) The volume of air expired during a period of 1 minute. (The dot above the V represents “time”.)
Orthopnea Severe dyspnea that is relieved when the patient elevates the head and chest.
Oxyhemoglobin Hemoglobin that is fully oxygenated.
Paroxysmal Nocturnal Dyspnea A sudden onset of severe dyspnea when the patient is lying down.
Partial Pressure The pressure exerted by each individual gas when mixed in a container with other gases.
Periodic Breathing A regular waxing and waning of ventilation as a result of fluctuations in the central respiratory drive.
Polycythemia Increased number of red blood cells in the blood.
Rales Short, discontinuous, explosive adventitious sounds, usually called crackles.
Reduced Hemoglobin Hemoglobin in the deoxy state (not fully saturated with oxygen).
Respiration The process by which oxygen and carbon dioxide are exchanged between the outside atmosphere and the cells in the body.
Rhonchi Continuous musical adventitious sounds.
Sleep Apnea Repeated absence of breathing during sleep, sometimes hundreds of times during the night and often for 1 minute or longer.
Tachypnea Increased rate of respirations.
Torr Units of the Torricelli scale, the classic mercury scale, used to express the same value as millimeters of mercury.
Ventilation The mechanical movement of air in and out of the lungs.
Wheeze A high-pitched sibilant rhonchus usually produced on expiration.
Respiratory System Anatomy
The Nose
The nose, the first area in which inhaled air is filtered (Fig. 12.1), is lined with ciliated epithelium. Cilia move mucus and particles of foreign matter to the pharynx to be expectorated or swallowed (Fig. 12.2). Other functions of the nose include humidification and warming of inhaled air and the olfactory function of smell.2
Dry gases are often administered during anesthesia. These gases dry the mucous membranes and slow the action of the cilia. The administration of moist gases in the PACU with various humidification and mist therapy devices keeps this physiologic filter system viable. A tracheostomy precludes the functions of the nose, and proper tracheostomy care, including the administration of humidified oxygen, must be instituted.3
The blood supply to the nose is provided by the internal and external maxillary arteries, which are derived from the external carotid artery, and by branches of the internal carotid arteries. The venous plexus of the nasal mucosa is drained into the common facial vein, the anterior facial vein, the exterior jugular vein, or the ophthalmic vein. A highly vascular plexus of vessels is located in the mucosa of the anterior nasal septum. This plexus is called the Kiesselbach plexus or the Little’s area. In most instances, this area is the source of epistaxis.4
Epistaxis can occur in the PACU after trauma to the nasal veins from nasotracheal tubes or to nasal airways during anesthesia. If epistaxis occurs, prompt action should be taken to prevent aspiration of blood into the lungs. The patient should be positioned with the head up and flexed forward toward the chest. Cold compresses applied to the bridge of the nose and neck may be effective in slowing or stopping the bleeding. If the bleeding is profuse, the oral cavity should be suctioned carefully, and the attending physician should be notified. A nasal pack or cautery with silver nitrate or electric current may be necessary to stop the bleeding.5
The Pharynx
The pharynx originates at the posterior aspect of the nasal cavities and is called the nasopharynx until it reaches the soft palate, where it becomes the oropharynx. The oropharynx extends to the level of the hyoid bone, where it becomes the laryngeal pharynx, which extends caudally to below the hyoid bone.2
The Larynx
The larynx, or voice box (Fig. 12.3), is situated anterior to the third, fourth, and fifth cervical vertebrae in the adult male. It is situated higher in women and children. The larynx consists of nine cartilages held together with ligaments and intertwined with many small muscles. The thyroid cartilage, the largest, is V-shaped; its protruding prominence is commonly referred to as the Adam’s apple. The thyroid cartilage is attached to the hyoid bone by the hyothyroid membrane and to the cricoid cartilage. The cricoid cartilage is situated below the thyroid cartilage and anteriorly forms a signet-shaped ring. The signet lies posteriorly as a quadrilateral lamina joined in front by a thin arch. The inner surface of the cricoid cartilage is lined with a mucous membrane. In children younger than 12 years, the cricoid cartilage is the smallest opening to the bronchi of the lungs.
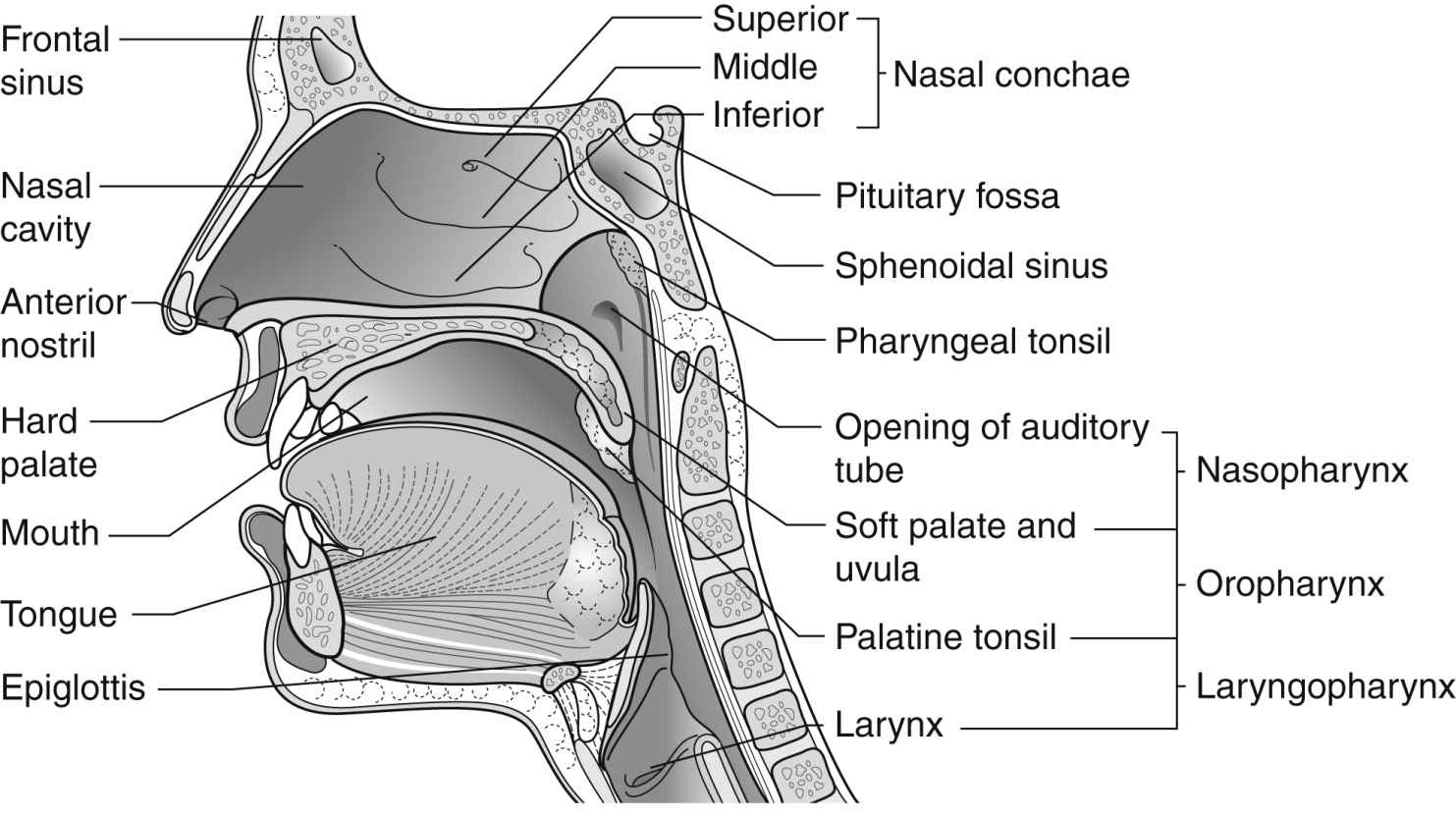
FIG. 12.1 Sagittal section through the nose. (From Watson R: Anatomy and physiology for nurses, ed 13, Edinburgh, UK, 2011, Baillière Tindall.)
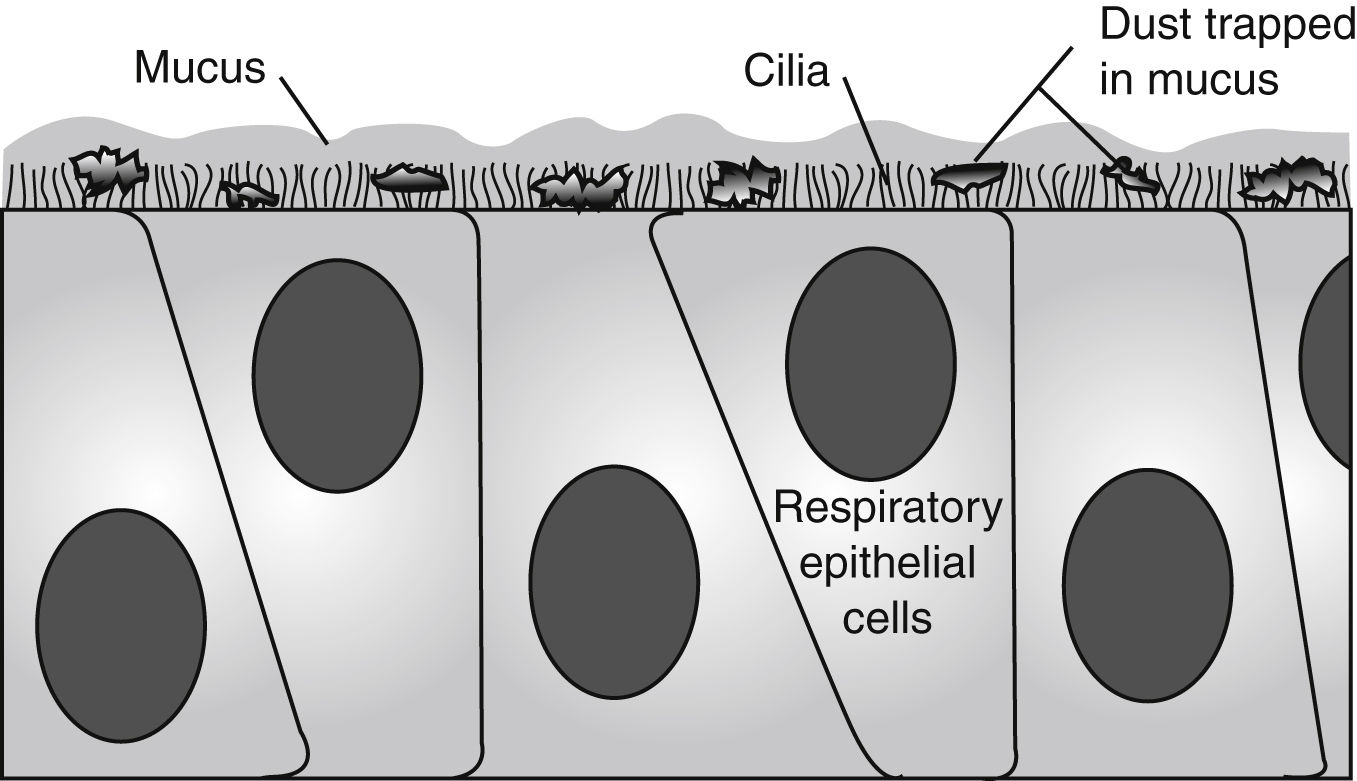
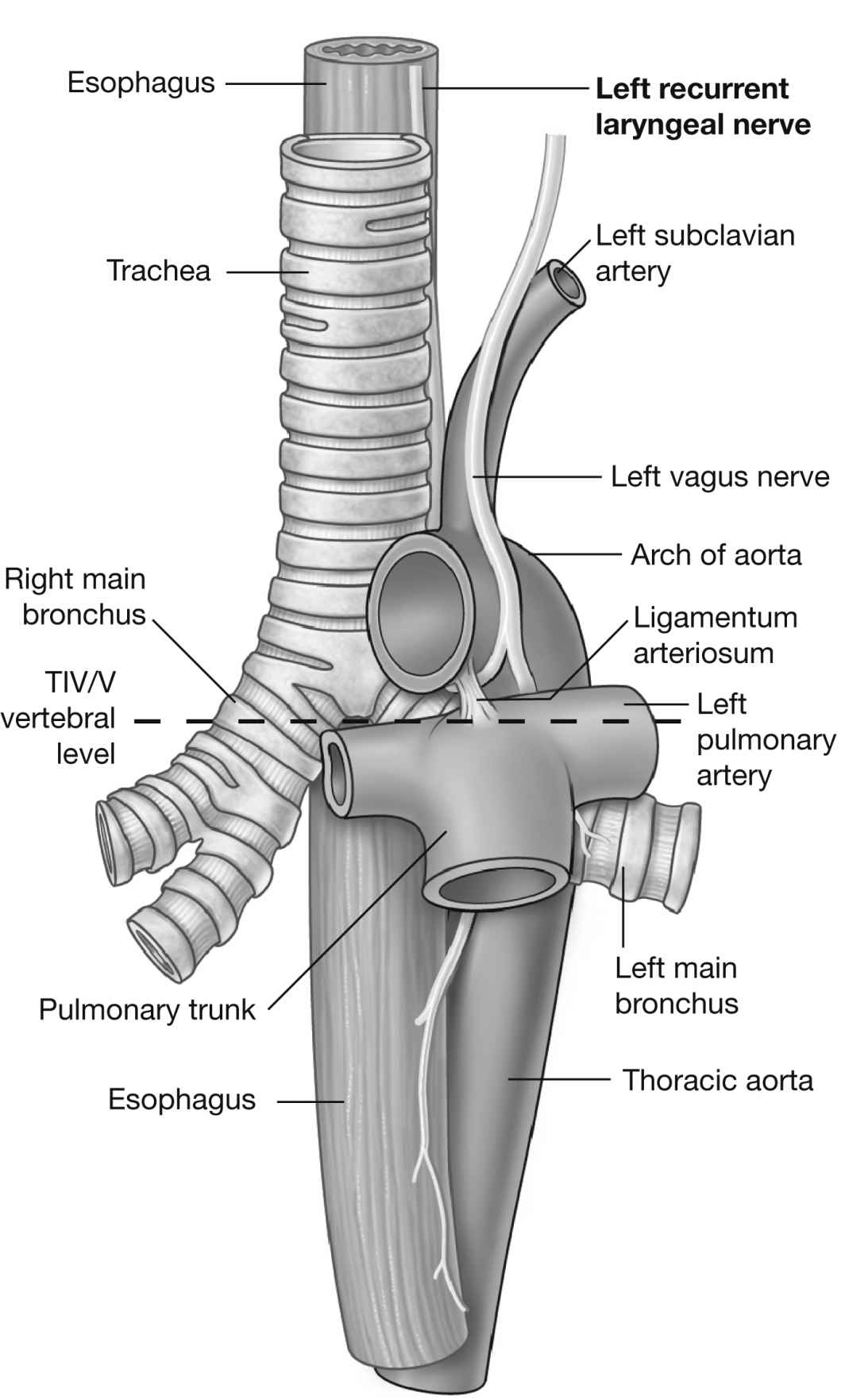
FIG. 12.2 Mucus blanket of nasal airways. Outer (gel-like) layer rests on tips of beating cilia, and inner (water) layer bathes cilia. Particles are trapped on sticky outer blanket and carried posteriorly into nasopharynx by organized beating of cilia. (From Bill RL: Clinical pharmacology and therapeutics for the veterinary technician, ed 3, St. Louis, MO, 2006, Mosby.)
The epiglottis, a cartilage of the larynx, is an important landmark for tracheal intubation that serves to deflect foreign objects away from the trachea. This cartilage is leaf-shaped and projects outward above the thyroid cartilage over the entrance to the trachea. The lower portion is attached to the thyroid lamina, and the anterior surface is attached to the hyoid bone and thereby to the base of the tongue. The valleys on either side of the glossoepiglottic fold are termed the valleculae.6
The arytenoid cartilages are paired and articulate with the lamina of the cricoid through the articular surface on the base of the arytenoid. The anterior angle of the arytenoid cartilage projects forward to form the vocal process. The medial surface of the cartilage is covered by a mucous membrane to form the lateral portion of the rima glottis—that is, the split between the vocal cords. The rima glottis is completed anteriorly by the thyroid cartilage and posteriorly by the cricoid cartilage.
The corniculate cartilages are two small nodules located at the apex of the arytenoid. The cuneiform cartilage is a flake of cartilage within the margin of the aryepiglottic folds. It probably serves to stiffen the folds.
The larynx has nine membranes and extrinsic or intrinsic ligaments. Extrinsic ligaments connect the thyroid cartilage and the epiglottis with the hyoid bone and the cricoid cartilage with the trachea. Intrinsic ligaments connect the cartilages of the larynx with each other.
The fissure between the vocal folds, or true cords, is called the rima glottidis or glottis. In the adult, this opening between the vocal cords is the narrowest part of the laryngeal cavity. Any obstruction in this area leads to death via suffocation if not relieved promptly. The rima glottidis divides the laryngeal cavity into two main compartments: (1) the upper portion is the vestibule, which extends from the laryngeal outlet to the vocal cords and includes the laryngeal sinus, sometimes called the middle compartment and (2) the lower compartment, which extends from the vocal cords to the lower border of the cricoid cartilage and, thereafter, is contiguous with the trachea.7
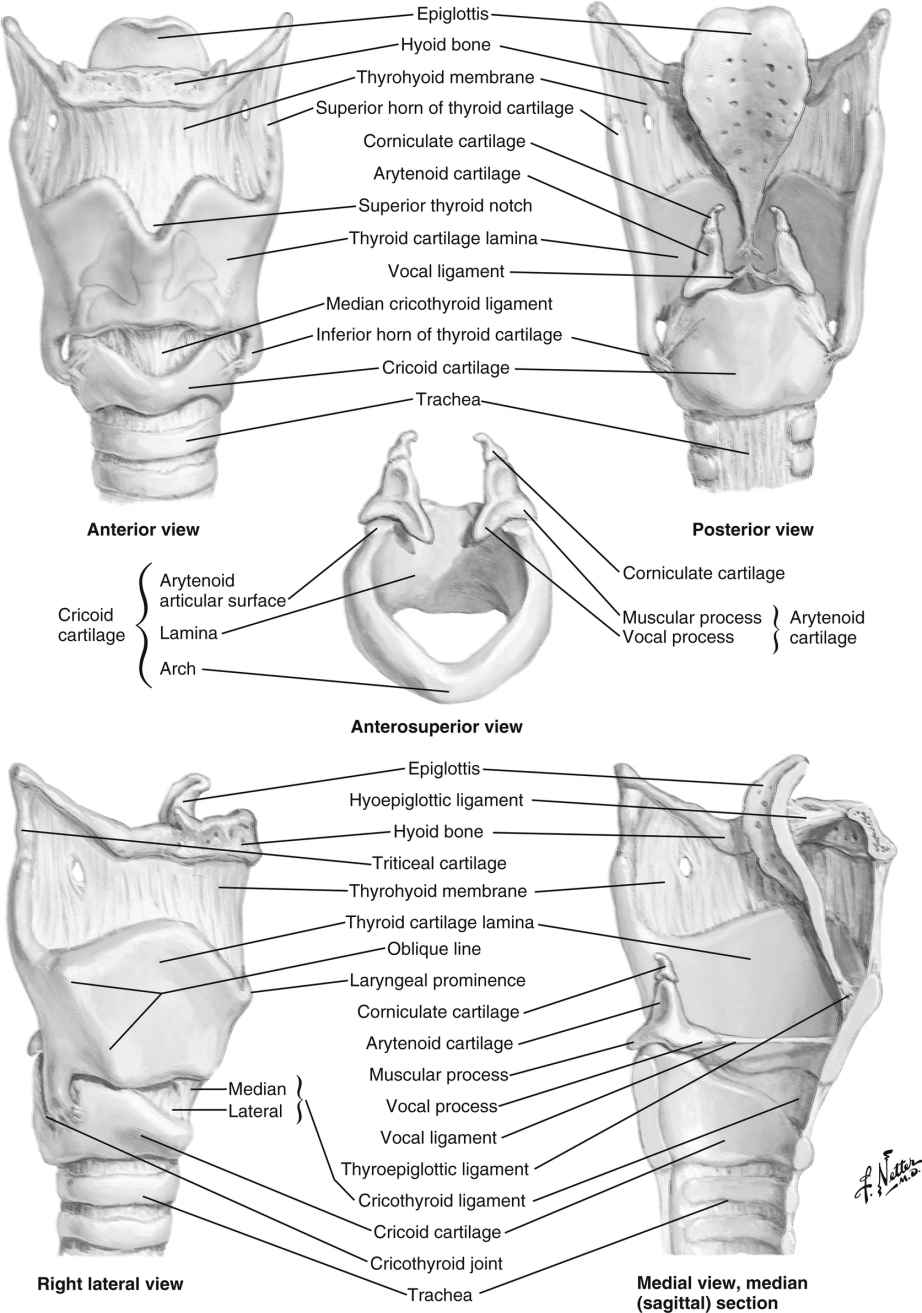
FIG. 12.3 The larynx. (From www.netterimages.com. © Elsevier Inc. All rights reserved.)
The muscles of the larynx are also either intrinsic or extrinsic. The intrinsic muscles control the movements of the laryngeal framework. They open the cords on inspiration, close the cords and the laryngeal inlet during swallowing, and alter the tension of the cords during speech. The extrinsic muscles are involved in the movements of the larynx as a whole, such as when swallowing.5
The nerve supply to the larynx is from the superior and recurrent laryngeal nerves of the vagus. The superior laryngeal nerve passes deep to both the internal and the external carotid arteries and divides into a small external branch that supplies the cricothyroid muscles that tense the vocal ligaments. The larger internal branch pierces the thyrohyoid membrane to provide sensory fibers to the mucosa on both sides of the epiglottis and the larynx above the cords.2
The recurrent laryngeal nerve on the right side exits from the vagus as it crosses the right subclavian artery and ascends to the larynx in the groove between the trachea and esophagus (Fig. 12.4). When the nerve reaches the neck, it assumes the same relationships as on the right. This nerve provides the motor function to the intrinsic muscles of the larynx, with the exception of the cricothyroid, and also provides sensory function to the laryngeal mucosa below the vocal cords.
Laryngospasm, a spasm of the laryngeal muscle tissue, may be complete (with complete closure of the vocal cords) or incomplete (with partial closure of the vocal cords). Patients with partial or complete airway obstruction, such as laryngospasm, usually have a paradoxical rocking motion of the chest wall. This motion can be misinterpreted as normal abdominal breathing. As a result, the perianesthesia nurse should always auscultate the patient’s lungs to determine the degree of ventilation and should not rely on a visual assessment of the chest’s motion.
When a laryngospasm occurs in the PACU, prompt emergency treatment is necessary to save the patient’s life. The perianesthesia nurse should have someone on the PACU staff summon the anesthesia provider when laryngospasm is suspected. Treatment consists of mask ventilation with sustained moderate pressure on the reservoir bag. This maneuver usually helps overcome the partial laryngospasm. Complete laryngospasm not relieved with positive pressure within at least 1 minute necessitates more aggressive treatment. Intravenous (0.5 mg/kg) or intramuscular (1 mg/kg) succinylcholine can be administered to relax the smooth muscle of the larynx. Endotracheal intubation may be necessary.8,9 The nurse must remember that ventilation of the patient’s lungs should be continued until complete respiratory functioning has returned.
The Trachea
The trachea is a musculomembranous tube surrounded by 16 to 20 incomplete cartilaginous rings. These C-shaped rings prevent the collapse of the trachea and maintain free passage of air. The trachea is lined with ciliated columnar epithelium, which aids in the removal of foreign material.
The area at the distal end of the trachea at the point of bifurcation into the right and left main stem bronchi is called the carina (Fig. 12.5). The carina contains sensitive pressoreceptors, which on stimulation (i.e., with an endotracheal tube) cause the patient to cough and “buck.” The angle created at the point of bifurcation into the right and left main stem bronchi is clinically significant to the perianesthesia nurse. This angle varies according to the age and gender of the patient (Table 12.1). The angle at the right main stem bronchus is smaller than the angle at the left main stem bronchus. Foreign material can easily enter the right main stem bronchus at this point. Endotracheal tubes, if advanced too far, usually enter the right main stem bronchus and thereby occlude the left main stem bronchus. As a result, the left lung cannot be ventilated. Signs of this complication include decreased or absent breath sounds in the left side of the chest, tachycardia, and uneven expansion of the chest on inspiration and expiration.6,10,11
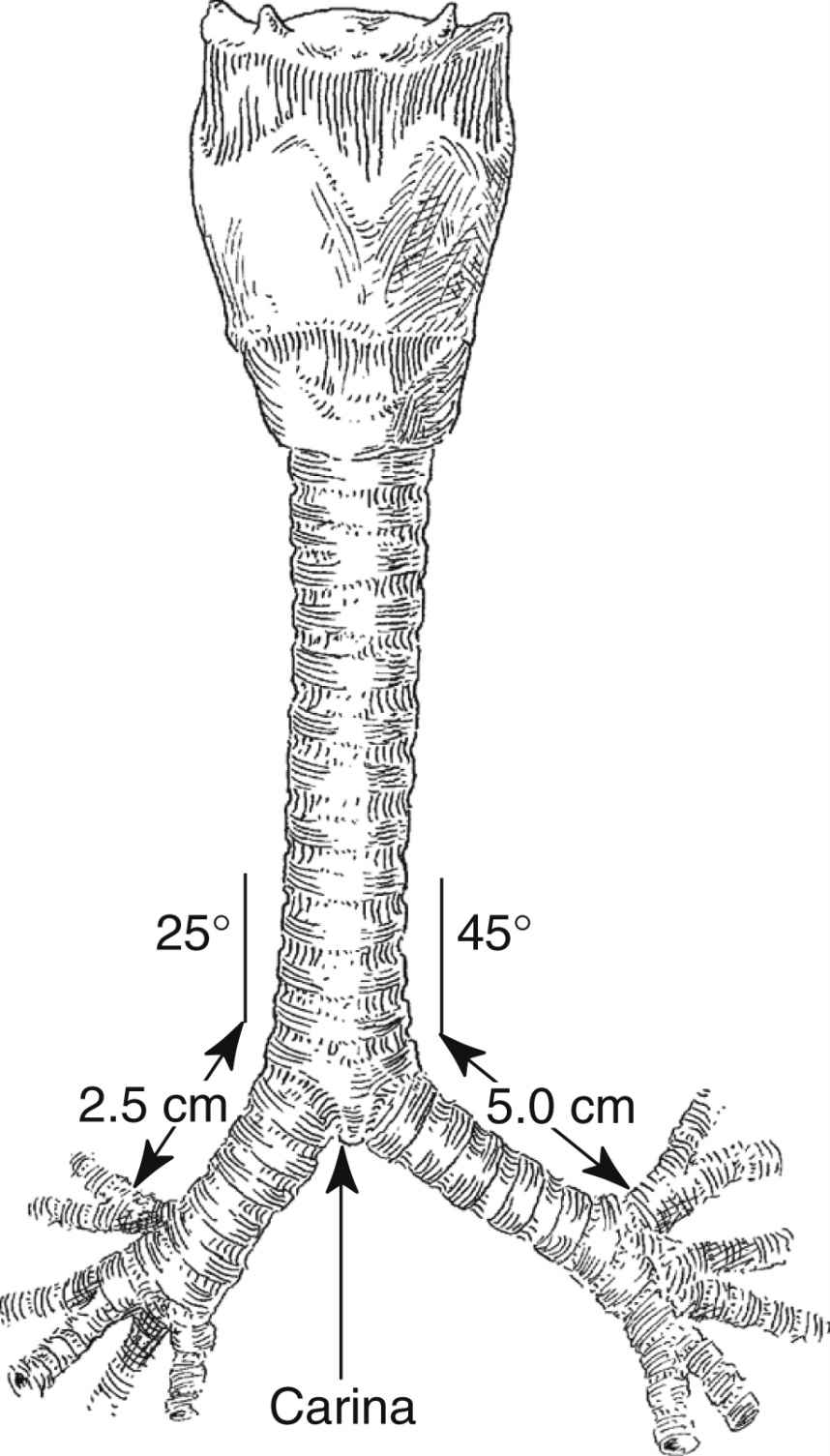
FIG. 12.5 Bifurcation of trachea into main stem bronchi. (From Nagelhout JJ, Plaus KL: Nurse anesthesia, ed 4, St. Louis, MO, 2010, Saunders.)
Bronchi and Lungs
Each primary bronchus supplies a number of lobar bronchi (Fig. 12.6). Humans have an upper, middle, and lower lobe bronchus on the right and only an upper and lower lobe bronchus on the left. Within each pulmonary lobe, a lobar (secondary) bronchus soon divides into tertiary branches that are remarkably constant as to number and distribution within the lobe. The segment of a lobe aerated by a tertiary bronchus is usually well delineated from adjoining segments by complete planes of connective tissue. These areas of the lung are well defined; therefore, pulmonary diseases may be limited to a particular segment or segments of a lobe.
The bronchi bifurcate 22 or 23 times from the main stem bronchus to the terminal bronchi.4 These bronchi have connective tissue and cartilaginous support. The terminal bronchi branch to the bronchioles with a diameter of 1 mm or smaller and lack cartilaginous support. Bronchioles have thin, highly elastic walls composed of smooth muscle, which is arranged circularly. When the circular smooth muscle is contracted, the bronchiolar lumen is constricted. This circular smooth muscle is innervated by the parasympathetic nervous system (vagus nerve), which causes constriction, and the sympathetic nervous system, which causes dilatation. Therefore, the patency of the terminal bronchioles is determined by the tonus of the muscle produced by a balance between the two components of the nervous system. Bronchospasm occurs when the smooth muscles constrict or experience spasm, ultimately leading to airway obstruction.
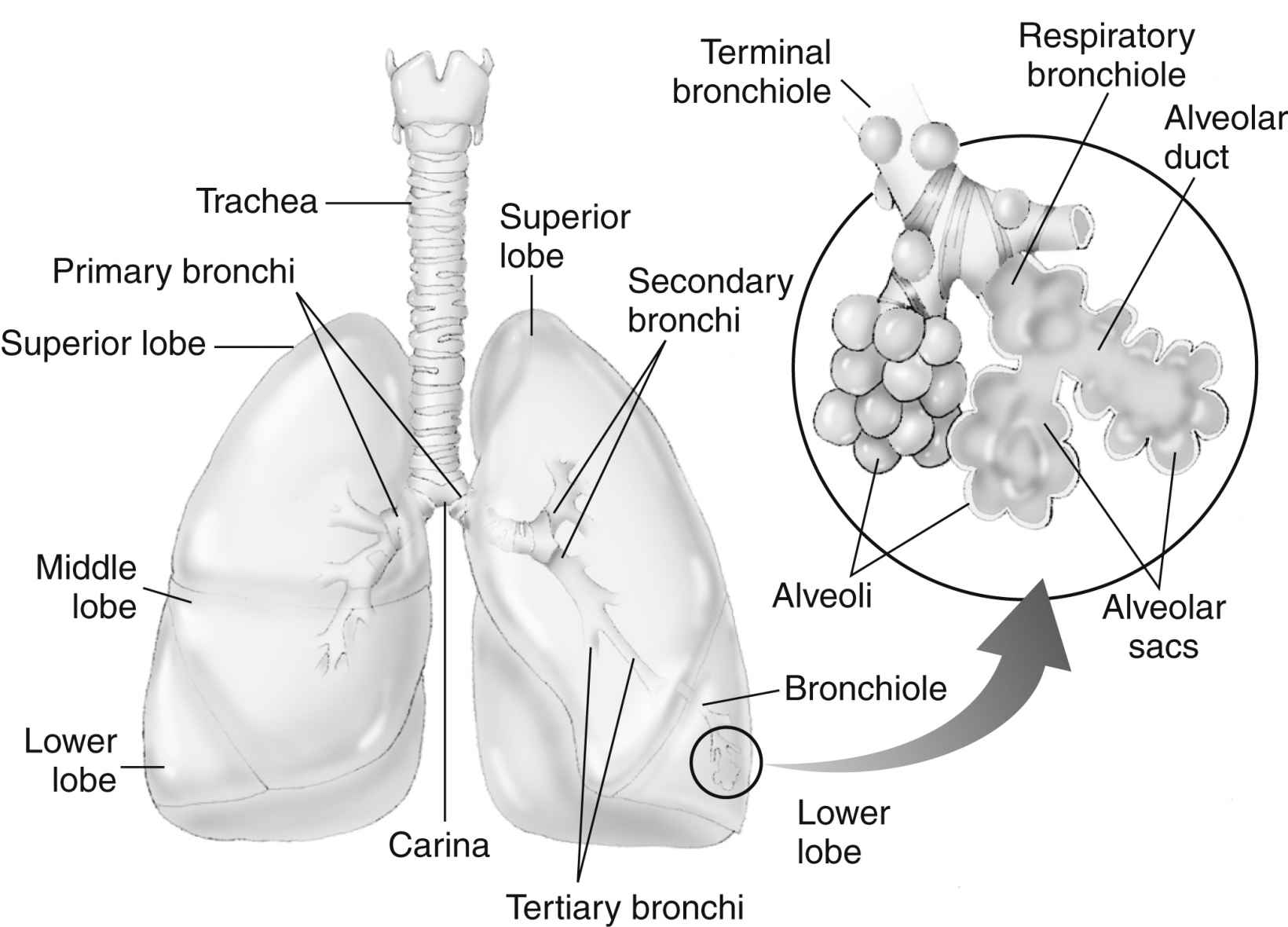
FIG. 12.6 Distribution of bronchi within lungs. Enlarged inset shows detail of alveolus. (From National Association of Emergency Media: PHTLS prehospital trauma life support, ed 6, St. Louis, MO, 2007, Mosby.)
The terminal bronchioles divide into the respiratory bronchioles in which actual gas exchange first occurs. The respiratory bronchioles bifurcate to form alveolar ducts, and these in turn terminate in spherical enclosures called the alveolar sacs. The sacs enclose a small but variable number of terminal alveoli.4
The number of alveoli in an average adult’s lungs is estimated to be 750 million. The surface area available for gas exchange is approximately 125 m2. Alveoli are shaped like soap bubbles in a glass. The interalveolar septum has a supporting latticework composed of elastic collagenous and reticular fibers. The capillaries are incorporated into and supported by the fibrous lattice. The capillary networks in the lungs are the richest in the body.
The lungs receive unoxygenated blood from the left and right pulmonary arteries, which originate from the right ventricle of the heart. The divisions of the pulmonary artery tend to follow the bifurcations of the airway. Typically, two pulmonary veins exit from each lung, and all four veins empty separately into the left atrium. The blood arriving in the rich pulmonary capillary network from the pulmonary arteries provides for the metabolic needs of the pulmonary parenchyma. Other portions of the lungs, such as the conducting vessels and airways, need their own private circulation. The bronchial arteries, which arise from the aorta, provide oxygenated blood to the lung tissue. The blood of the bronchial arteries returns to the heart by way of the pulmonary veins.4
Each lung is contained in a thin elastic membranous sac called the visceral pleura, which is adherent to the external surface of the lung. Another membrane, the parietal pleura, lines the chest wall. These two membranes normally are close to each other. A few milliliters of viscous fluid are secreted between them for lubrication. The visceral pleura continuously absorbs this fluid.
Respiratory System Physiology
Lung Volumes and Capacities
Perianesthesia care of the patient is largely based on knowledge of the physiology and pathophysiology of the respiratory system. Dysfunction in lung volumes and capacities that occurs in the patient after surgery is the compelling reason for institution of the stir-up regimen in the PACU. Accordingly, the physiology of the lung volumes, capacities, and mechanics are described in detail. Table 12.2 provides the definition and normal value for each lung volume and capacity. As shown in Table 12.2 and Fig. 12.7, a lung capacity comprises two or more lung volumes.
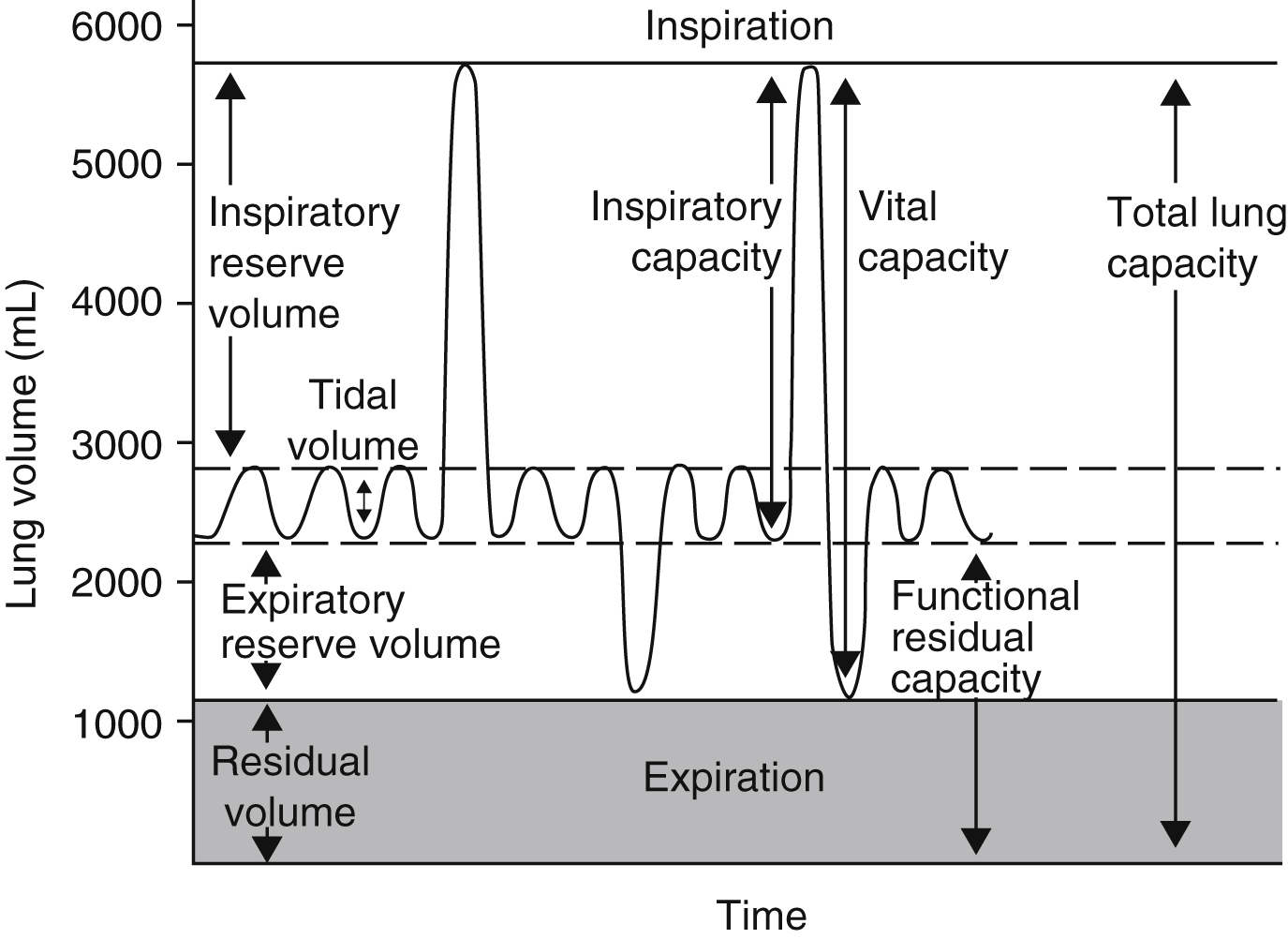
FIG. 12.7 Graphic representation of normal lung volumes and capacities. (From Hall JE: Guyton and Hall textbook of medical physiology, ed 13, Philadelphia, PA, 2016, Elsevier.)
Lung Volumes
The tidal volume (VT) represents the amount of air moved into or out of the lungs during a normal ventilatory excursion. Monitoring of this lung volume is important when the patient receives ventilatory support. Because the VT measurement is highly variable, it is not an extremely helpful parameter in pulmonary function tests. Clinically, the VT can be estimated at 7 mL/kg. For example, a man who weighs 70 kg has a VT of approximately 490 mL (7 × 70 = 490).
The expiratory reserve volume (ERV) is the maximal amount of air that can be expired from the resting position after a normal spontaneous expiration. The ERV reflects muscle strength, thoracic mobility, and a balance of forces that determine the resting position of the lungs and chest wall after a normal expiration. This lung volume is usually decreased in patients who are morbidly obese (see Chapter 45). This lung volume also is decreased in the immediate postoperative period in patients who have undergone an upper abdominal or thoracic operation.6,10,11
The residual volume (RV) is the volume of air that remains in the lungs at the end of a maximal expiration. This lung volume represents the balance of forces of the lung elastic forces and thoracic muscle strength. Patients with skeletal muscle relaxant that was not adequately reversed at the end of the anesthetic period may have an elevated RV because not enough muscle strength can be generated to force all the air out of the lungs. As the RV increases, more air remains in the lungs so it does not participate adequately in gas exchange and becomes dead-space air. As the dead-space volume of air increases, it can impinge on the VT, and hypoxemia can ensue. The importance of the RV is that it allows for continuous gas exchange throughout the entire breathing cycle by providing air to most of the alveoli, and it aerates the blood between breaths. Consequently, the RV prevents wide fluctuations in oxygen and carbon dioxide concentrations during inspiration and expiration.5
The inspiratory reserve volume (IRV) reflects a balance of the lung elastic forces, muscle strength, and thoracic mobility. The IRV is the maximal volume of air that can be inspired at the end of a normal spontaneous inspiration. Physiologically, the IRV is available to meet increased metabolic demand at a time of excess physical exertion. It assists in moving a larger volume of air into the alveoli through each ventilatory cycle, increasing the overall performance and efficiency of the respiratory system.
Lung Capacities
The inspiratory capacity (IC) is the maximal volume of air that can be inspired from the resting expiratory position. The IC is the sum of the VT and the IRV.
The functional residual capacity (FRC) represents the previously mentioned resting position. The FRC is the volume of air remaining in the lungs at the end of a normal expiration when no respiratory muscle forces are applied. At FRC, the mechanical forces of the lung and thorax are at rest and no airflow is present. Because the FRC is usually reduced in patients recovering from anesthesia, this particular lung capacity is of great importance to the perianesthesia nurse when intensive nursing care is rendered. For this reason, breathing maneuvers, such as the sustained maximal inspiration (SMI), are instituted in the PACU to raise the FRC (see the next section on lung mechanics). The FRC represents the sum of the ERV and the RV. A severe increase in the FRC is often associated with pulmonary distention, which is technically a state of hyperinflation of the lung. This state of hyperinflation can be caused by two abnormal conditions: airway obstruction and loss of elasticity. Airway obstruction is exemplified by an episode of acute bronchial asthma; a loss of lung elasticity is usually associated with emphysema. A severe decrease in FRC is associated with pulmonary fibrosis and can be the sequela of postoperative atelectasis.
The vital capacity (VC) is the amount of air that can be expired after the deepest possible inspiration. The VC is the sum of the VT, the ERV, and the IRV. The VC measures many factors that simultaneously affect ventilation, including activity of respiratory centers, motor nerves, and respiratory muscles, and thoracic maximum, airway and tissue resistance, and lung volume. The total lung capacity (TLC) is the total amount of air in the lung at a maximal inspiration. The TLC is the sum of the VC and the RV.
Clinical measurements of the TLC, FRC, and RV are difficult because these values include a gas volume that cannot be exhaled; therefore, the measurements require sophisticated pulmonary function testing equipment with gas dilution techniques or plethysmography. Measurements of lung volumes and capacities are useful in the evaluation of lung function.6
Lung Mechanics
Mechanical Features of the Lungs
Mechanical forces of the respiratory system actually determine the lung volumes and capacities. For an understanding of how these lung volumes and capacities are determined and how they are affected by anesthesia and surgery, the perianesthesia nurse should become familiar with the balance-of-forces concept of the respiratory system (see the section on combined mechanical properties of the lungs and chest wall). The PACU stir-up regimen is designed to increase the postoperative patient’s lung volumes and capacities with enhancement of the mechanical forces of the respiratory system.
The lungs and chest wall are viscoelastic structures, one within the other. Because they are elastic, the lungs always want to collapse or recoil to a smaller position. Therefore, as can be seen in the pressure-volume (P-V) curve of the lungs alone (Fig. 12.8), at less than RV the lungs are collapsed and no pressure is transmitted across the lungs (i.e., no transpulmonary pressure). When the lungs are inflated to a volume halfway between RV and TLC, the lungs seek to recoil or collapse back to the resting position equal to or less than RV, which is reflected by an increase in transpulmonary pressure. When the lungs are fully inflated at TLC, a maximal transpulmonary pressure is also exhibited. By analogy, when a balloon is completely deflated, the pressure measured at the mouth of the balloon is zero. When the balloon is partially inflated, the pressure increases as the elastic forces of the balloon try to make the balloon recoil to its resting position. If the balloon is maximally inflated, the elastic recoil of the balloon is greater as is the pressure measured at the mouth of the balloon.
Pulmonary Hysteresis
Inflation and deflation paths of the P-V curve of the lung are not aligned on top of each other (Fig. 12.9). The path of deformation (inspiration) to TLC is different from the path followed when the force is withdrawn (expiration) from TLC to RV. This phenomenon is known as pulmonary hysteresis. The following factors contribute to pulmonary hysteresis: properties of the tissue elements (a minor factor), recruitment of lung units, and the surface tension phenomenon (surfactant).2
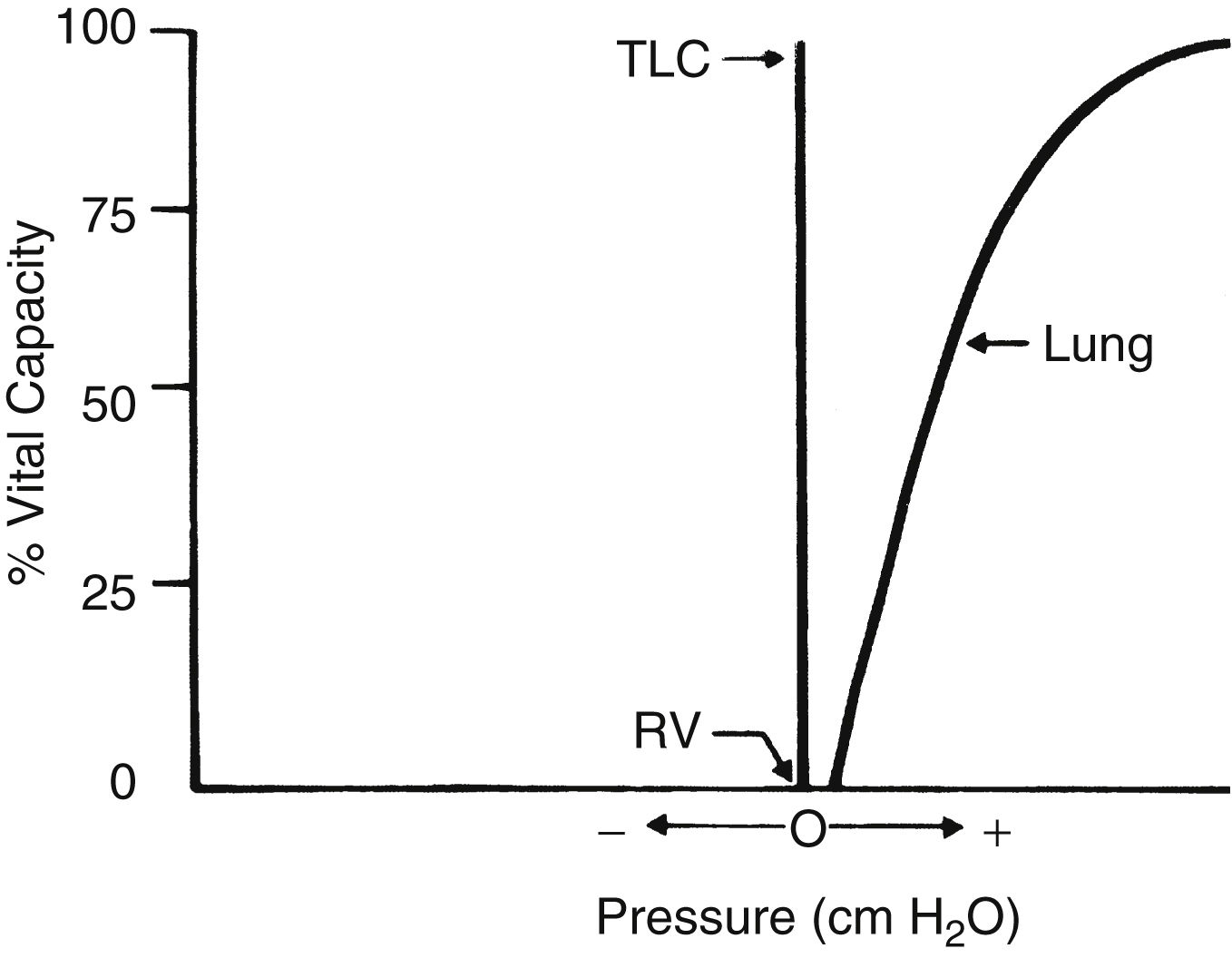
FIG. 12.8 Static deflation pressure-volume curve for lung. Positive pressures represent pressures that tend to decrease lung volume. TLC, Total lung capacity; RV, residual volume. (From Drain C: Physiology of the respiratory system related to anesthesia. CRNA 7:163–180, 1996.)
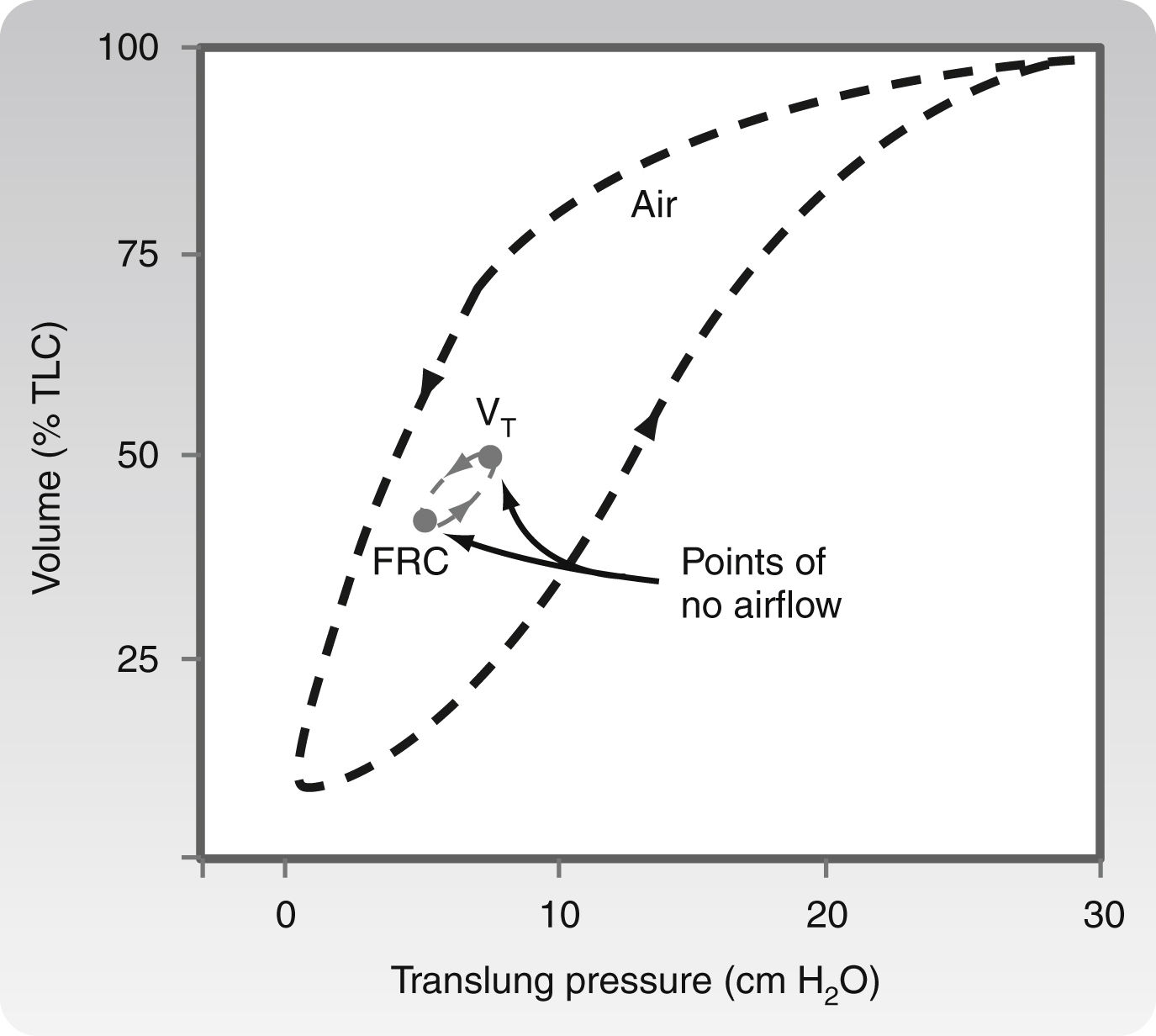
FIG. 12.9 Inflation and deflation paths of pressure-volume curve of lungs. (From Koeppen BM, Stanton BA: Berne and Levy’s physiology, ed 6 [updated edition], St. Louis, MO, 2010, Mosby.)
Elastic Properties of the Lung
The elastic properties of the lung tissue contribute only a small part to the phenomenon of hysteresis. Other properties of the lung tissue contributing to hysteresis are the recruitment of lung units, surface tension of the alveolar unit, and the lung capacities. These components will be discussed in detail in the following section.
Recruitment of Lung Units
Recruitment of lung units has an important role in pulmonary hysteresis. For an understanding of recruitment of lung units, the nurse must be familiar with the concept of airway closure. An apex-to-base gradient of alveolar size exists in the lung (Fig. 12.10). This gradient occurs because of the weight of the lung, which tends to pull the lung toward its base. As a result, the pleural pressure is more negative at the apex than at the base of the lung. Ultimately, at low lung volumes, the alveoli at the apex are more inflated than the alveoli at the base. At the base of the lungs, some alveoli are closed to ventilation because the weight of the lungs in that area causes the pleural pressure to become positive. Airways open only when the critical opening pressure is achieved during inflation and the lung units peripheral to them are recruited to participate in volume exchange. This process is called radial traction or a tethering effect on airways. An analogy of a nylon stocking can aid in the explanation of this concept. When no traction is applied to the nylon stocking, the holes in the stocking are small. As traction is applied to the stocking from all sides, each nylon filament pulls on the others, which spreads apart all the other filaments and the holes in the stocking enlarge. Similarly, as one airway opens, it produces radial traction on the next airway and pulls the next airway open; in other words, it recruits airways to open. The volume of air in the alveoli behind the closed airways is termed the closing volume (CV). The CV plus the RV is termed the closing capacity (CC). The CC normally occurs at less than the FRC.6
During the early emergence phase of anesthesia, patients usually have low lung volumes, which can lead to airway closure. Consequently, a postoperative breathing maneuver that has a maximal alveolar inflating pressure, a long alveolar inflating time, and high alveolar inflating volume, such as the SMI or yawn maneuver, should be used to facilitate the maximal recruitment of lung units. With the recruitment of lung units, the FRC could be raised out of the CV range and, ultimately, hypoxemia could be reduced.
Surface Tension Phenomenon
The surface tension phenomenon relates to the action of surfactant on lung tissue. Surfactant is a phospholipid rich in lecithin produced by the type II alveolar cells. Surfactant lines the alveolus as a thin surface-active film. This film has a physiologic action of reducing the surface tension of the alveoli and terminal respiratory airways. If the surfactant were not present, the surface tension would be fixed, and greater pressure would be needed to keep the alveolus open. As a result, small alveoli would empty into larger ones, atelectasis would regularly occur at low lung volumes, and large expanding pressures would be necessary to reopen collapsed lung units. Surfactant is also an important factor in alveolar inflation because it provides uniformity in the inflation of lung units. In these ways, surfactant helps impart stability to alveoli in the normal lung. In addition to a major role in pulmonary hysteresis, surfactant also contributes to lung recoil and reduces the workload of breathing.9
Lung Compliance
Several other terms that relate to the P-V curve of the lung deserve attention. One term is lung compliance (CL), which is defined as the change in volume for a given change in pressure or the pressure needed for maintenance of a given volume of inflation. The normal value for CL is 0.1 L per cm H2O.
CL=ΔVΔP

where V represents volume and P represents pressure.
CL is a measurement of the distensibility of the lungs during breathing. According to convention, CL means the slope on the static deflation portion of the P-V curve over the VT range; therefore, CL can be said to be the slope of the P-V curve, and it may remain unchanged even if marked changes in lung elastic properties cause a shift of the P-V curve to the left or right. As a result, clinical measurement of CL is done over the VT range during deflation. Measurement of the CL over any other portion of the P-V curve can result in an inaccurate reading compared with a normal value. Lung elastic recoil (PstL) is the pressure exerted by the lung (transpulmonary pressure) because of its tendency to recoil or collapse to a smaller resting state. At low lung volumes, the PstL is low; at high lung volumes, the PstL is high. This elastic retractive force (i.e., PstL) is the result of the overall structural elements of the lung combined with the lung surface tension forces. As mentioned previously, the CL represents the slope of the P-V curve, and the PstL represents the points along the P-V curve. Changes in CL and PstL have dramatic implications in the alteration of lung volumes that occurs in the immediate postoperative period (see the section on postoperative lung volumes).6
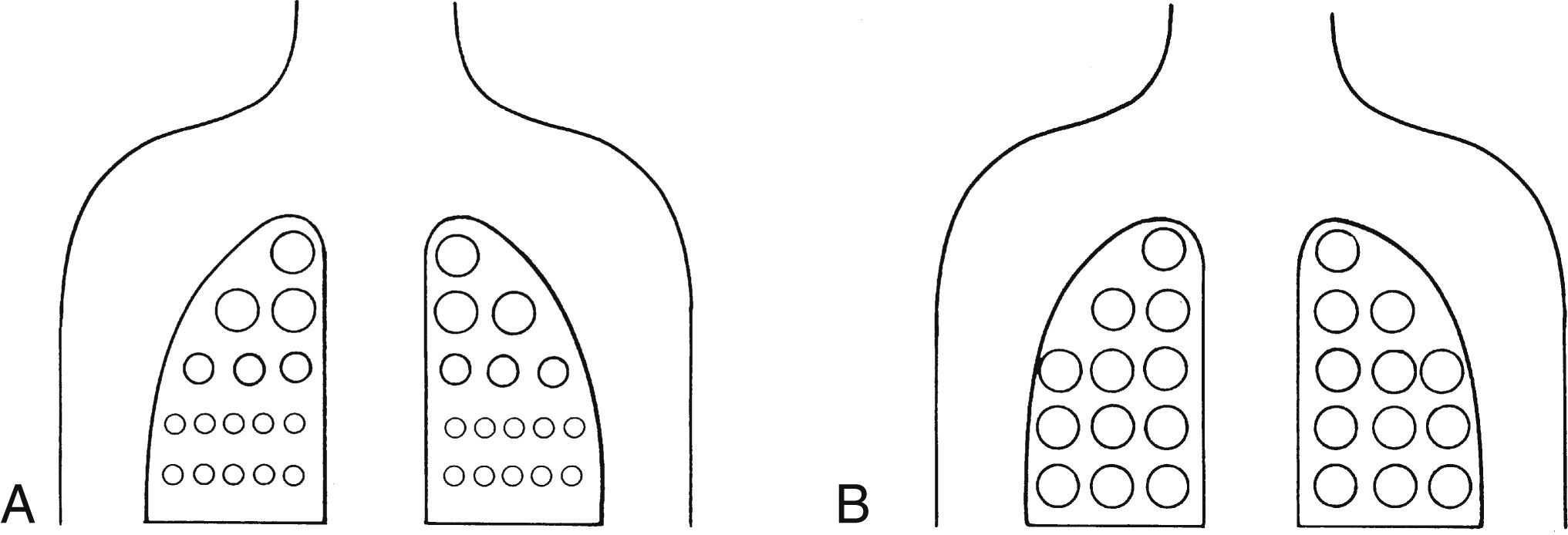
FIG. 12.10 A, Alveolar size from apex to base of lungs as subject inhales from residual volume to B, total lung capacity.
Equal Pressure Point
The equal pressure point (EPP) has many clinical implications to perianesthesia practice. More specifically, intraoperative and postoperative mechanical ventilations, along with pursed lips and abdominal breathing of the patient with compliant airways, are based on this concept.
The alveoli and airways can be imagined as a balloon in a box (Fig. 12.11). Flow out of the balloon is facilitated by the recoil of the balloon, which forces the air out of the balloon through the neck and out into the atmosphere. The addition of pressure all over the box forces the air out of the balloon at a higher rate of flow. Physiologically, the balloon recoil is analogous to the alveolar recoil pressure. The pressure pushing down on the balloon and its neck corresponds to a positive pleural pressure generated on a forced expiratory maneuver. For the air to move out of the alveoli, the alveolar pressure must exceed the pressure at the mouth. The pressure inside the neck of the balloon corresponds to the intraluminal airway pressure. Consequently, the alveolar pressure comprises the recoil pressure of the alveoli and the pleural pressure. Also, the pressure to generate airflow decreases down the airway to the mouth (see Fig. 12.11). During a forced expiratory maneuver, the pleural pressure pushes down on the alveoli and the airways. If the alveolar recoil pressure is 30 and the pleural pressure is 20, the alveolar pressure is 50. The pressure inside the airway (intraluminal pressure) decreases progressively downstream toward the mouth. The EPP occurs when the intraluminal pressure is equal to the pleural pressure (20 = 20); from that point, the pleural pressure exceeds the intraluminal pressure, and dynamic compression of the airway occurs. Total collapse of the airways from the EPP and the mouth does not normally occur because of the compliance of the airways. Physiologically, the dynamic compression reduces the airways’ radius and thus results in an increase in flow rates in the compressed area that aids physiologic mechanisms, such as the cough maneuver, to sheer and expel secretions and mucus out of the airways.6
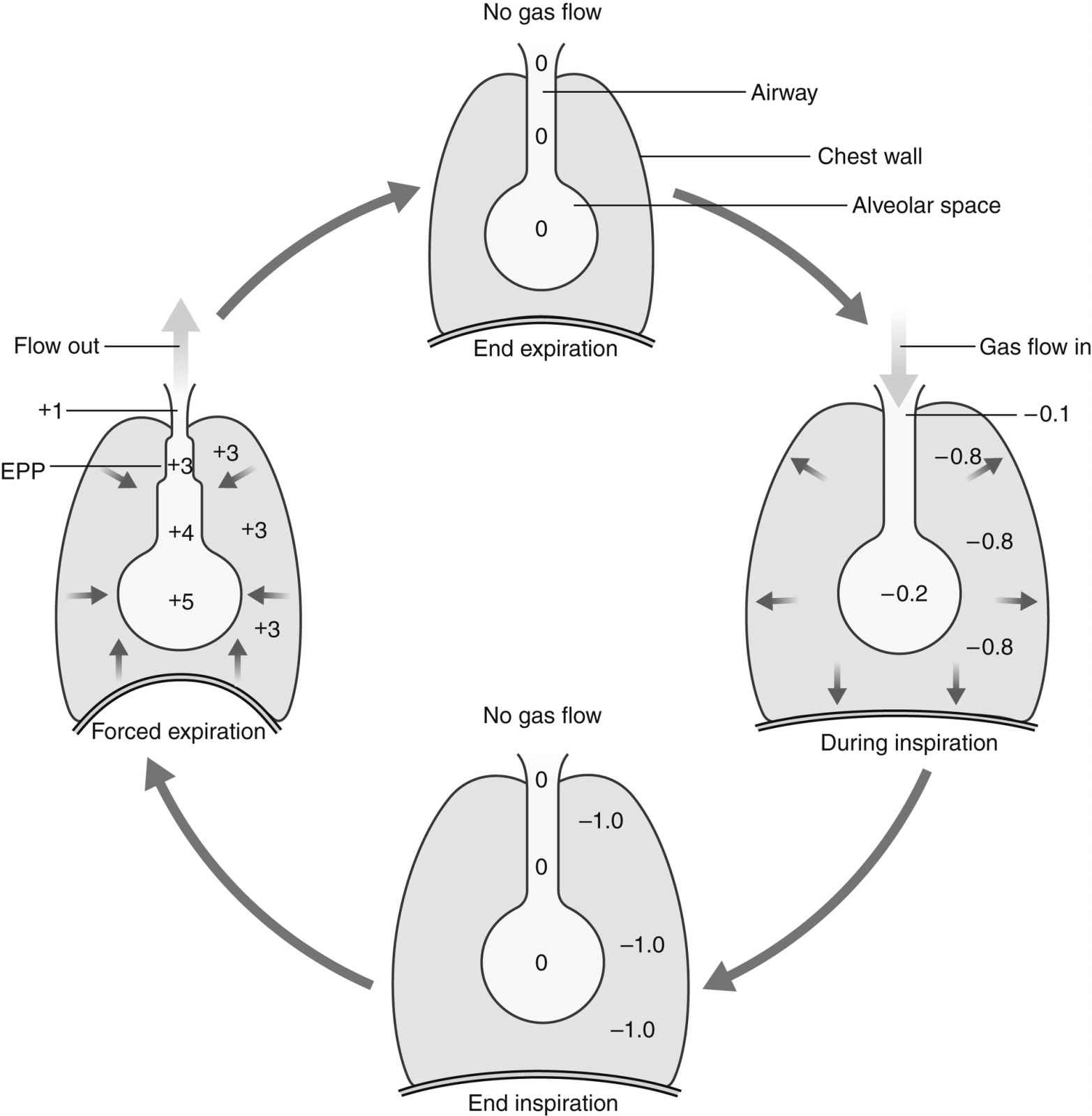
FIG. 12.11 Pressure changes in the chest and lung during inspiration and forced expiration. The pleural pressure around the airways is usually negative (less than atmospheric). During inspiration, the chest wall expands, and there is a greater negative pleural pressure, drawing air into the airways. At forced expiration, the pleural pressure may become positive, forcing air out. The equal pressure point (EPP) is where airway pressure equals pleural pressure. (From Naish J, Court DS: Medical sciences, ed 2, St. Louis, MO, 2015, Saunders.)
In the patient with highly compliant airways (i.e., with chronic obstructive pulmonary disease), the dynamic compression can completely close the airways. The trapped air increases the FRC and becomes dead space. The harder the patient tries to expel air, the greater the pleural pressure becomes and more dynamic compression occurs; thus a vicious cycle ensues. Interventions to help these patients move air out of the lungs are focused on a reduction of the amount of dynamic compression on the airways. The interventions are to increase the expiratory time and provide physiologic positive end-expiratory pressure (PEEP). Lengthening of the expiratory time aids in the reduction of the amount of positive pleural pressure on the airways, and physiologic PEEP enhances the airway’s intraluminal pressure in the highly compliant airways. In the awake patient with highly compliant airways, abdominal breathing prolongs the expiratory time, and pursed-lip breathing provides physiologic PEEP. In the patient who is anesthetized, prolonging the expiratory time (i.e., inspiration:expiration ratio of 1:3) on the ventilator and use of physiologic PEEP (i.e., 5 cm H2O) aids in moving air out of the airways.
Pulmonary Time Constant
The pulmonary time constant is similar to the half-life used in the assessment of the pharmacokinetic activity of drugs. A time constant represents the amount of time necessary for flow to decrease by a rate equal to half the initial flow. A time constant equals the resistance multiplied by the compliance. Therefore, the time necessary to reach each time constant depends on the individual values of resistance and compliance. In normal conditions, the decrease in flow at the first time constant is approximately 37% of the initial flow or approximately 63% of the total volume added or removed from the lungs. The first time constant represents the time necessary for removing or adding 63% of the total volume of air in the lungs. The decrease in flow rate at the second time constant is approximately 14%, and the percent volume of air added or removed from the lungs is 86%. The decrease in flow at the third time constant is 5% with a corresponding 95% volume added or removed; therefore, the higher the time constant, the more air is removed or added to the lungs.5
The clinical implications of time constants are extremely important in the perianesthesia care of patients who have received an inhalation anesthetic. Patients who have increased airway resistance, increased CL, or both have a prolonged time necessary for filling and emptying of the lungs. The lung units in this situation are referred to as slow lung units. The patient with slow lung units usually has chronic obstructive pulmonary disease. Patients with a significant amount of increased secretions also have some slow lung units. Consequently, patients with slow lung units usually have a slow emergence from inhalation anesthesia. Patients with a low CL, such as patients with pulmonary fibrosis, have fast lung units. As a result, these patients can fill or empty the lungs rather rapidly and have a rapid emergence from inhalation anesthesia.
Mechanical Features of the Chest Wall
Because of its elastic properties, the chest wall always springs out or recoils outward, seeking a larger resting volume. The resting volume of the lungs alone is less than the RV, and the resting volume of the chest wall is approximately 60% of the VC.
The action of the chest wall can be illustrated with the analogy of a wire screen attached around a balloon. The wire screen tends to spring outward so the screen pulls the balloon open at lower balloon volumes. A measure of the pressure at the mouth of the balloon reflects a negative number. At approximately 60% of the total capacity of the balloon, the screen no longer tends to spring outward. At that point, the addition of air causes the screen to push down on the balloon—a reflection of a positive pressure at the mouth of the balloon. The screen around the balloon can be likened to the chest wall. As shown in Fig. 12.12, at lower lung volumes, the chest wall clearly is inclined to recoil outward, thus creating a negative pressure. At approximately 60% of the VC, the chest wall starts to push down on the lungs, thus creating a positive pressure. The result of the interplay between the chest wall’s strong tendency to spring outward and the lung’s strong tendency to recoil inward is the subatmospheric pleural pressure.6
Pleural pressure can become positive during a cough or other forced expiratory maneuvers. Pneumothorax can occur when the chest wall is opened or when air is injected into the pleural cavity. With this occurrence, the lungs collapse because they naturally recoil to a smaller position; the ribs flare outward because of their natural inclination to recoil outward. Clinically, inspection of a patient with a pneumothorax may reveal protruding ribs on the affected side.
The two types of pneumothoraces are open (simple) and closed (tension). Simple pneumothorax occurs when airflow into the pleural space results in a positive pleural pressure. The lungs collapse because the recoil pressure is not counterbalanced with negative pleural pressure. Treatment for a pneumothorax can be conservative or more aggressive depending on the type and amount of pneumothorax. Aggressive treatment consists of the insertion of chest tubes into the pleural space to recreate the negative pleural pressure. This maneuver reestablishes normal ventilatory excursions. In most instances, the air leak between the lung and the pleural space seals after the chest tubes have been removed. If air continues to flow into the intrapleural space but cannot escape, the intrapleural pressure continually increases with each succeeding inspiration. Like a one-way valve, pressure increases, and a tension pneumothorax develops. In a brief period, as the intrapleural pressure increases, the affected lung is compressed and puts a great amount of pressure on the mediastinum. Hypoxemia and reduction in cardiac output result, and if treatment is not instituted immediately, the patient may die. Treatment consists of immediate evacuation of the excess air from the intrapleural space with either chest tubes or a large-bore needle. A tension pneumothorax is truly a medical emergency.3
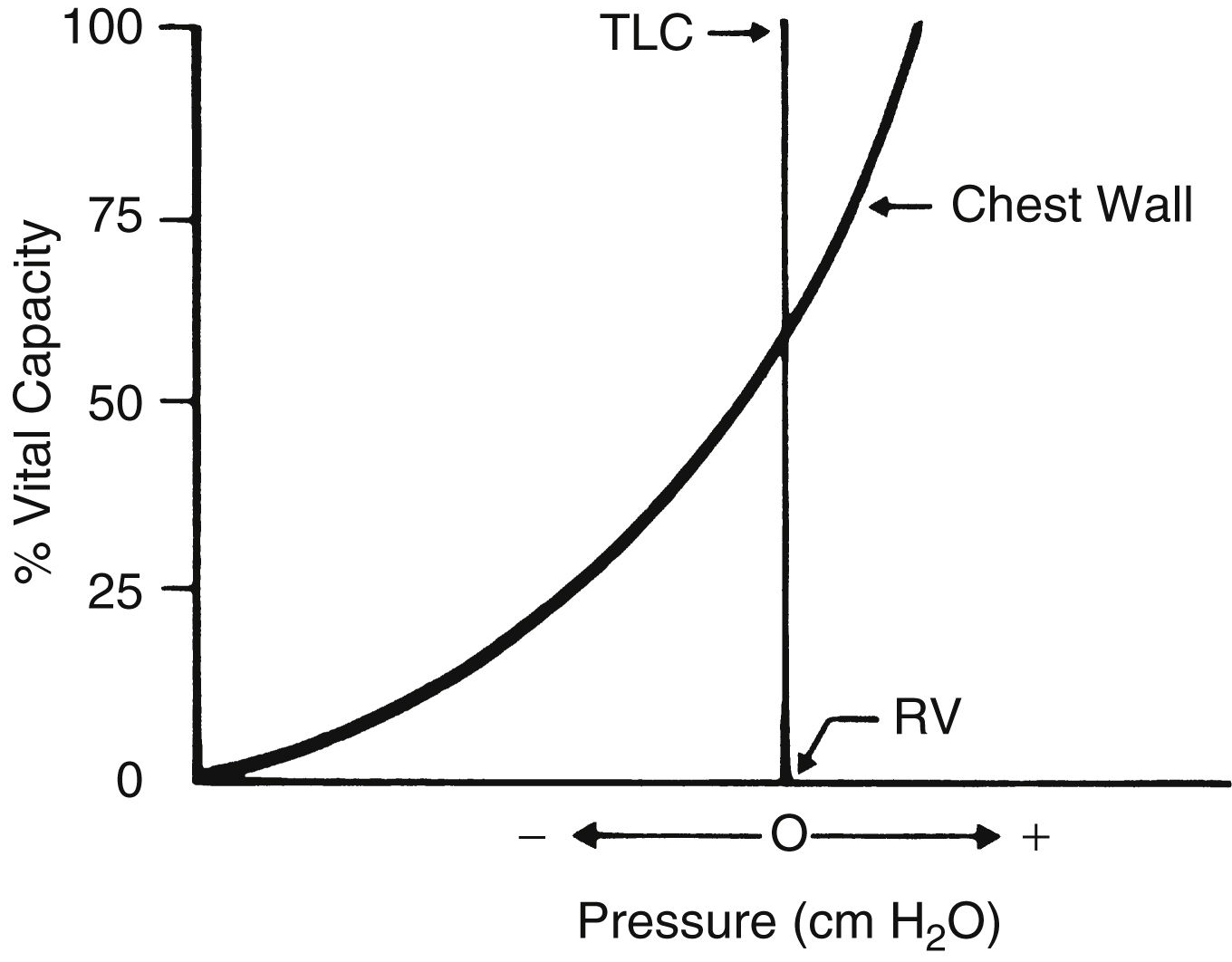
FIG. 12.12 Pressure-volume curve of chest wall during deflation going from TLC to RV. Positive pressures of the chest wall represent pressures that tend to decrease lung size, and negative pressures represent pressures that tend to increase lung volume because of outward recoil tendency of chest wall at approximately 60% of vital capacity or less. RV, Residual volume; TLC, total lung capacity. (From Drain C: Physiology of the respiratory system related to anesthesia. CRNA 7:163–180, 1996.)
Combined Mechanical Properties of the Lungs and Chest Wall
The combined P-V characteristics of the lungs and the chest wall have many implications for the perianesthesia nurse. The combined P-V curve is the algebraic sum of the individual P-V curves of the lungs and chest wall. When no muscle forces are applied to the respiratory system, the FRC is determined by a balance of elastic forces between the lungs and the chest wall (Fig. 12.13). Any pathophysiologic or pharmacologic process that affects the elasticity of either the lungs or the chest wall affects the FRC.
Alterations in the Balance of Pulmonary Forces in the Perianesthesia Patient
During the induction of anesthesia, the shape of the P-V curve of the chest wall is altered. This agent-independent phenomenon is probably the result of loss of chest wall elasticity. Thus, the P-V curve of the chest wall of a patient with normal lung function is shifted to the right, the balance of forces occurs sooner, and the FRC decreases (Fig. 12.14). This shift to the right affects the P-V curve of the lung; it also shifts to the right, and secondary changes occur in the lung. More specifically, the changes consist of an increase in lung recoil (↑PstL) and a decrease in CL (↓CL). Ultimately, the lung becomes stiffer, and the FRC decreases and may drop into the CC range. Therefore during tidal ventilation, some airways are closed to ventilation, and ventilation-perfusion mismatching occurs (↓alveolar ventilation/perfusion [↓VA/QC]), which ultimately leads to hypoxemia. Research indicates that this phenomenon, coupled with sighless breathing patterns in the PACU, can cause patients to have hypoxemia in the recovery phase of the anesthetic (see the section on postoperative lung volumes).10 This is a key concept to be used when recovering patients from anesthesia and surgery. Even if the patient has normal or altered preoperative lung function, the FRC will be reduced upon emergence from anesthesia as his or her P-V curve will be shifted to the right (Fig. 12.14) due to the previously discussed alteration in the lung mechanics. More specifically, the factors that make up hysteresis are altered such that the elastic properties of the lung tissue along with the recruitment of lung units, surface tension of the alveolar unit, and the lung capacities all become compromised to some level, leading to the reduction in the FRC. Chapter 28 will provide a comprehensive discussion of the nursing interventions associated with the reduced FRC. It must be remembered that the previously discussed lung mechanics become altered in the immediate postoperative period, and the SMI maneuver will serve to improve the lung mechanics and lead to an improved FRC. Lung mechanics play a vital role in the physiology of ventilation and are the key to the nursing care regimen used in the postanesthesia phase of the surgical patient (see Chapter 28).
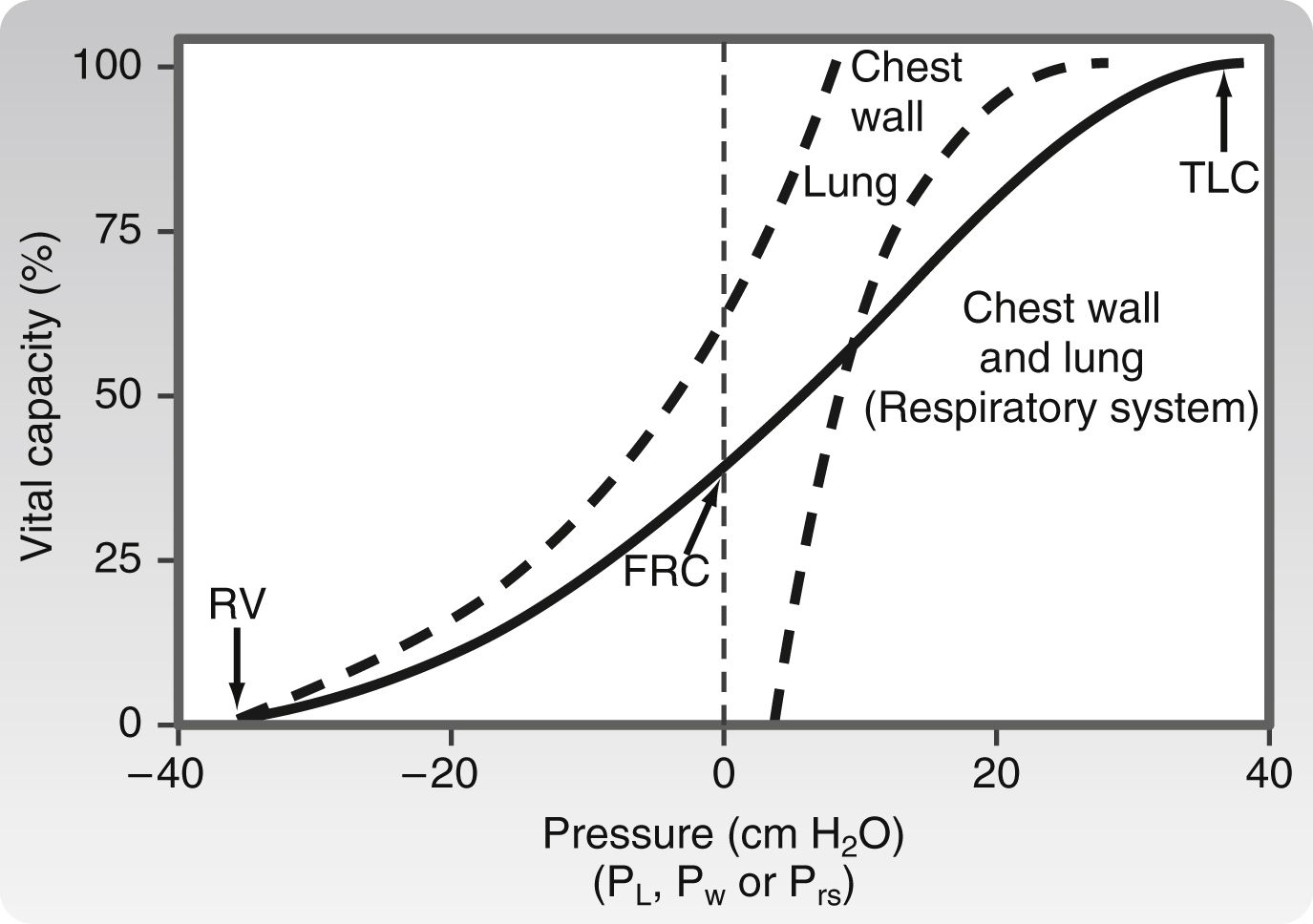
FIG. 12.13 Combined P-V curves of lungs and chest wall. Individual P-V curves of lungs and chest wall are represented with dashed lines. They are transposed from static deflation P-V curves of lungs (see Fig. 12.8) and chest wall (see Fig. 12.12). The combined P-V curve is the algebraic sum of deflation curves of the lungs and chest wall. In a combined P-V curve, FRC can be seen to be determined by balance of elastic forces of the lungs and chest wall when no respiratory muscles are applied. FRC, Functional residual capacity; P-V, pressure-volume; RV, residual volume; TLC, total lung capacity. (From Koeppen BM, Stanton BA: Berne and Levy’s physiology, ed 6 [updated edition], St. Louis, MO, 2010, Mosby.)
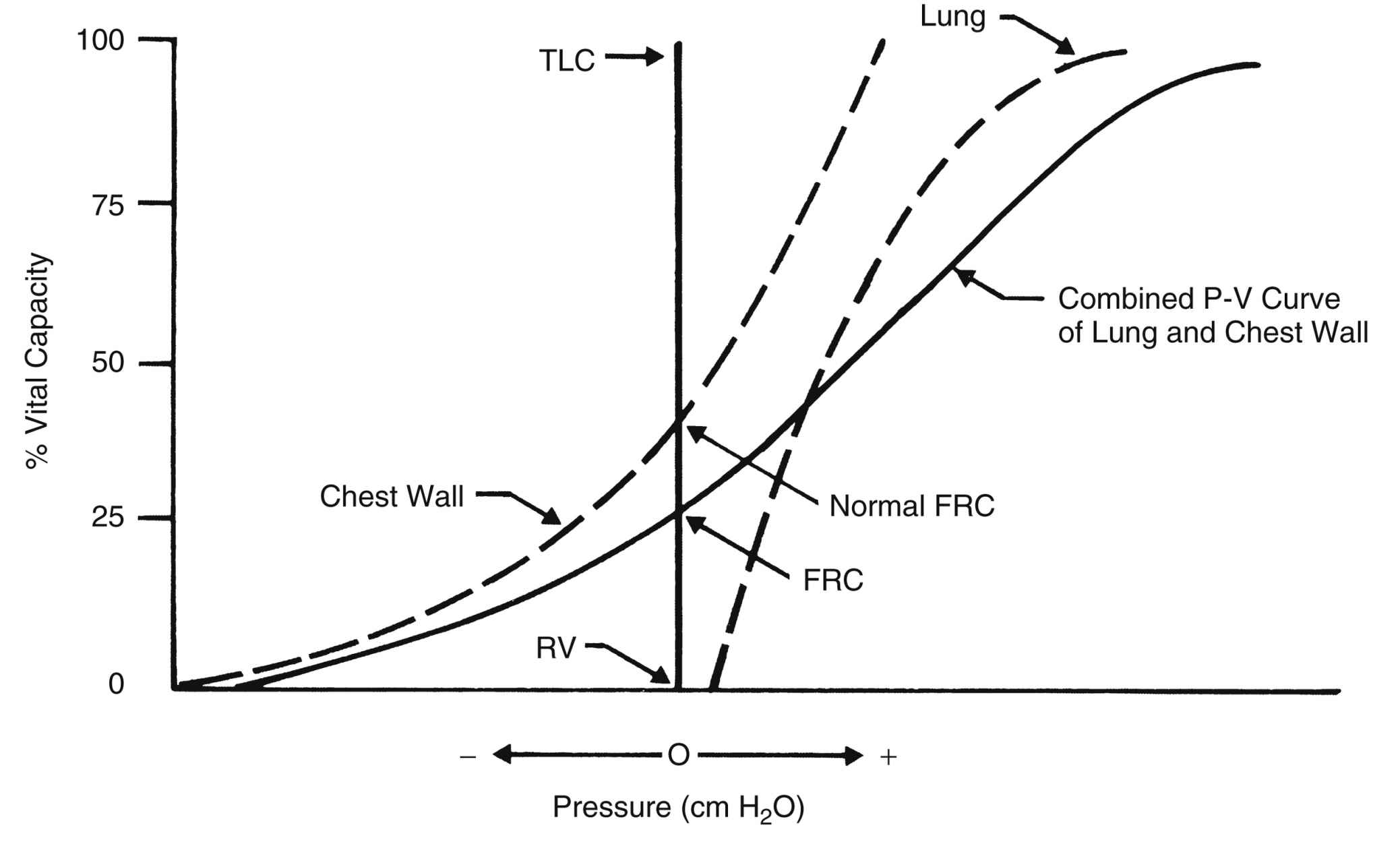
FIG. 12.14 P-V curve representing the lung mechanics of a patient in the immediate postoperative period who has undergone upper abdominal or thoracic surgical procedure. This patient has a loss of chest wall elastic recoil that causes lungs to become less compliant. Consequently, the combined P-V curve shifts to the right, leading to a decline in the FRC because balance of forces occurs at lower lung volumes. FRC, Functional residual capacity; P-V, pressure-volume; RV, residual volume; TLC, total lung capacity. (From Drain C: Pathophysiology of the respiratory system related to anesthesia. CRNA 7:181–192, 1996.)
Pulmonary Circulation
The basic functions of the pulmonary circulation are exchanging gas, providing a reservoir for the left ventricle, furnishing nutrition, and protecting the lungs.
Gas Exchange
The major aspects of gas exchange are discussed in the section on blood gas transport. Because of the implications for perianesthesia nursing care, the concepts of transit time and pulmonary vascular resistance are presented here.
Of the 5 L of blood that flows through the lungs every minute, only 70 to 200 mL are active in gas exchange at any one time. The time a red blood cell (RBC) takes to cross the pulmonary capillary bed is 0.75 seconds, but the RBC takes only 0.25 seconds to become saturated with oxygen—that is, until all the oxygen-bonding sites on the hemoglobin molecule are occupied. Because the transit time is 0.75 seconds and the saturation time is only 0.25 seconds, the body has a tremendous backup of 0.5 seconds for hemoglobin saturation with oxygen.5 If the RBCs move across the pulmonary capillary bed at an accelerated pace (decreased transit time), the amount of time available for oxygen to saturate the RBCs is decreased. During stress or exercise, however, the complete saturation of the hemoglobin can still be accomplished because the transit time of an RBC rarely decreases at less than 0.25 seconds.6
However, this process is not true for patients with interstitial fibrosis who have a thickened respiratory exchange membrane. These patients may have a normal PaO2 at rest, but exercise or exertion of surgery increases the cardiac output and decreases the RBC transit time; therefore, the hemoglobin does not become completely saturated during its passage through the pulmonary capillary bed. This phenomenon occurs because more time is needed for oxygen to pass through the diseased membrane. For these patients, the lower limit for complete saturation may be 0.5 seconds, not 0.25 seconds. As a result, patients with disorders of the respiratory exchange membrane can have a lower oxygen saturation (SaO2) on the pulse oximeter with any exertion that could decrease RBC transit time. Clinically, this phenomenon is sometimes called desaturation on exercise. Patients in the PACU suspected of having this problem should be given low-flow oxygen and be closely monitored for desaturation via a pulse oximeter. Because of the possibility of desaturation, the low-flow oxygen administration should not be discontinued until the patient’s condition stabilizes, which could indicate continued administration after the patient is discharged from the PACU. Measures should be started to reduce the extrinsic factors, such as stress, elevated body temperature, and anxiety, which increase the cardiac output.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree