [9]. We think that patients should not be “rushed” to the operating room before adequate resuscitation has been achieved, even recognizing resuscitation continues in the operating room.
There are no firm rules regarding any of these parameters, and careful clinical judgment is needed in evaluating the totality of the patient. Regarding the cardiopulmonary status of the patient, we argue against placing a nail in any patient who is currently hypotensive or requiring massive transfusion, and we typically would not place a nail in a patient requiring pressors before surgery. Further, although we commonly place reamed nails in patients with lung injuries, we will not do so in the subset of patients with high oxygen requirements on airway pressures indicating poor lung function that might be worsened by nail placement.
Determining which TBI can be treated is complex, and high-level conversation often is required to facilitate initial placement of external fixation to receive the proposed pulmonary benefit of DCO. We use failure to respond to indicate lactate trending toward 2.5 [7, 10], although recent work has shown that a value of 4.0 might be more reasonable [11].
Most work on DCO focuses on femoral shaft fractures, but the general concepts can be extrapolated to other fractures. Patients who are deemed appropriate to receive DCO are treated with external fixation for certain fractures (femoral shaft, mechanically unstable pelvis) and splint fixation for other fractures (humeral shaft, distal radius, closed tibial shaft). Open fractures undergo débridement, and the compartments are released as needed.
Patients with multiple fractures require continuous reevaluation in the operating room to assess whether the original plan for ETC is still safe. We typically develop “break points” in the surgery at which we reevaluate how the patient is doing before continuing. If the patient’s status changes, a decision is made to change to DCO. This approach requires thoughtful planning by the orthopedic team regarding the sequence of fracture fixation and close coordination between the orthopedics and anesthesia teams (and possibly consultation with a general surgery team) to ensure the safest approach.
Once the decision to use DCO has been made, the timing of definitive fixation is guided by the rationale for DCO. If the decision was because of TBI or failure to respond to resuscitation, we proceed once resuscitation is complete and/or the TBI stabilizes. For patients who receive DCO because of persistent shock or pulmonary issues, we are more conservative and tend to wait a longer time period. Some argue that the inflammatory cascade resulting from nail insertion is lessened in patients who are treated >5 days after injury [12]; however, we do not strictly adhere to this argument. We prefer to have a patient’s respiratory status improved to the level of being near extubation before proceeding with procedures such as femoral nail insertion that might place the lungs at additional risk of damage.
When in doubt, a DCO approach should be used. Although the overuse of DCO leads to unnecessary surgery and likely delays discharge, underuse of DCO could lead to death. For this reason, if the clinician is unsure, we recommend DCO.
Outcomes
Outcome data indicate that our general approach to femoral shaft fractures in patients with polytrauma yields low rates of death (2 %) and ARDS (1.5 %) [7], despite the high-energy nature of the mechanisms of injury in our patient cohort. Several explanations exist for our center’s relative improved performance over German studies on the topic [7], and one possibility is differences in ventilator management [13]. Complication rates of late conversion to nails after initial external fixation seem to be low [5]. Other centers have reported good outcomes with similar algorithms for a broader range of fractures, including an “early appropriate care” algorithm for pelvic and acetabular fractures [11].
Complications with Treatment
The dreaded complications associated with the inappropriate timing of fracture fixation in patients with polytrauma are ARDS, SIRS, and death. The severity of the sequelae of errors in this decision heightens the importance of all clinicians being aware of these issues.
DCO is not associated with particular complications except soft tissue issues related to external fixation. Prolonged external fixation of femora does not seem to incur risk of subsequent infection; however, surgeons are hesitant to insert a nail to treat a tibial fracture that has been in an external fixator for more than 2 weeks because of the concern regarding infection.
Timing of Open Fracture Treatment
History of Care
Open fractures (Fig. 20.2) traditionally were thought to require emergent débridement within 6 h of injury to reduce the risk of osteomyelitis. This “6-hour rule” seems to have been derived largely from guinea pig studies in abdominal surgery in the 1800s before the advent of antibiotics. Multiple studies and systematic reviews of the literature have failed to establish the validity of this link [14]. Even in high-energy lower extremity fractures thought to be at highest risk of infection, time to the operating room was not predictive of infection risk [15]. Interestingly, time to the definitive treatment center is predictive of infection rates, and Pollak et al. [15] theorized that this time is a marker for time to definitive resuscitation.


Fig. 20.2
Timing of débridement remains controversial, but the 6-h rule for débridement of fractures, even high-energy fractures such as a femoral fracture after an industrial accident, as shown, has not stood the test of time.
Technique with Personal Tips
At our center, we do not rush open fractures to the operating room. Time is allowed for adequate resuscitation before débridement as needed. We almost always treat open fractures within 24 h after injury and more often within 12 h but typically not within 6 h [14, 15].
There is, however, a subset of open fractures that we tend to treat with more emergent débridement. These fractures are the rare high-grade open fractures with gross contamination that typically require multiple débridement procedures. The wounds are so contaminated that every effort should be made to quickly decrease the bacterial load. No data are currently available to support this practice, but we are less inclined to let these fractures wait until the morning.
Attempts at treating all open fractures in a more emergent manner have some potential downsides. Allowing time to pass allows borderline tissue to declare itself better and increases the effectiveness of the initial débridement. Considering that many lower energy fractures are closed definitively, the quality of this initial débridement is likely important. Further, resources needed for emergent treatment of open fractures, which typically occur in the middle of the night, might not be in-house at all trauma centers. Expending resources in an effort that is not clinically indicated is not globally beneficial.
Some patients are so ill or have such concerning TBI that fracture care for more than 24 h is appropriate. Our policy is to maintain antibiotics until the patient is treated. Specific data regarding these rare patients is not available, but evidence that preoperative antibiotics reduce infection rates in open fractures is strong [16], so it is our practice to make every attempt to continue antibiotics at least until débridement can be performed.
Outcomes
The outcomes of fractures that are treated outside the 6-h window from injury seem to be similar to those of fractures treated within that window [14, 15]. No level I studies are available, and none are likely to emerge. Available retrospective studies suffer from selection biases that might skew the results in either direction. A much more powerful predictor of the infection rate is the open fracture grade [17], which shows markedly increasing infection rates as the grade increases from type I to IIIC.
Complications with Treatment
Infection and osteomyelitis potentially result from delayed débridement. Osteomyelitis in the setting of fractures can require many surgical procedures to “cure” the disease, if this is even possible, and results in amputation in some cases. Considering the severity of this complication, for patients who cannot undergo débridement within 24 h after injury, every effort is made to perform débridement as soon as possible.
Timing of Compartment Syndrome Treatment
History of Care
Although controversy continues regarding the diagnosis of compartment syndrome [18], almost no controversy exists regarding the ideal timing of treatment. Both animal [19–22] and clinical [23, 24] studies support emergent treatment with fasciotomy. The window of time after which outcomes substantially decline is approximately 6–12 h after injury [19–24].
Technique with Personal Tips
Compartment syndrome is a true emergency that should be treated in the operating room as quickly as possible. There is no known or theoretic benefit to delay. The surgery is simple (Fig. 20.3) and can be performed with almost no equipment in any operating room by any well-trained surgeon. The leg is the most common site of compartment syndrome, and the treatment procedure is described in detail in a recent chapter on the topic from this institution [25].
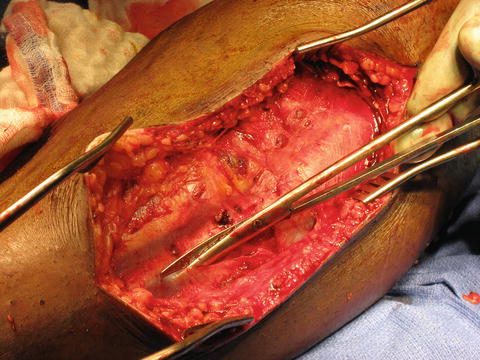
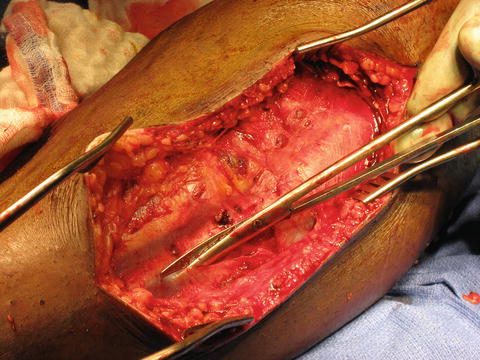
Fig. 20.3
Strong data support that compartment syndrome should be treated with emergent fasciotomy, such as that shown, which is being performed in the anterior and lateral compartment of the leg.
We recommend a two-incision fasciotomy technique that releases all four compartments of the lower leg. One incision is parallel to the fibula but centered approximately 1 cm anterior to it. This wound allows release of both anterior and lateral compartments. The superficial peroneal nerve should be identified and avoided, if possible. The second incision is located 1 cm posterior to the medial border of the tibia and allows release of both the superficial and deep posterior compartments. The posterior border of the tibia should be exposed, which indicates that the deep posterior compartment has been released. Skin incisions typically are at least 20 cm in length.
Two common errors are to make the incisions too small and to fail to release all four compartments. More muscle mass is present proximally in the leg, so adequate proximal releases are particularly important. Wounds often are initially managed with vacuum-assisted closure unless there is a concern for hemostasis. The wounds typically are treated with a second look 3 or 4 days later, with attempts at closing the medial wound at each return trip to the operating room. The lateral wound often requires split-thickness skin grafting approximately 1 week after surgery.
Outcomes
Patients who undergo fasciotomy more than 6–12 h after onset of symptoms have significantly worse outcomes (P < 0.05). Outcomes of delayed treatment or, even worse, missed compartment syndrome can be devastating. Loss of muscle function and foot drop are common. Complete loss of muscle function, renal damage from rhabdomyolysis, and amputation can occur.
Complications with Treatment
Treatment delay leads to poor outcomes, as noted previously. No complications are associated with earlier treatment.
Timing of Acetabular Fracture Fixation
History of Care
The ideal timing of acetabular fracture fixation is controversial. Delay of treatment beyond 2 weeks from injury is associated with poor hip outcomes and high rates of posttraumatic arthritis [26]. However, it is unclear how early acetabular fractures should be treated. It is thought that bleeding is increased with early treatment, perhaps leading to increased risk of mortality and prolonged stay in the intensive care unit. However, early treatment, analogous to the approach described previously for patients with polytrauma, might get the patient out of bed sooner and reduce the risk of respiratory and other systemic complications.
Technique with Personal Tips
We divide acetabular fractures into “high-risk” and “low-risk” categories in terms of bleeding. Low-risk acetabular fractures include simple fractures that can be fixed relatively quickly with lower blood loss, such as “posterior wall” [27] acetabular fractures (Fig. 20.4a). High-risk acetabular fractures are complex fracture types (e.g., “associated both columns”) (Fig. 20.4b, c). Fracture and patient specifics help define risk of bleeding. Earlier treatment is thought to be safe in healthier patients. We delay fixation in older patients who can tolerate blood loss more poorly to allow clot to solidify. Blood loss for complex cases can reach 3,000 mL or more.
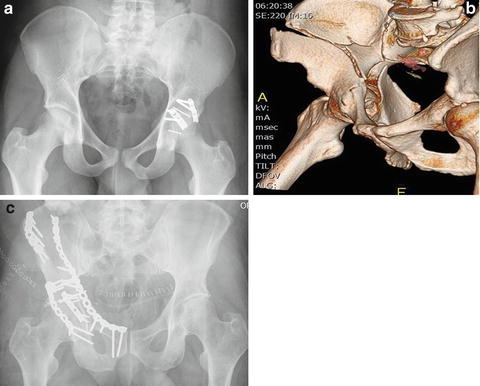
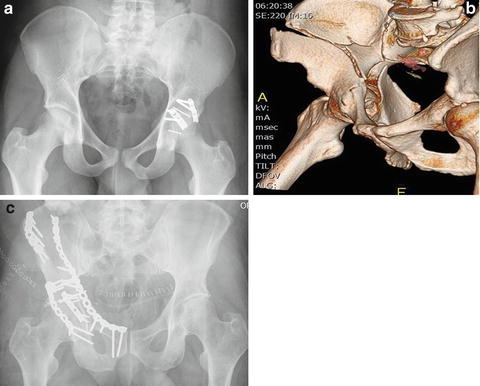
Fig. 20.4
Simple acetabular fractures, such as posterior wall fractures (a) in healthy patients, can typically be treated safely with immediate fixation. More complex patterns that require more extensive approaches and surgery should be delayed a few days from injury (b and c), particularly in elderly patients or other patients who cannot tolerate significant blood loss.
Low-risk fractures are treated as soon as the patient has been deemed appropriate for surgery. High-risk fracture patient combinations are delayed 2–3 days in traction. Acetabular fractures are not good “night and weekend” cases because they can require significant resources from surgical and anesthetic teams.
Outcomes
Early treatment of posterior wall fractures seems to be safe and is not associated with clinically important increase in blood loss [27]. Based on anecdotal evidence, early treatment of complex fractures is associated with increased risk of bleeding and is not important in younger patients but is likely important in geriatric or sicker patients. We rarely proceed early with patients who are at high risk of bleeding, thus limiting our ability to assess the danger of early surgery in these patients [28].
Complications with Treatment
When performed too early, surgery can result in increased bleeding. Unnecessary delay can be associated with prolonged bed rest and traction that delays mobilization and discharge.
Timing of Hip Fracture Fixation
History of Care
Geriatric Hip Fractures
The timing of hip fracture treatment (Fig. 20.5a, b) is controversial. Geriatric hip fractures dominate this issue. More and more data exist suggesting that delay in fixation beyond 48 h is associated with increased mortality, even when controlling for risk factors for death [29, 30].
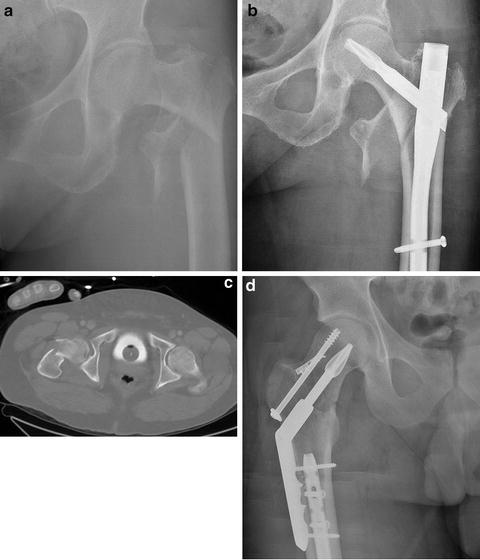
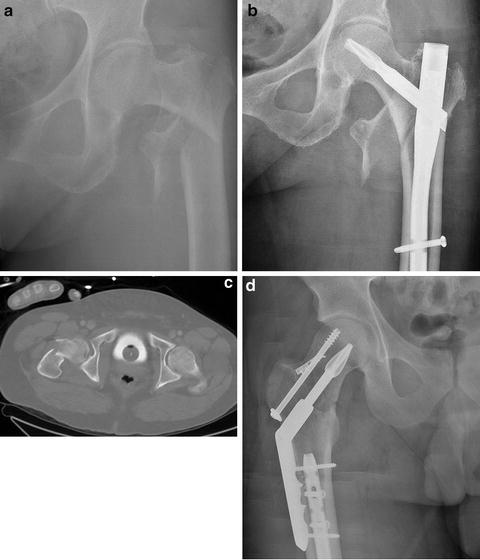
Fig. 20.5
Low-energy geriatric hip fractures (a) should be fixed (b) within 48 h to limit mortality. Timing of high-energy displaced femoral neck fractures in young patients (c) is more controversial, with some surgeons recommending emergent treatment to limit the risk of avascular necrosis of the femoral head and others treating urgently in the light of day to optimize surgical reduction (d).
High-Energy Displaced Femoral Neck in the Young
Another issue exists regarding the timing of treatment of displaced intra-articular hip fractures in young patients (Fig. 20.5c, d). Historically, these fractures have been labeled orthopedic emergencies in an effort to reduce the risk of avascular necrosis of the femoral head. The fragile blood supply to the femoral head can become kinked and is not restored until better alignment is obtained. Emergent capsulotomy to reduce hematoma in the hip capsule that might also be compromising blood flow has been advocated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








