FIG. 13.1 Anatomy of renal and urinary systems. A, Urinary system. B, Cross section of a kidney.
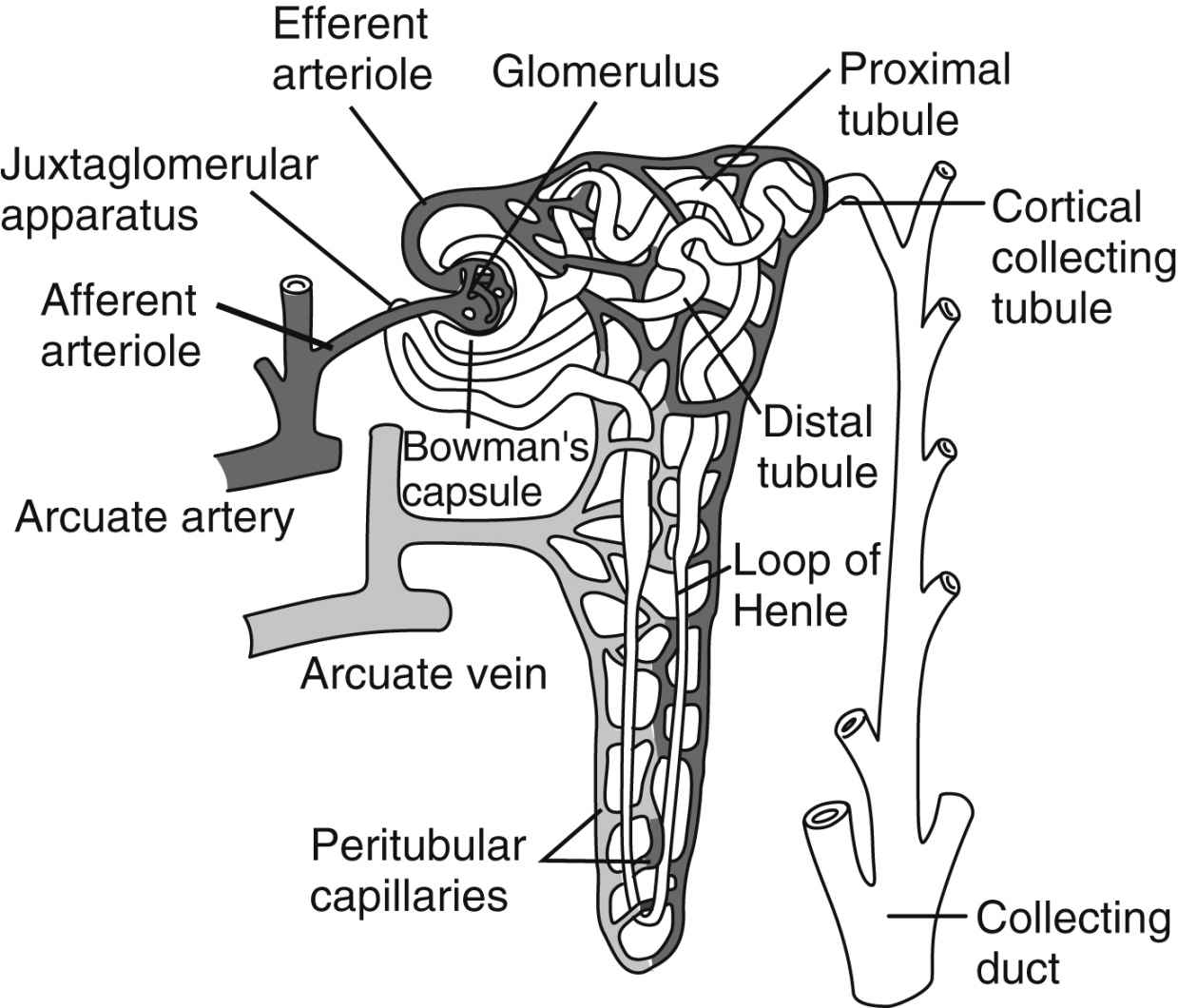
FIG. 13.2 Functional nephron. (From Hall J: Guyton and Hall textbook of medical physiology, ed 13, Philadelphia, PA, 2016, Elsevier.)
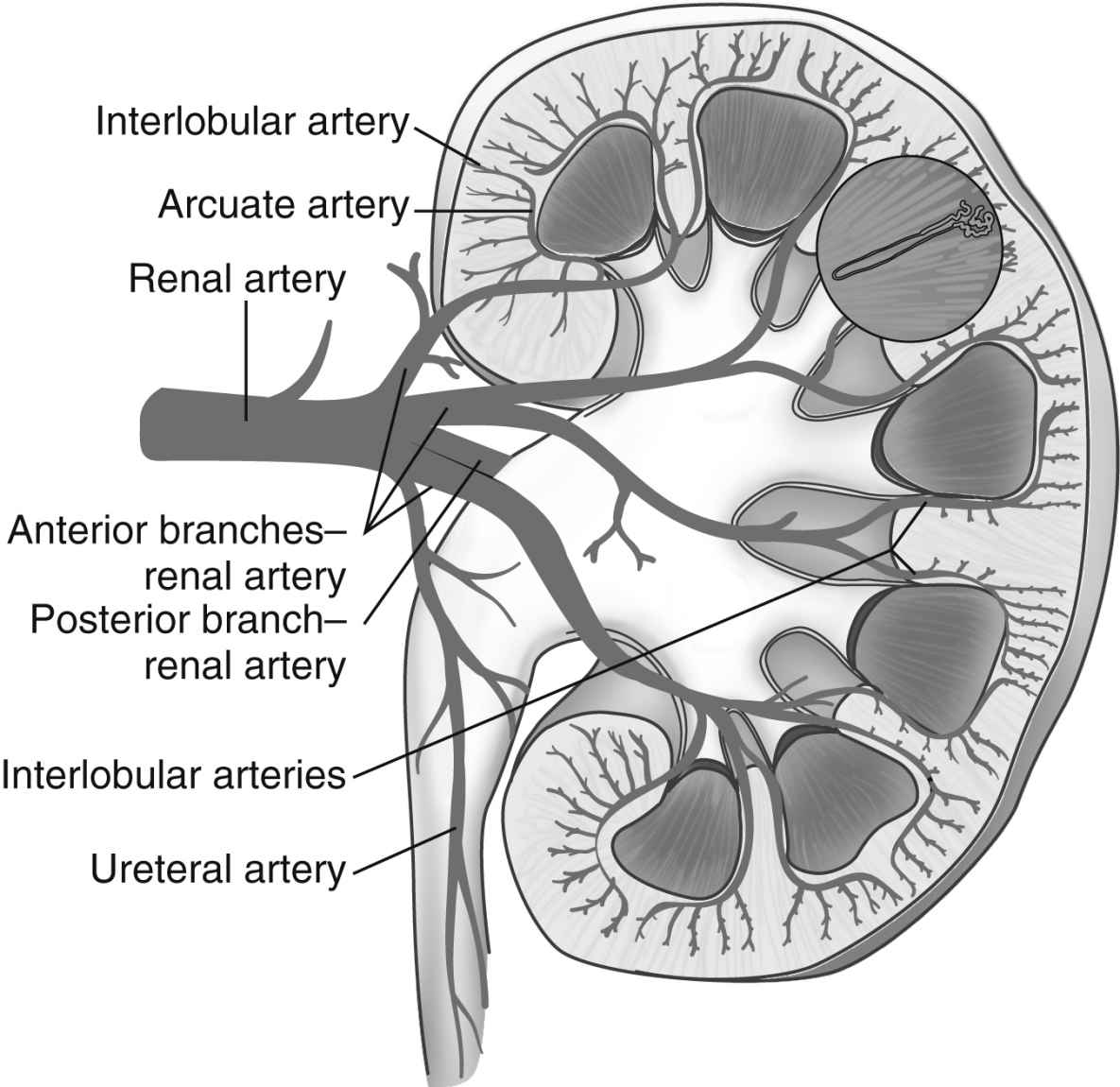
FIG. 13.3 Arterial supply to kidney. Soon after entering the hilum of the kidney, the renal artery divides into several anterior and posterior branches. Branches divide into interlobar arteries, which give off arcuate arteries that course between cortex and medulla.
Table 13.1
Particles Filtered by the Glomerulus, Reabsorbed by the Tubules, and Excreted in the Urine
The renal pelvis is a wide, funnel-shaped structure composed of the calyces draining the kidney. The pelvis drains into the ureter, which leads to the bladder.
Kidney Physiology
Urine is formed by processes of filtration, reabsorption, and secretion. Filtration occurs as the blood passes through the glomerulus. The force of filtration is a pressure gradient that pushes fluid through the glomerular membrane. Approximately 180 L of water along with other substances is filtered out of plasma by the glomeruli every 24 hours (Table 13.1). Blood cells and heavy particles including proteins are retained in the blood because they are too large to pass through the glomerular epithelium. The presence of red blood cells or protein in the urine usually indicates a pathologic process in the kidney.
Reabsorption occurs in the proximal and distal tubules. Approximately 99% of the water filtered by the glomeruli is reabsorbed. Many substances in the water are reabsorbed with active or passive transport. Active transport requires energy for movement of the substance across the membrane. Passive transport can be regarded as simple diffusion that does not require energy.
Important constituents of body fluids—substances such as glucose, amino acids, sodium, potassium, calcium, and magnesium—are almost entirely reabsorbed. Certain substances are reabsorbed in limited quantities, such as urea and phosphate, and consequently appear in the urine. In a healthy individual, creatinine is the only filtered substance not reabsorbed and entirely secreted, allowing creatinine to serve as an indicator of glomerular filtration ability. The last process in the formation of urine is secretion. Various substances, including hydrogen and potassium ions, are secreted directly into the tubular fluid through the epithelial cells that line the renal tubules. Secretion plays an important role in promoting the body’s acid-base balance.
Regulation of Kidney Function
The formation of urine and the reabsorption of substances needed for body function are aided by three physiologic mechanisms: the countercurrent mechanism, autoregulation, and hormonal control.
Countercurrent Mechanism
The kidneys use the countercurrent mechanism to concentrate urine. The vasa recta are special capillaries that, with the loop of Henle, form the countercurrent mechanism. Fluids flow in opposite directions between the ascending and descending loops and sections of the vasa recta. The osmolality or weight of particles in solution of the interstitial fluid increases as it moves deeper into the medulla. The increase in osmolality results in active transport of particles or solutes into the interstitial fluid. The countercurrent mechanism is useful when the body needs to excrete a large amount of waste products yet reabsorb the normal amount of solutes and when the water in the body needs to be conserved, while waste products are eliminated.
Autoregulation
Autoregulation helps keep the glomerular filtration at a near normal rate despite fluctuations in arterial pressure. The kidney is able to autoregulate when the mean arterial pressure is more than 75 mm Hg.2 As arterial pressure increases, the sympathetic innervation to the afferent arterioles causes constriction, thus keeping the glomerular filtration rate constant. When the arterial pressure is low, dilatation of the afferent arterioles serves to maintain glomerular filtration. However, sympathetic stimulation can disrupt the autoregulatory process, reducing blood flow despite the mean arterial pressure.
Hormonal Control
Secretion of antidiuretic hormone (ADH) by the posterior pituitary gland is affected by plasma osmolality. When the blood becomes hypertonic, ADH is secreted and the kidneys retain water. If the blood is hypotonic, less ADH is formed, causing the kidneys to reabsorb less water and increasing urine formation. ADH acts on the distal tubules and collecting tubules by altering permeability to water.
The juxtaglomerular complex is a group of cells, located just before the glomerulus and in close proximity to the distal tubule, which contain granules of inactive renin. Renin is released in response to reduced arterial blood pressure entering the afferent arteriole of the kidney or a low concentration of sodium in the distal tubule. The released renin acts as an enzyme to convert angiotensinogen to angiotensin I. Angiotensin I is converted to angiotensin II by the angiotensin-converting enzyme, which leads to angiotensin II. Angiotensin II stimulates the adrenal cortex to release aldosterone. Aldosterone signals the kidney tubules to increase the reabsorption of sodium and retention of water. Because the renin-angiotensin system causes this reabsorption of water and sodium, it plays a role in the control of arterial blood pressure and is important in the conservation of sodium and control of fluid volume in hypotensive states (Fig. 13.4).
Regulation of Body Homeostasis
The kidneys play a significant role in regulation of body fluids. The kidneys adjust blood volume and influence extracellular fluid volume, extracellular fluids, electrolytes, and ions. Homeostasis is maintained when the kidneys remove waste products and toxic substances.
The kidneys regulate blood volume through ADH, aldosterone, and the renin-angiotensin mechanism. When the circulating blood volume is excessive, the cardiac output and arterial pressure increases, resulting in greater pressure in the renal artery and the kidney afferent arteriole. Water and sodium are excreted. If the patient is hypovolemic, the kidneys reabsorb fluid to return the blood volume to normal limits.
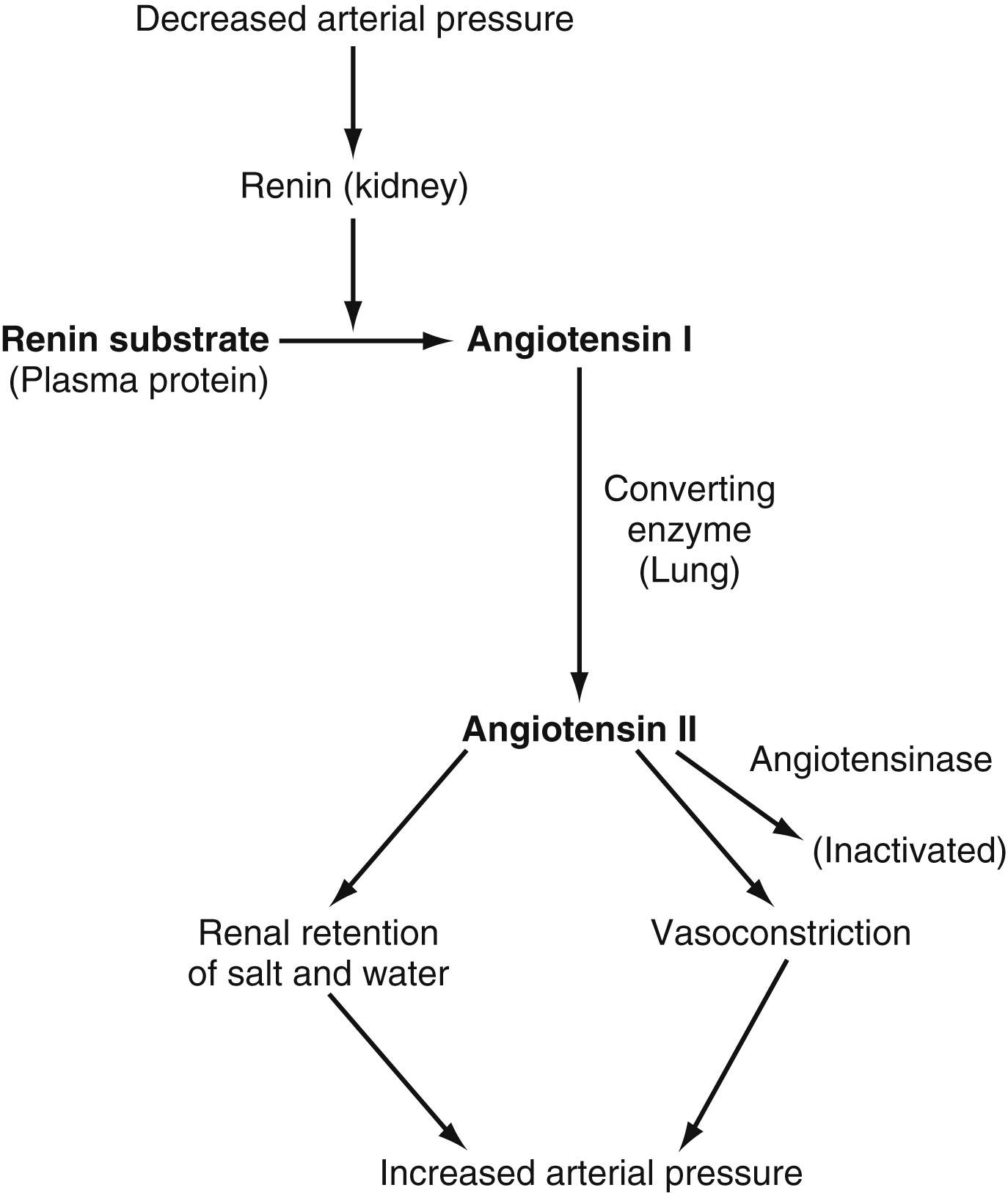
FIG. 13.4 Renin-angiotensin-vasoconstrictor mechanism for arterial pressure control. (From Hall J: Guyton and Hall textbook of medical physiology, ed 13, Philadelphia, PA, 2016, Elsevier.)
The kidneys indirectly control the extracellular fluid volume, which results in a control of blood volume. The relative ratio of the extracellular fluid volume to blood volume depends on the physical properties of the circulation and of the interstitial spaces including compliance and dynamics. The kidney maintains the osmolality of the extracellular fluid mainly by regulating the extracellular sodium concentration. Extracellular sodium controls 90% to 95% of the effective osmotic pressure of extracellular fluid.3 The extracellular concentration of other electrolytes, including potassium, calcium, magnesium, and phosphate ions, is also under renal control.
Components of Urine
The end product of filtration, absorption, and excretion is urine, which is composed of 95% water and 5% solids. The solids, approximately 60 g/L of urine, are listed in Table 13.2. Urea is derived from the breakdown of amino acids. Uric acid is an end product of purine metabolism, formed from purines ingested as food and from those formed in the body. Creatinine is an end product of creatine of which 95% is found in muscle tissue. Creatinine is produced during the production of muscle energy.
Creatinine is considered a nonthreshold substance because it is excreted by the kidney in its entirety. High-threshold substances are almost entirely reabsorbed in the kidney. They are an important portion of the blood and are excreted only if they are in an excess concentration. High-threshold substances include glucose, potassium, calcium, and magnesium. Low-threshold substances such as urea, uric acid, and phosphates are only minimally reabsorbed by the kidney.
In consideration of the substances found in urine, knowledge of the characteristics of normal urine is useful. Normal urine should be clear and transparent with an amber color, a reflection of urobilin, a byproduct of bilirubin breakdown. Urine is usually acidic because of the excretion of sodium acid phosphate with a pH of approximately 6. The specific gravity is between 1.003 and 1.025. The volume of urine excreted every 24 hours by an adult is approximately 1500 mL.
Acid-Base Balance
The kidneys play a major role in acid-base balance. Although they are the most powerful acid-base regulators, they require several hours to 1 day to return the hydrogen ion concentration to a normal range. In contrast, the respiratory system can react to acid-base imbalances within 1 to 3 minutes.
The pH is an expression of the hydrogen ion concentration in the body fluids. Bicarbonate and carbon dioxide are also factors. The bicarbonate concentration is mainly under renal control, whereas the carbon dioxide is under respiratory control. Approximately twentyfold more bicarbonate than carbon dioxide is in the plasma, resulting in a 20:1 ratio. Thus, any change in the 20:1 ratio affects the pH. Any change that affects kidney function affects the bicarbonate portion of the ratio and becomes a metabolic problem. Conversely, any change in the function of the lungs, which affects the carbon dioxide portion of the ratio, is a respiratory problem.
If, for example, a large amount of a bicarbonate solution is rapidly infused into a patient and ventilation does not change (PCO2 stays constant), the result is a higher value for the bicarbonate and no change in the PCO2. The net result is a higher pH, which indicates alkalosis, in this case metabolic alkalosis. Conversely, if an acid is infused, the ratio becomes smaller and the pH falls, indicating acidosis, which is termed metabolic acidosis.
The kidneys regulate pH by increasing or decreasing the bicarbonate ion concentration in the blood and eliminating hydrogen ions. This regulation is done with a complex series of reactions, which begins with hydrogen ions being secreted into the tubular filtrate. Carbon dioxide, an end product of tubular cell metabolism, combines with water to form carbonic acid (H2CO3). The carbonic acid dissociates to form hydrogen and bicarbonate (HCO3). The hydrogen ion is taken via active transport to the renal tubule and usually exchanges in the tubule with sodium. Via active transport, the sodium moves to the extracellular fluid where it combines with the bicarbonate that was reabsorbed into the extracellular fluid to form sodium bicarbonate (NaHCO3). In the tubules, the hydrogen ion that was actively transported to the tubule combines with the filtrate bicarbonate to form carbonic acid. The carbonic acid dissociates to form carbon dioxide and water. The carbon dioxide is reabsorbed into the extracellular fluid and is eventually excreted by the lungs; the water is excreted as part of the urine.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree