The Preoperative Evaluation
Richard D. Urman
Jonathan Kaper
Fred E. Shapiro
A pleasant and comfortable outcome for the patient will begin with planning in advance of the surgery. Such planning includes reviewing the patient’s medical history, scheduling the preoperative interview and physical examination, assessing for possible drug interactions with anesthetic, deciding on the most appropriate type of anesthesia, and then developing a complete care plan.
It is widely recognized that a thorough preoperative evaluation is a critical aspect of patient care. The anesthesiologist, however, is often faced with several issues that are unique to the office. More often than not, the anesthesiologist will meet and evaluate the patient on the day of the scheduled procedure. Therefore, although the patient would have been seen by the surgeon who would perform the initial patient evaluation, a focused preanesthetic evaluation would not have occurred. Unfortunately, the office usually does not have the traditional preoperative testing center now common in most hospitals. As the anesthesiologist evaluates the patient before providing anesthesia services, it is important to ask the following two questions:
Is the proposed procedure appropriate to be performed in the office? |
Is the patient a good candidate for the procedure to be performed in the office? |
There are procedures that may be inappropriate for an office-based setting. Many states and professional organizations have established rules and guidelines defining the complexity of surgical procedures and their appropriateness for an office-based setting. Some procedures may require nothing more than local anesthesia or conscious sedation, whereas others may require general anesthesia. When the anesthesiologist is evaluating the patient, it is important to consider how the proposed surgical procedure will impact the length of recovery and the complexity of postoperative care by the recovery room staff. Procedures that may entail large blood loss or large fluid shifts may not be appropriate for the office, as are procedures involving intracranial, intra-abdominal or intrathoracic cavities. The anesthesiologist must ascertain that the proposed procedure is within the scope of practice of the office facility and all health care providers involved (1).
PREOPERATIVE PATIENT EVALUATION
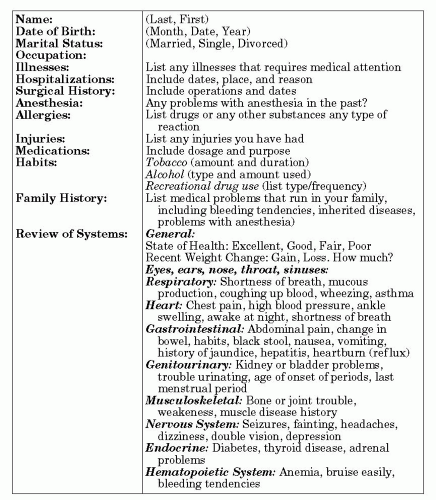
In addition to evaluating the appropriateness of the surgical procedure, the anesthesiologist must perform a thorough evaluation of the patient. In the office, this often takes place on the day of surgery, although ideally such an evaluation should take place days ahead to allow for necessary testing and medical record evaluation. Many offices begin by giving out a patient information packet, which includes an anesthesia information sheet. This handout provides answers to most frequently asked questions and addresses most common patient concerns (see Figure 6.1).
PREOPERATIVE INTERVIEW
To establish a good rapport with the patient and achieve a comfortable operating room experience, the nurse and/or anesthesiologist will interview
the patient by either a telephone call or at an office visit. This is a way to get introduced to the patient and in an unhurried interview to discuss the anticipated plan of care. This way, any questions regarding the patient’s medical history can be addressed, and any concerns of the patient can be discussed. These interviews are designed to ensure the goals of a safe and pleasant surgical and anesthetic experience are met, and to assure patients that their special concerns will be addressed. It is important for the anesthesia provider to alleviate the psychological stress of surgery by answering all of the patient’s questions and being available if further patient concerns arise before surgery.
the patient by either a telephone call or at an office visit. This is a way to get introduced to the patient and in an unhurried interview to discuss the anticipated plan of care. This way, any questions regarding the patient’s medical history can be addressed, and any concerns of the patient can be discussed. These interviews are designed to ensure the goals of a safe and pleasant surgical and anesthetic experience are met, and to assure patients that their special concerns will be addressed. It is important for the anesthesia provider to alleviate the psychological stress of surgery by answering all of the patient’s questions and being available if further patient concerns arise before surgery.
STANDARDS FOR ANESTHESIA CARE
In conjunction with various state and society regulations, many offices establish their own preoperative patient selection and evaluation guidelines.
Patient selection and evaluation criteria must also meet the standards set forth by the American Society of Anesthesiologists (ASA). The evaluation of patients for anesthesia in the office-based setting is further complicated by the fact that the resources taken for granted in the hospital-based operating room may not be immediately available. Careful classification of these patients must be performed to insure that they are indeed appropriate candidates for office-based anesthesia. The ASA has established Basic Standards For Preanesthesia Care (2), which were first approved by the ASA House of Delegates in 1987, and last amended in 2005. Specifically, these guidelines state that the anesthesiologist must review medical records, perform an appropriate physical examination, document relevant medical history, request additional testing and premedications, and obtain an informed consent. These recommendations describe the responsibilities of the anesthesiologist (see Box 6.1).
Patient selection and evaluation criteria must also meet the standards set forth by the American Society of Anesthesiologists (ASA). The evaluation of patients for anesthesia in the office-based setting is further complicated by the fact that the resources taken for granted in the hospital-based operating room may not be immediately available. Careful classification of these patients must be performed to insure that they are indeed appropriate candidates for office-based anesthesia. The ASA has established Basic Standards For Preanesthesia Care (2), which were first approved by the ASA House of Delegates in 1987, and last amended in 2005. Specifically, these guidelines state that the anesthesiologist must review medical records, perform an appropriate physical examination, document relevant medical history, request additional testing and premedications, and obtain an informed consent. These recommendations describe the responsibilities of the anesthesiologist (see Box 6.1).
Box 6.1
The anesthesiologist, before the delivery of anesthesia care, is responsible for the following:
Reviewing the available medical record
Interviewing and performing a focused examination of the patient to:
discuss the medical history, including previous anesthetic experiences and medical therapy
assess those aspects of the patient’s physical condition that might affect decisions regarding perioperative risk and management
Ordering and reviewing pertinent available tests and consultations as necessary for the delivery of anesthesia
Ordering appropriate preoperative medications
Ensuring that consent has been obtained for the anesthesia care
Documenting in the chart that the above has been performed
These standards apply to all patients who receive anesthesia or monitored anesthesia care, and the anesthesiologist should be responsible for “determining the medical status of the patient” and “developing a plan of anesthesia care.” Under unusual circumstances (e.g., extreme emergencies), these standards may be modified. When this is the case, the circumstances shall be documented in the patient’s record. The ASA physical status classification is also used to standardize the way patients are categorized (ASA I-VI) based on pre-existing medical condition (see Box 6.2). This classification system has been used as a common denominator for all communication, guidelines, discussion, and research purposes. In evaluating patients for surgery, the anesthesiologist and the office staff should pay a particularly close attention to the ASA Class III and IV patients who may require optimization of their medical conditions before surgery or may not be appropriate candidates for office surgery.
Box 6.2
ASA Physical Status Classification Guidelines
P1 | Normal healthy patient |
P2 | Patient with mild systemic disease |
P3 | Patient with severe systemic disease |
P4 | Patient with severe systemic disease that is a constant threat to life |
P5 | Moribund patient who is not expected to survive without the operation |
P6 | Declared brain-dead patient whose organs are being removed for donor purposes |
If the patient has had anesthesia in the past, it is important to note previous problems with anesthesia as well as good experiences in order to better tailor the anesthetic plan for each individual patient. In addition, a family history of problems with anesthesia must also be obtained.
The history and physical examination are the best measures of screening for disease and should be completed well in advance of the surgery. A patient-completed questionnaire will assist the surgeon and anesthesiologist in determining the need for further workup. Special attention should be paid to predictors of perioperative cardiac morbidity such as history of previous myocardial infarction, congestive heart failure, angina, hypertension, diabetes, cardiac arrhythmias, peripheral vascular disease, valvular heart disease, cigarette smoking, and obesity. The anesthesiologist should follow the current American College of Cardiology/American Heart Association guidelines for perioperative cardiovascular testing for noncardiac surgery (3).
In all patients, pertinent laboratory values and test results (hematology and chemistry laboratories, electrocardiogram, chest x-ray, cardiac/pulmonary reports) must be evaluated and reviewed by the anesthesiologist before the procedure. In addition, it may be necessary to obtain further tests and consultations that will be necessary to conduct the anesthesia. Before undergoing anesthesia, the patient may need medical clearance or may need comorbid conditions optimized before surgery. The history and physical examination should be current and re-evaluated by the surgeon on the day of surgery to ascertain that no significant changes in medical condition have occurred.
Despite these interventions, some patients may still not be good candidates for an elective cosmetic procedure that is to be performed in an office-based setting. It is important to assess these situations in advance to avoid canceling a procedure based on a lack of preoperative preparation. Because these pre-existing conditions have the potential for perioperative problems, patients with unstable conditions should be referred to a hospital where their specific medical conditions can be managed more acutely. As with any health care matter, it is important for the patient to be involved in the planning and the delivery of their care.
While performing a preoperative evaluation, the anesthesiologist should take the following factors into consideration when deciding whether the patient may be an appropriate candidate for surgery (4):
Abnormalities of major organ systems
Stability and optimization of any medical illness
Difficult airway
Previous adverse experience with anesthesia and surgery
Current medications and drug allergies
Time and nature of the last oral intake
History of alcohol or substance use or abuse
Presence of an adult who assumes responsibility specifically for caring for and accompanying the patient from the office
Preoperative preparation should also include adherence to the NPO guidelines outlined in the ASA Practice Guidelines for Preoperative Fasting (see Table 6.1) (5




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree