The Placebo Response: Implications for Neural Blockade
Damien G. Finniss
Fabrizio Benedetti
The placebo response has been a topic of interest for over 200 years and, in recent times, has been gaining more interest in the scientific and clinical communities. Our understanding of the mechanisms of the placebo effect has improved with more rigorous studies using novel research design and technology. This enhanced understanding has led in turn to further questions as to the impact of the placebo effect on clinical practice and clinical trial design (1,2). Much of our knowledge about the mechanisms of the placebo effect has come from the field of pain and analgesia. This chapter surveys the placebo effect per se, as distinct from the well-described physiologic effects of needle insertion that must also be taken into account in evaluating the effects of regional anesthesia. The latter are reviewed in Chapter 34 by Butler and Siddall.
Historical Overview
The first documented use of the word placebo in medical literature dates back to 1785, and not long after that, the first placebo-controlled trial was apparently conducted (3,4). This trial was conducted between 1799 and 1801 by Haygarth, who experimented with the use of metallic rods (“Perkins tractors”) on five patients. It was believed that implantation of these metallic rods would alleviate the symptoms of many diseases, due to the electromagnetic properties of the metal. Haygarth first implanted imitation rods (made from wood) in his five patients, finding that four gained relief. He then repeated the procedure the following day on the same patients, however, this time, he used the metallic rods. Again, four patients gained relief. Possibly the most interesting feature of this trial was one of Haygarth’s conclusions. He remarked “an important lesson in physic is here to be learnt, the wonderful and powerful influence of the passions of the mind upon the state and disorder of the body” (3).
Since the trial conducted by Haygarth, a steady if slow increase has occurred in the number of trials using placebo controls, which ultimately resulted in the development of the double-blinded trial (5). The randomized, double-blind, placebo-controlled trial, in which both the clinician and the patient are unaware of whether active treatment or placebo is being given, is now the gold standard in clinical trial design (4,6). Despite placebo use in clinical trials for some years, and the publication over 50 years ago of Beecher’s landmark paper analyzing the responses of patients in some of the early placebo-controlled trials (7), the study of the mechanisms of the placebo effect has only recently started to gain more attention in the scientific community.
Mechanisms of the Placebo Response
The mechanisms of the placebo response can be discussed under separate psychological and neurobiologic categories, although it is the integration of these two approaches that provides an opportunity to explore the complexity of the mind–brain–body interaction.
Psychological Mechanisms
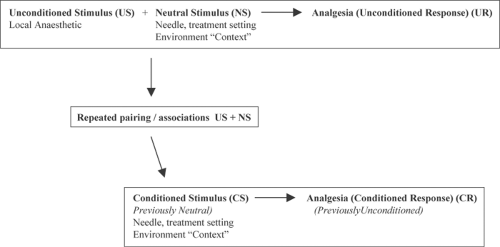
The psychological mechanisms of placebo responses studied in greatest detail are those of expectancies and conditioning. Other potential mechanisms that require further investigation include changes in anxiety and desire for pain relief (8,9). The conditioning mechanism is based upon the theory of classical conditioning, whereby a previously neutral stimulus (such as the treatment characteristics or the environment in which treatment is delivered) is paired or “conditioned” with an unconditioned stimulus (the active drug) that is able to elicit a response (conditioned response) (10,11). In the case of injections, the pairing of the context of treatment with an active drug and analgesia may result in a conditioned analgesic response to an injection of a placebo at a later stage (Fig. 36-1). The conditioning mechanism has gained support through a variety of trials both in animals (12,13) and humans (14,15). A recent study demonstrated that placebo analgesic responses were able to be conditioned using both opiate and nonopiate drugs (16). This study also looked at expectancy mechanisms and found that the placebo analgesic response was greatest when both conditioning and expectancy were involved. There is, however, a degree of difficulty in distinguishing the conditioning mechanism from the expectancy mechanism in placebo analgesia, as the conditioning process may influence the expectations of the patient toward the treatment, and thus the placebo analgesic response may in fact be mediated by expectancies (17,18,19).
One study was able to demonstrate the conditioning mechanism in a clinical population (20). In this study, patients were given standard postoperative analgesia, and ventilatory function was monitored. On the third postoperative day, a placebo was given that resulted in similar changes in ventilatory
function (respiratory depression) as had been experienced with the opioids. In this study, the placebo was able to cause a “side effect” similar to that of the active drug. More recent work has also shown that the conditioning mechanism, particularly when involving unconscious processes, such as hormone secretion (18) and immune responses (21,22), may contribute to placebo effects. In the case of placebo analgesia, it would seem that the expectancy mechanism plays a significant role and may be integrated with the conditioning process.
function (respiratory depression) as had been experienced with the opioids. In this study, the placebo was able to cause a “side effect” similar to that of the active drug. More recent work has also shown that the conditioning mechanism, particularly when involving unconscious processes, such as hormone secretion (18) and immune responses (21,22), may contribute to placebo effects. In the case of placebo analgesia, it would seem that the expectancy mechanism plays a significant role and may be integrated with the conditioning process.
The expectations of the patient regarding the treatment being administered, also termed response expectancies, are those held by an individual about his automatic emotional and physiological responses to a particular stimulus (23,24). A variety of studies have investigated the expectancy mechanism using simple verbal cues (suggestibility) (16,25,26,27), as well as more complicated conditioning protocols aimed at increasing expectations prior to placebo administration (17,28,29). These studies have shown that expectations are powerful contributors to placebo responses, particularly the placebo analgesic response.
Neurobiologic Mechanisms
The neurobiologic mechanisms of the placebo response were highlighted for the first time in 1978, by Levine, Gordon, and Fields, who showed that placebo analgesia was reversed by the administration of naloxone, an endogenous opioid antagonist, suggesting a role of endogenous opioids in the placebo analgesic response (30). The majority of research into the neurobiologic mechanisms of the placebo response has looked at the role of endogenous opioids, although in some studies naloxone has had no effect on placebo analgesia (16,31,32). The occurrence of both positive and negative results for the effects of naloxone suggests that placebo analgesia is mediated by both opioid and nonopioid mechanisms.
One interesting example of the variable role of endogenous opioids is the study by Amanzio and Benedetti in 1999 (16). In this study, both conditioning and expectancy mechanisms were manipulated. Two different types of drugs were used for the conditioning protocol, an opiate analgesic (morphine) and the nonsteroidal anti-inflammatory drug (NSAID) ketorolac. The same drugs were used to explore expectancy manipulations. Placebo analgesic responses were seen following conditioning with both these drugs, and the responses in the expectancy groups were reversed by naloxone, demonstrating that the expectancy mechanism is mediated by endogenous opioids. Interestingly, in the conditioning groups, only the placebo analgesic response that was conditioned with morphine was able to be reversed by naloxone, whereas the placebo response conditioned with the NSAID was not. This variability demonstrates that different mechanisms (both opioid and nonopioid) are involved in the placebo response and that the drug used to condition the response plays a role in the mechanism of the response.
The role of endogenous opioids has been supported by numerous experiments that have indicated that naloxone can fully (33,34) or partially (35) reverse placebo analgesia, including placebo analgesia elicited through expectation and opioid conditioning (16,25). Interestingly, naloxone is able to reverse spatially or target-specific placebo analgesia in specific parts of the body, suggesting a somatotopic organization of endogenous opioid systems at the level of higher centers in the brain (25). This is a particularly important finding as it demonstrates that the placebo analgesic response acts through release of endogenous opioids at a variety of sites in the nervous system that are involved in the experience of pain. The reversal of placebo-induced respiratory depression (20), decreased heart rate, and decreased β-adrenergic response (36) indicates that the opioid mechanisms of the placebo response also act on other regions and neural circuits, such as the respiratory and cardiovascular centers.
Further interesting examples of the involvement of other neurochemical systems are seen in other recent studies. In one study, preconditioning with a serotonin agonist (sumatriptan) prior to placebo administration resulted in placebo-induced increases in plasma growth hormone and decreases in cortisol (18). Studies of the placebo response in Parkinson disease have added to our understanding of the neurobiology of the placebo response. In Parkinson disease, placebo administration can lead to an increase in dopamine in the ventral (37) and dorsal striatum (38) of sufferers, and this increase in dopamine correlates with improvement in motor function (38). Electrophysiologic evidence has also shown improvements in motor function, along with placebo-induced changes in subthalamic nucleus neuronal activity (39). The relevance of
placebo-induced dopamine release for placebo analgesia is that dopamine has been shown to play an important role in reward mechanisms, and placebo administration activates brain areas associated with both reward system and opioid system circuitry (40,41,42,43). Parkinson disease has thus emerged as an interesting model to study the placebo response, particularly in light of the increasingly evident anatomic and biochemical relationship between reward and opioid circuitry.
placebo-induced dopamine release for placebo analgesia is that dopamine has been shown to play an important role in reward mechanisms, and placebo administration activates brain areas associated with both reward system and opioid system circuitry (40,41,42,43). Parkinson disease has thus emerged as an interesting model to study the placebo response, particularly in light of the increasingly evident anatomic and biochemical relationship between reward and opioid circuitry.
Advances in imaging technology have allowed the investigation of regional brain activation during the experience of pain and during the placebo analgesic response. Positron emission tomography (PET) and functional magnetic resonance imaging (fMRI) studies have shown consistent activation of certain cortical and subcortical areas during the experience of pain compared to control groups who are not experiencing pain (44,45). These areas encompass the neural pathways believed to be responsible for the sensory, affective, and evaluative dimensions of the pain experience. This pattern of activation, termed the pain matrix, corresponds to the neuronal substrate of multiple dimensions of pain according to the neuromatrix model described by Katz and Melzack in Chapter 35.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree