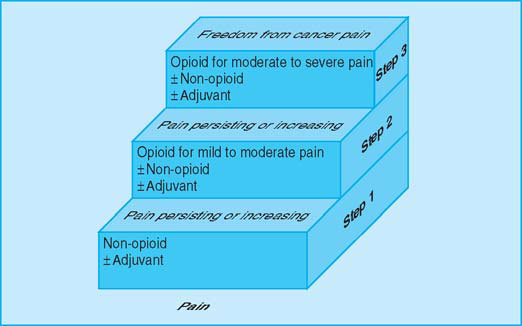
The WHO analgesic ladder
The analgesic ladder remains the mainstay of our approach to analgesia, though this was never designed for use in isolation. Surgery, radiotherapy, and appropriate tumoricidal treatments will have an important role in some patients, as will non-drug treatments. A combined approach can lead to optimum analgesia with minimum side effects.
Analgesic drugs do, however, remain key in managing cancer pain. The choice of drug should be based on the severity of the pain, not the stage of disease. Drugs should be administered in standard doses at regular intervals in a stepwise fashion. If a non-opioid or, in turn, an opioid for moderate pain is not sufficient, an opioid for severe pain should be used.
When a non-opioid drug is used with an opioid for moderate pain, many patients find combination formulations more convenient to use. Care must be taken with the dose of each drug in the formulation; some combinations of codeine or dihydrocodeine with aspirin or paracetamol (including co-codamol and co-dydramol) contain subtherapeutic doses of the opioid. The decision to use an opioid for severe pain should be based on severity of pain and not on prognosis.
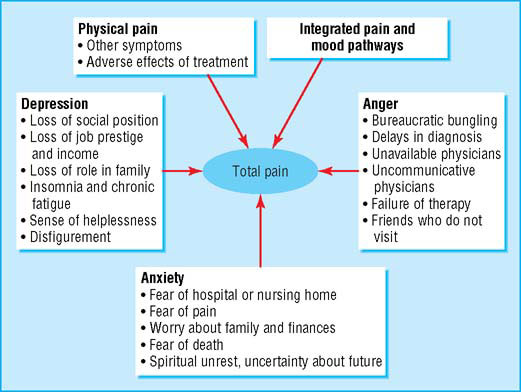
Factors affecting patient’s perceptions of pain (adapted from Twycross RG, Lack SA, Therapeutics in terminal disease, London: Pitman, 1984)
- Aspirin 600 mg four times a day
- Paracetamol 1 g four times a day
- Codeine 60 mg (plus non-opioid drug) four times a day
- Morphine 5–10 mg (starting dose) every four hours
- TENS (transcutaneous electrical nerve stimulation)
- Physiotherapy
- Acupuncture
- Relaxation therapy
WHO analgesic ladder (adapted from WHO’s Cancer pain relief and palliative care technical report series 804)
Adjuvant analgesics
Adjuvant analgesic drugs may be usefully added at any stage. An adjuvant analgesic is a drug whose primary indication is for something other than pain but that has an analgesic effect in some painful conditions. Examples are corticosteroids, non-steroidal anti-inflammatory drugs, tricyclic antidepressants, anticonvulsants, and some antiarrhythmic drugs.
Tricyclic antidepressants and anticonvulsants
Tricyclic antidepressants are effective in relieving neuropathic pain. There are no significant differences in efficacy between the different tricyclic antidepressants, though unfortunately, side effects often limit their use. While the evidence for venlafaxine is less strong, its use can be justified, particularly in patients with both neuropathic pain and low mood. There is a lack of high level evidence of the efficacy of selective serotonin reuptake inhibitors (SSRIs) for treating neuropathic pain.
The anticonvulsants carbamazepine, phenytoin, sodium valproate, clonazepam, gabapentin, and pregabalin are effective in treating neuropathic pain. Benefit is independent of the characteristics of the pain. Gabapentin and pregabalin are licensed for treatment of neuropathic pain.
There is no measurable difference in the analgesic benefit of the two drug classes (tricyclic antidepressants or anticonvulsants) in neuropathic pain or in the number of patients needed to treat before a minor or major adverse effect occurs. Gabapentin and pregabalin, however, can have fewer side effects in many patients, though systematic examination of this is awaited in patients with cancer pain.
Patients with neuropathic pain should have a trial of a tricyclic antidepressant or venlafaxine or an anticonvulsant. The choice of drug should be based on relative contraindications, possible drug interactions, and risk of side effects for each patient. Antidepressants and anticonvulsants may occasionally be prescribed simultaneously, though it is good clinical practice to introduce only one drug at a time.
Opioid analgesics for severe pain
Morphine is the most commonly used opioid in this group. When possible, it should be given by mouth, the dose tailored to each patient, and doses repeated at regular intervals so that the pain is prevented from returning. There is no arbitrary upper limit, but negative attitudes to using morphine still exist.
Dose titration—A normal release formulation of morphine (either elixir or tablet), with a rapid onset and short duration of action, is preferred for dose titration. The simplest method is to prescribe a regular four hourly dose but allow extra doses of the same size for “breakthrough pain” as often as necessary. After 24 or 48 hours, the daily requirements may be reassessed and the regular dose adjusted as necessary. This process is continued until pain relief is satisfactory. By this method, the many factors that contribute to the variability in dose are taken into account. These include the severity of the pain, the type of pain, the affective component of pain, and variation in pharmacokinetic parameters. The regular four hourly dose may range from 5–10 mg to ≥250 mg (or the equivalent in controlled release tablets). The dose is titrated against effect, though few patients need high doses—with most requiring <200 mg a day.
Maintenance dose—Patients with advancing disease and increasing pain may require continual adjustment of dose. For many patients, however, there is a period of stability during which the dose required remains unchanged or needs only small adjustments, and this may last for weeks or months or sometimes longer. Once pain is relieved, maintenance will be
| Common adjuvant analgesics for cancer pain Drugs Indications | |
| Drugs Indications | Indications |
| Non-steroidal anti-inflammatory drugs | Bone pain Soft tissue infiltration Hepatomegaly |
| Corticosteroids | Raised intracranial pressure Soft tissue infiltration Nerve compression Hepatomegaly |
| Antidepressants Anticonvulsants Antiarrhythmics | Nerve compression or infiltration Paraneoplastic neuropathies |
| Bisphosphonates | Bone pain |
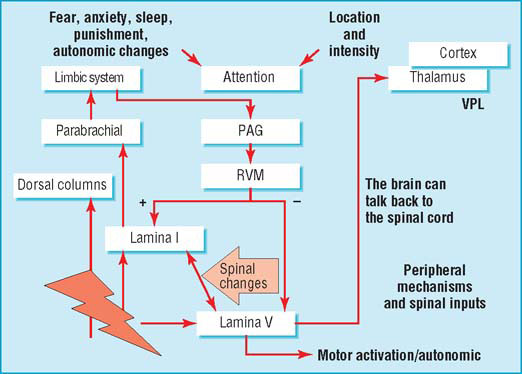
Integration of pain and emotion at higher centres. With permission from Professor A. Dickenson
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








