Introduction
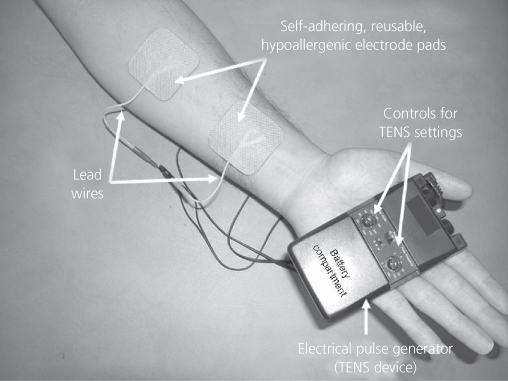
Transcutaneous electrical nerve stimulation (TENS) is a non-invasive analgesic technique that administers pulsed electrical currents across the intact surface of the skin to activate underlying nerves. A battery powered portable device is used to generate currents and self-adhering conducting pad electrodes are used to deliver the currents through the skin (Figure 18.1). TENS is used as a stand-alone treatment for mild to moderate pain and in combination with drug medication for moderate to severe pain. There is no known potential for overdose and there are few side effects or drug interactions, so patients can self-administer TENS and titrate dosage as required. Effects are generally rapid in onset and offset so patients are encouraged to administer TENS throughout the day. TENS devices are inexpensive and can be purchased without medical prescription in the United Kingdom.
Electric catfish (Malapterurus electricus) and electric rays (Torpedo marmorata) which can generate 300-volt shocks were used by the ancient Egyptians (2500 BC), Greeks (400 BC) and Romans (AD 46) to treat pain (Figure 18.2). The invention of electrostatic machines catalysed the use of electrotherapeutic devices in mainstream medicine in the 19th century.
Figure 18.2 Natural sources of electrical pain modulation. (a) Malapterurus electricus – Electric Catfish. (b) Torpedo marmorata – Marbled Electric Ray.

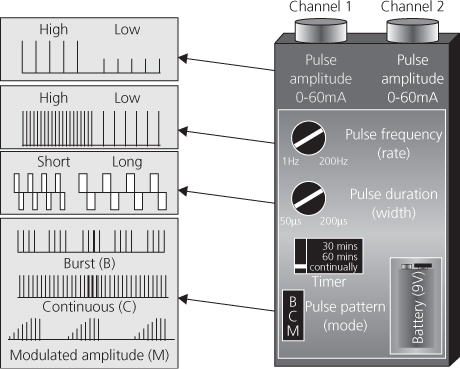
In 1965, Melzack and Wall suggested that activity in large diameter myelinated afferents (A-beta) could inhibit onward transmission of noxious information in the central nervous system resulting in pain relief akin to ‘rubbing pain better’. Percutaneous electrical stimulation of peripheral nerves was shown to reduce chronic neuropathic pain and dorsal column stimulation, a forerunner of spinal cord stimulation, shown to relieve chronic pain. TENS was used to predict the success of spinal cord stimulation implants until it was realised that TENS was a successful modality on its own. Nowadays, a variety of ‘TENS-like devices’ are available on the market (Johnson, 2001), although the term TENS is generally used to describe stimulation using a ‘standard TENS device’ (Figure 18.3).
Figure 18.3 Output characteristics of a standard TENS device. Differences in design between manufacturers are often minor and cosmetic.
Techniques and Mechanism of Action
Users select different TENS settings and electrode positions in order to activate different types of peripheral nerve fibre (Box 18.1).
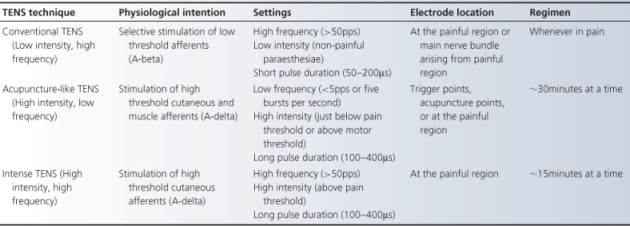
Conventional TENS
The physiological intention of TENS, in its conventional form, is to selectively stimulate A-beta afferents in pain-related dermatomes (Figure 18.4). Extracellular recordings from spinal cord neurones in anaesthetised rats and cats have shown that TENS delivered to somatic receptive fields inhibits noxious evoked responses in sensitised wide dynamic range cells immediately and one hour after stimulation. This inhibition remains after spinal cord transection, suggesting segmental neural circuitry. TENS reduces aspartate and glutamate levels in the spinal cord via the release of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA).
Figure 18.4 Segmental action of conventional TENS. White arrows indicate TENS-induced impulses leading to segmental analgesia. Nociceptive afferent input causes activity in second order nociceptive transmission cells in the central nervous system [1] which leads to pain. Activation of large diameter non-noxious afferents by TENS [2] activates interneurones [3] which release inhibitory neurotransmitters such as GABA and reduce activity in second order nociceptive transmission cells [4]. Nociceptive input to the brain declines resulting in pain relief [5]. TENS-induced activity in non-noxious transmitting pathways results in a sensation of electrical paraesthesiae [6].
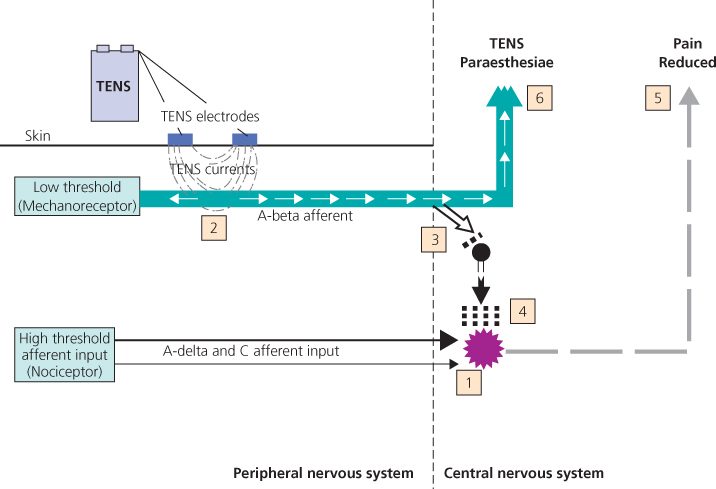
Large diameter afferents have lower thresholds of excitation than their small diameter counterparts, so A-beta afferents are selectively activated by titrating TENS pulse amplitude. A strong, comfortable, non-painful paraesthesia beneath the electrodes is indicative of A-beta activation and is achieved using low intensity currents. Large diameter afferents have short refractory periods and high rates of impulse generation. Hence, high frequency TENS may produce a stronger afferent barrage and stronger segmental inhibition. Low frequency TENS has been shown to involve mu opioid receptors and high frequency TENS delta opioid receptors in animal studies. Claims about optimal pulse frequencies, durations and patterns in humans are based on poor quality research, so patients are encouraged to adjust settings to find the most comfortable settings for their pain at that moment in time.
Acupuncture-like TENS (AL-TENS)
AL-TENS is a form of hyperstimulation first described Sjölund and colleagues. The physiological intention of AL-TENS is to activate high threshold cutaneous and muscle afferents (A-delta) which prolongs segmental nociceptor cell inhibition by up to 2 hours. AL-TENS has been shown to activate nuclei in the midbrain periaqueductal grey and rostral ventromedial medulla associated with descending pain inhibitory pathways which synapse at all levels of the spinal cord. This leads to extrasegmental analgesia (Figure 18.5). AL-TENS increases central levels of opioids, serotonin and noradrenaline, which have a key role in inhibiting onward transmission of noxious information in the spinal cord.
Figure 18.5 Extrasegmental action of acupuncture-like TENS. White arrows indicate TENS-induced impulses leading to extrasegmental analgesia. Nociceptive afferent input causes activity in second order nociceptive transmission cells [1] which leads to pain. Higher intensity TENS activates A-delta afferents directly [2] and/or motor neurones leading to a muscle twitch [3]. Small diameter muscle afferent activity from the muscle twitch [4] activates central ascending pathways [5], which excite descending pain inhibitory pathways [6] and inhibition of second order nociceptive transmission cells [7]. Nociceptive input to the brain declines resulting in pain relief [8]. TENS induced activity results in sensations of electrical ‘twitching’ [9].
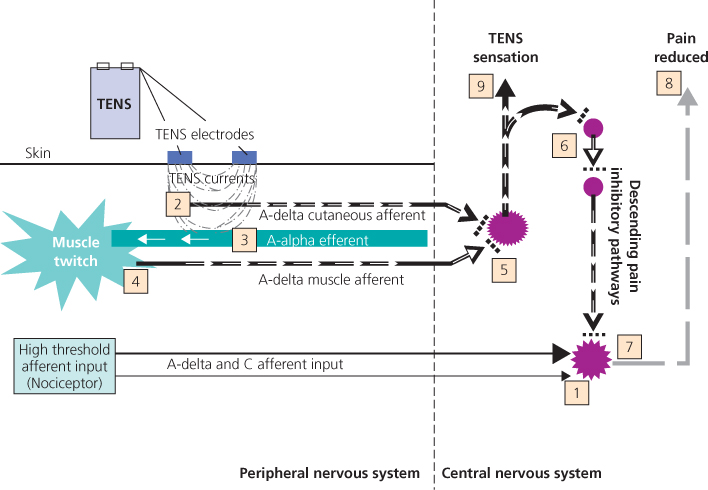
AL-TENS is administered using high intensity, low frequency currents. AL-TENS is often delivered to generate non-painful muscle twitches because A-delta muscle afferent activity has been shown to generate larger inhibition than cutaneous afferents. The user titrates TENS pulse amplitude to the desired intensity; low frequency trains or bursts (2–4 Hz) of high frequency pulses (100–200 pps) are often used, as they are more comfortable than single pulses delivered at low frequency. Electrodes are positioned in pain-related dermatomes, myotomes, acupuncture points and trigger points. Patients administer AL-TENS less frequently than conventional TENS, for example 20 minutes, three times a day.
Intense TENS
Intense TENS is a form of counter-irritation and activates diffuse noxious inhibitory controls. The physiological intention of intense TENS is to activate high threshold cutaneous afferents (A-delta) at intensities above pain threshold. High frequency pulses (up to 200 pps) and longer pulse durations that activate small diameter fibres at lower pulse amplitudes are used. Electrodes are positioned in pain-related dermatomes. Intense TENS is delivered for short periods of time for minor procedures such as wound dressing and suture removal.
Mechanism of Action
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree