8
Thoracic injuries
Introduction
Thoracic injury is one of the most serious types of trauma, second only to central nervous system injuries and may result in disruption of the airway, breathing or circulation. It is responsible for approximately 25 % of trauma-related deaths and approximately 33 % of patients presenting with blunt trauma will have a thoracic injury (Kiraly & Schreiber 2010). Although many of these deaths occur immediately from the combined effects on respiratory and haemodynamic function, namely hypoxia, hypercarbia and acidosis (Rooney et al. 2000), there is a significant group of patients who, having sustained thoracic trauma, may survive with simple prompt effective systematic assessment and management. The management of patients with chest injuries can, therefore, be challenging and rewarding.
Mechanisms of injury
Blunt and penetrating mechanical energy transfers are the most common causes of thoracic trauma (Legare & Sawatzky 2010). Blunt chest trauma commonly results from rapid deceleration of the chest wall against a solid object. Typically, this is seen following road traffic collisions (RTCs) in which the chest strikes the vehicle steering wheel, causing a high-velocity blunt chest injury. Superficial tissues are mostly affected; however, as the energy transfer increases in direct-force injuries, deeper tissues become involved, producing contusions, haemorrhages, organ ruptures and fractures. RTCs represent the most common cause of blunt thoracic trauma (Kiraly & Schreiber 2010). However blunt chest trauma can also result from a fall from a height. Shearing forces make organs and tissue planes move relative to each other, resulting in tearing of the communicating structures and blood vessels. This type of chest trauma may be associated with injuries to the great vessels, major airways, lung parenchyma and myocardium, as well as diaphragmatic rupture and fractures to the ribs and/or sternum. Crush injuries are second only to RTCs as a major cause of blunt trauma, this includes chest compressions during cardiopulmonary resuscitation efforts which may also lead to cardiac injury (El-Chami et al. 2008). Frequently, fractured ribs and cardiac and pulmonary contusion may ensue. Other causes of blunt chest trauma include blast injury and low-velocity impact from direct blows to the chest. Penetrating injuries, such as stabbings or gunshot wounds, cause 7.9 % of major trauma in the US compared to 4 % in Europe (Edwards et al. 2007, Glance et al. 2010). There is no longer such a large gap (15 %) between the two continents where penetrating trauma is concerned.
Anatomy of the chest
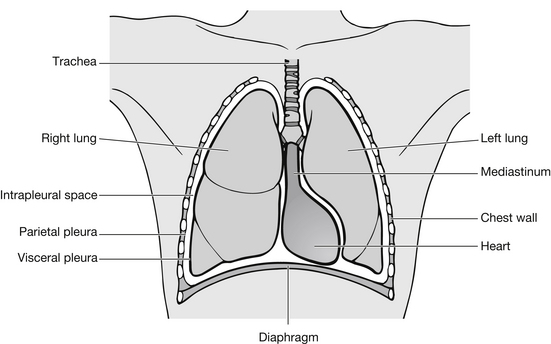
Chest injury occurs when there is damage to the thoracic cage or its contents. The thoracic cage comprises ribs and intercostal muscles. It is divided by the central mediastinum, which acts as a partition between the lungs. The outer surface of each lung is covered by the visceral pleura and this is reflected onto the chest wall as the parietal pleura (Fig. 8.1). The two pleural layers are effectively sealed together by a film of pleural fluid that exerts a strong surface tension force that prevents separation of the membranes. This enables the lungs to cling tightly to the thorax wall, which forces them to expand and recoil passively as the volume of the thoracic cavity alternately increases and decreases during breathing (Marieb & Hoehn 2007). If the pleura is breached, e.g., as a result of penetrating trauma, the integrity of this system is disrupted and the lung will collapse.
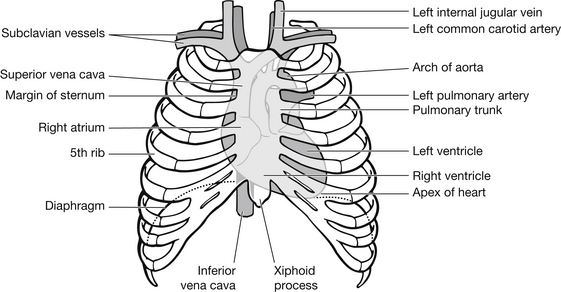
The heart lies above the diaphragm at the base of the thoracic cavity, with two-thirds of its bulk to the left of the body’s midline. The outer surface of the heart is covered by the visceral pericardium. This is reflected onto the surrounding fibrous sac to form the parietal pericardium. A thin film of fluid separates these pericardial surfaces, allowing the heart to move freely, only being anchored by the great vessels (Fig. 8.2). This potential space can become filled with blood (haemopericardium) following trauma or myocardial infarction. As the fibrous pericardium is unable to distend, any fluid collecting within the potential space (pericardial cavity) will exert pressure on the heart and impair filling.
Below the level of the fourth intercostal space, the thoracic cage surrounds the upper abdominal region, particularly when the diaphragm elevates during expiration. Any injury to the ribs at or below this level should alert the nurse that an intra-abdominal injury, specifically to the liver, spleen or diaphragm, may also be present.
The physiology of respiration
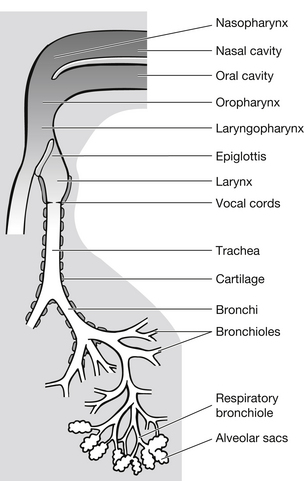
The key functions of respiration are oxygen uptake and carbon dioxide elimination. To enable this to happen, air is conveyed through the respiratory tract – this is called ventilation (Fig. 8.3).
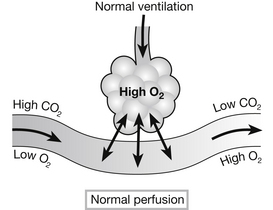
In addition, an adequate blood volume must circulate through the pulmonary capillaries. This is called perfusion. The exchange of oxygen and carbon dioxide between the alveoli and capillaries is called diffusion. Gases move from an area of high partial pressure to one of low partial pressure. When leaving the lungs via the alveolar capillaries and into the pulmonary veins, blood has its highest partial pressure of oxygen (PO2) (Marieb & Hoehn 2007).
• a high concentration of oxygen in the alveolus
• a low blood concentration of oxygen
• membrane thickness that the gas has to cross
Damage to either system leads to hypoxia or hypercapnia, which in turn threatens homeostasis. The ratio between ventilation and perfusion is fundamental to the success of respiratory function (Fig. 8.4).
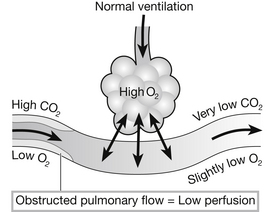
If a problem occurs with pulmonary flow, most commonly a low circulatory volume in trauma, adequate oxygen cannot be taken up. This is because less blood passes the alveoli and there is subsequently less haemoglobin take-up of oxygen. This results in a decrease in tissue perfusion. Unbound oxygen is expired. This results in a high ventilation/perfusion ratio (Fig. 8.5).
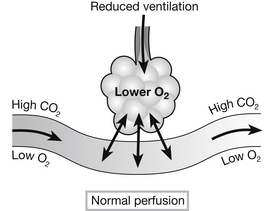
If ventilation decreases, most commonly with an obstructed airway, the amount of oxygen reaching the alveoli is reduced. When perfusion is normal this results in more blood and haemoglobin passing the alveoli than can be saturated with oxygen. As a result, the blood leaving the lungs has a low oxygen content. This is a low ventilation/perfusion ratio (Fig. 8.6).
Although the ventilation/perfusion ratio varies in different parts of the lung, a high ratio in one area will not offset a low ventilation/perfusion ratio in another. This is because of the reduction in haemoglobin saturation. In the trauma patient, particularly where chest injury has occurred, maintaining adequate ventilation is crucial in preventing hypoxia. Oxygen should be administered in high-inspired concentrations (preferably via face mask) to all patients as soon as they are placed on the bed (Curtis et al. 2010). Acidosis, which results from impaired ventilation associated with chest injury, activates the respiratory centre to increase respiratory rate and depth, which eliminates more CO2 (Marieb & Hoehn 2007). Metabolic acidosis results from inadequate tissue perfusion secondary to airway, breathing and circulatory problems, further compounding the patient’s condition.
Principles of care
Each hospital should have its own activation criteria based on its individual patient population. This may also be dependent on the size of emergency department, and some major trauma centres now have a tiered response to the multiple injured patients (Curtis & Asha 2010). Many EDs have established a system of care for seriously injured patients based on a team approach that utilizes Advanced Trauma Life Support (ATLS) principles and incorporates well-established objectives of trauma management (American College of Surgeons 2008) (see Chapter 2). The team leader is responsible for the coordination of care and the appropriate delegation of roles whilst maintaining an overview of the situation. The use of a standardized systematic approach not only expedites patient care, but also offers a format enabling less-experienced staff to focus their activities in a predetermined order. Some hospitals have established trauma teams in which each member has a specific role.
Clearly, the ED nurse’s role is dynamic and directly related to the patient’s needs. The key components of the nursing role when caring for patients with chest trauma are outlined in Box 8.1. The number and experience of other team members may influence the nurse’s actual activities, but the needs of the patient and their family/friends must remain paramount. Ideally, a member of the care team will be allocated to care for and liaise with the patient’s family and/or friends (see Chapter 14 for guidance on this issue).
Assessment of chest injury
The immediate management of the patient with chest injury should follow the principles laid down in the ATLS guidelines (American College of Surgeons 2008). A primary survey should be carried out to identify and treat any immediately life-threatening conditions (Box 8.2; the management of specific conditions will be discussed later in the chapter). In the stable patient, a secondary survey or head-to-toe examination should then be carried out to identify any other injury.
The Trauma Nursing Core Course (Emergency Nurses Association 2007) and similar such courses recommend pre-hospital information should be obtained before the patient’s arrival to ED, e.g., a tension pneumothorax may have been decompressed. The sequence of questions in the hand-over to the hospital care can be remembered as ‘MIST’: Mechanism of injury, Injuries found and suspected, Signs (respiratory rate, sPO2, blood pressure), Treatment given pre-hospital.
Additional investigations may include:
• chest X-ray/lateral cervical spine and pelvis (trauma series)
• blood chemistry (may include CPK and CK-MP, troponin I and troponin T; however, no specific blood test for myocardial injury following trauma exists)
• full blood count and cross-match
• ultrasound/echocardiography/Focussed Assessment with Sonography for Trauma (FAST)
• computed tomography/magnetic resonance imaging
• angiography (aortic disruption)
• thorascopy: direct or video assisted if not contra-indicated.
A specific chest injury assessment is listed in Box 8.3.
Initial management of chest injury
Management of chest injury should include high-flow oxygen as described above. The method of delivery depends largely on the patient’s condition; in a conscious patient without obvious compromise, use of a tight-fitting mask (NB: be aware of possible parallel facial injuries) and non-rebreathing bag is the method of choice. If the patient is unable to maintain their airway, as is common after chest injury, supportive methods should be found (Box 8.4).
Airway compromise occurs either because of damage to the airway, resulting in oedema, compression, bleeding, foreign body obstruction, displaced facial bones or suspected cervical spine injuries, or through a deterioration in the patient’s consciousness level, resulting in the loss of the gag reflex. If breathing is absent, the airway should be assumed to be blocked. Noisy breathing (stridor) may be indicative of partial upper airway obstruction or laryngospasm. If the patient is able to give a verbal response, then the airway can be assumed to be patent for the present time (Box 8.5).