FIGURE 8.1 Coronal section of the sella turcica demonstrating the anatomic relationship between the pituitary gland and cranial nerves, carotid arteries, and the cavernous and sphenoid sinuses. (By permission of Mayo Foundation for Medical Education and Research. All rights reserved.)
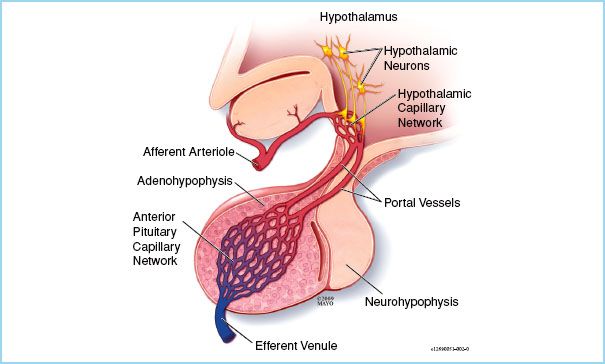
FIGURE 8.2 Physiology of the adenohypophysis. Afferent arterioles enter the hypothalamus where hypothalamic neurons secrete hormone into the circulation. Blood then leaves the hypothalamus via portal vessels and enters the adenohypophysis (i.e., anterior pituitary gland) where the hypothalamic hormones enter a second capillary network and act upon adenohypophyseal cells thus regulating the secretion of hormones. Hormones produced by the adenohypophysis enter the capillary network and enter the systemic circulation by the efferent venule. The advantage of a portal system allows for low volumes of hypothalamic hormones to be secreted since their concentration will be much higher in the portal vessels than in the systemic circulation also allowing rapid regulation of hormone secretion by the adenohypophysis. (By permission of Mayo Foundation for Medical Education and Research. All rights reserved.)
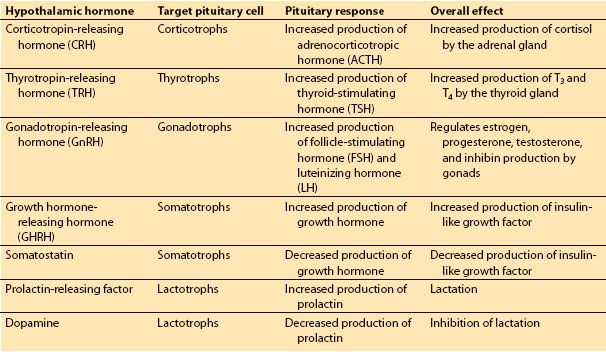
Table 8.1 Hypothalamic and adenohypophyseal hormones
C. Physiology of the neurohypophysis. A direct extension of the brain, the neurohypophysis contains the terminal axons of neurons located in the supraoptic and paraventricular nuclei (Fig. 8.3). Thus the pituitary stalk contains axons of the hypothalamo-hypophyseal tract. These neurons synthesize, store, and secrete into capillaries located within the neurohypophysis, both oxytocin and antidiuretic hormone (ADH) (i.e., vasopressin).
CLINICAL PEARL
Nonfunctional pituitary tumors often become symptomatic due to growth and compression of surrounding structures, thus are often larger and more locally invasive at resection than functional tumors.
II. Pituitary tumors. Tumors of the pituitary gland are the most common cause of pituitary dysfunction in adults. Eighty-five percent of all pituitary tumors are adenomas; however, other tumors such as craniopharyngiomas, meningiomas, primary carcinomas, metastatic tumors, astrocytomas, hemangiomas, and hamartomas can also occur [1]. Most adenomas consist of a single cell type and are generally classified into two categories based on whether or not the tumor cells secrete a specific hormone which results in clinical manifestations of hormone excess.
1
A. Functional tumors. These tumors will manifest as clinical signs and symptoms of excess production of one or more specific hormones. These specific clinical scenarios are addressed in section III of this chapter. As functional tumors often produce clinical signs and symptoms related to hormone overproduction prior to those related to compression of structures adjacent to the sella turcica, they are often smaller at the time of diagnosis. Hence, most functional tumors are microadenomas or <1 cm in diameter at diagnosis.
B. Nonfunctional tumors. Adenomas may also be derived from either nonfunctional cell lines or from hormone-producing cell lines in which hormonal overproduction does not lead to overt clinical manifestations. In the latter scenario, adenomas derived from gonadotropin-producing cell lines (e.g., follicle-stimulating hormone, luteinizing hormone) or prolactin-secreting cell lines may produce very nonspecific clinical signs and symptoms, or no symptoms related to excessive hormone production. Nonfunctional tumors are often identified either by signs and symptoms related to compression of structures within the confines of the sella turcica or may extend to impinge on surrounding structures. Increased pressure from the tumor within the sella may produce headache or hypopituitarism. Superior extension may result in compression of the optic chiasm which contains the axons of afferent neurons from the medial retina. As these neurons relay information from the lateral visual fields, early inferior compression from a tumor results in bitemporal superior quadrantanopia whereas later, more severe compression results in bitemporal hemianopsia or complete loss of lateral visual fields. (Fig. 8.4). Further rostral tumor grown may result in hypothalamic dysfunction or obstructive hydrocephalus. Lateral extension can lead to dysfunction of cranial nerves that traverse the cavernous sinus causing dysfunction of extraocular muscles and diplopia or sensory disturbances of the face. In addition, compression of the carotid artery may occur. As nonfunctional tumors need to grow in order to produce clinical manifestations, they are usually larger than functional tumors at the time of diagnosis; hence they are often referred to as macroadenomas (>1 cm diameter).
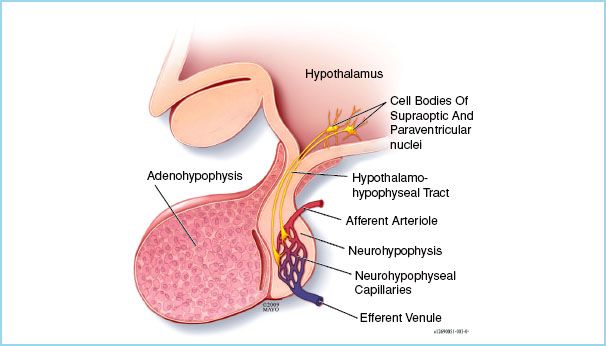
FIGURE 8.3 Physiology of the neurohypophysis. The axons of neurons located in the supraoptic and paraventricular nuclei of the hypothalamus extend via the hypothalamo-hypophyseal tract to the neurohypophysis. When stimulated, these neurons secrete either oxytocin or vasopressin into the capillary network of the neurohypophysis. (By permission of Mayo Foundation for Medical Education and Research. All rights reserved.)
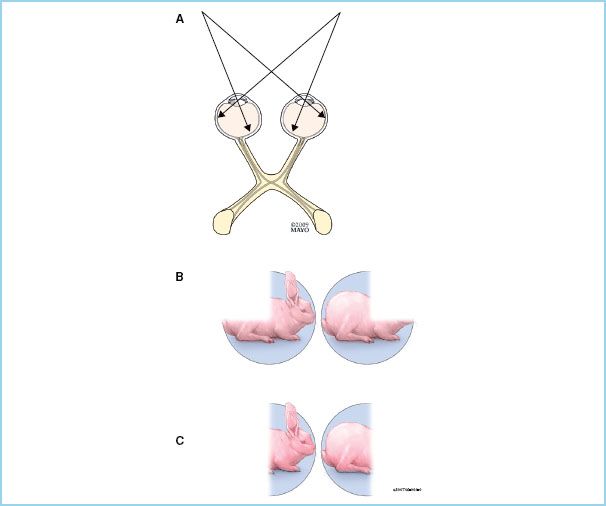
FIGURE 8.4 Visual fields. A: Light from the left and right lateral (or temporal) visual fields strikes the left and right medial regions of the retina, respectively. Afferent neurons originating from the medial regions of the retina cross in the optic chiasm. Injury to the optic chiasm results in dysfunction of these neurons thus loss of the lateral visual fields. Early in the course of enlargement of the contents of the sella turcica, axons located within the inferior portion of the optic chiasm are compressed. These axons carry information from the inferiomedial bilateral retinas and visual information from the superiolateral visual fields resulting in loss of the superiolateral quadrants of the visual field (i.e., bitemporal superior quadrantanopia (B)). As tumor growth continues, as all axons within the optic chiasm can become compressed, full loss of the lateral visual fields occurs (i.e., bitemporal hemianopsia (C)). (By permission of Mayo Foundation for Medical Education and Research. All rights reserved.)
C. Treatment. Treatment of pituitary tumors depends on multiple factors such as patient age, tumor type, size, invasiveness, hormonal aberrations, and comorbidities. Patients may undergo medical therapy for specific tumor pathologies, radiation therapy, or surgical resection. Medical therapy will be discussed later in this chapter in the context of specific tumor pathologies.

FIGURE 8.5 The transsphenoidal route is the most common approach for the resection of pituitary tumors in adults. Usually with the aid of an operating microscope, instruments are advanced through the nasal cavity. The sphenoid sinus is entered after which the roof of the sphenoid sinus is opened and the pituitary gland is approached through the floor of the sella turcica. (By permission of Mayo Foundation for Medical Education and Research. All rights reserved.)
D. Management of anesthesia. In the majority of cases, surgical resection of a pituitary tumor is accomplished via the transsphenoidal route (Fig. 8.5) whereas other approaches, such as translabial or craniotomy, are often reserved for patients requiring increased tumor exposure due to size or invasiveness, or in children in whom the size of the nares and nasal cavity may not permit the introduction of necessary surgical instruments. Transsphenoidal resection of a pituitary mass is performed via general anesthesia. The sphenoid sinus is entered endoscopically and the posterior/superior wall of the sphenoid sinus is traversed to enter the sella turcica. The tumor is then resected with the aid of microscope.
Airway management, specific drug choices, and the need for invasive monitoring and large-bore intravenous access are typically determined based on the size and degree of invasiveness of the tumor, stigmata of endocrinopathy, and the presence of comorbid conditions. Significant bleeding may occur during the resection of large invasive tumors. Pharyngeal packing should be considered to limit gastric accumulation of blood. As vasoconstrictors, such as cocaine or epinephrine, are usually administered within the nasal mucosa, significant hypertension may occur. Patient movement should be avoided given the close proximity of the carotid artery to the sella. In addition, the surgeon may request placement of a lumbar drainage catheter. This will allow indirect manipulation of the tumor via the withdrawal of cerebrospinal fluid (to elevate the tumor by reducing intracranial pressure) or instillation of either air or sterile saline to displace the tumor caudally. If air is injected, nitrous oxide, if used, should be either discontinued or reduced in concentration.
2
Hormonal aberrations can occur following pituitary tumor resection and include hypopituitarism, diabetes insipidus (DI), or syndrome of inappropriate antidiuretic hormone (SIADH). Generally, a serum cortisol concentration is obtained the day following surgery as changes in hormonal concentrations of the pituitary–adrenal axis are most sensitive to acute pituitary insufficiency as the serum half-lives of adrenocorticotropic hormone (ACTH) and cortisol are short (10 minutes and 70 to 120 minutes respectively). If serum cortisol is >10 μg/dL, the patient is unlikely to develop hypopituitarism [2,3]. Urine output should be monitored postoperatively to assess for DI, or less likely the SIADH. Patients developing DI may require treatment with desmopressin acetate (DDAVP). Persistent cerebrospinal fluid leak occurs in approximately 2% of cases and is evident by rhinorrhea with symptoms of low cerebrospinal fluid pressure (e.g., headache occurring in the sitting or standing position) [4]. The presence of β2-transferrin in the rhinorrhea fluid is diagnostic. Other complications include postoperative nausea and vomiting, bleeding, infection, and injury to nearby neurologic structures (e.g., cranial nerves, optic chiasm).
CLINICAL PEARL
Postoperative complications of pituitary tumor resection include nausea and vomiting, bleeding, hypopituitarism, infection, cerebrospinal fluid leak, and although rare, injury to local neurologic and vascular structures.
III. Cushing’s disease
A. Physiology of the hypothalamic–hypophyseal–adrenal axis. Cortisol is the primary glucocorticoid produced in humans. Production of cortisol by the adrenal gland is regulated by a negative feedback loop that also involves the hypothalamus and adenohypophysis (Fig. 8.6). Secretion of corticotropin-releasing hormone (CRH) by the hypothalamus stimulates the production of ACTH by the adenohypophysis. In turn, ACTH enters the systemic circulation and stimulates the secretion of cortisol by the adrenal cortex. Cortisol production then inhibits production of CRH and ACTH by the hypothalamus and adenohypophysis, respectively, thus reducing further stimulus for cortisol production. Of note, central nervous system-mediated changes in cortisol production (e.g., during times of stress, diurnal variation) are likely mediated by the hypothalamus as changes in CRH production.
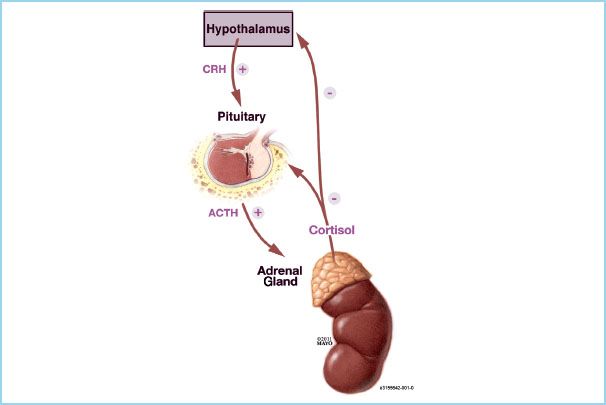
FIGURE 8.6 Cortisol production by the adrenal gland is regulated via a feedback loop involving both the hypothalamus and adenohypophysis. Corticotropin-releasing hormone (CRH) stimulates the production of adrenocorticotropic hormone (ACTH) by the adenohypophysis. ACTH stimulates production of cortisol by the adrenal glands which suppresses further production of both CRH and ACTH. (By permission of Mayo Foundation for Medical Education and Research. All rights reserved.)
B. Physiologic role of cortisol. Although named for their role in modulating glucose metabolism, glucocorticoids have wide physiologic effects.
1. Metabolism. Cortisol stimulates both gluconeogenesis and glycogen synthesis by the liver. Cortisol also decreases the sensitivity of tissues to the effect of insulin by decreasing the expression of glucose transporters on cell membranes. As such, cortisol increases serum glucose concentration and facilitates the storage of glycogen. Cortisol also increases energy substrate availability by stimulating protein degradation in muscle and increasing lipolysis in adipose tissue.
2. Vasculature. Cortisol is critical to maintaining the sensitivity of the vasculature to the vasoconstrictive effects of catecholamines, specifically epinephrine and norepinephrine.
3. Immune system. The anti-inflammatory and immune system suppressive effects of cortisol and other glucocorticoids are well known. These effects are likely mediated by diverse actions of glucocorticoids on many different pathways responsible for the inflammatory and immune responses. Glucocorticoids inhibit the release and antagonize the actions of interleukin-1, a cytokine that is pivotal in mediating the immune response via promoting leukocyte chemotaxis and lymphocyte proliferation. Degranulation of leukocytes, mast cells, and macrophages is inhibited by the glucocorticoids. Glucocorticoids also interfere with the metabolism of arachidonic acid thus reducing the synthesis of prostaglandins, thromboxanes, and leukotrienes.
4. Renal. Glucocorticoids facilitate free water excretion by the kidney.
C. Pathophysiology of Cushing’s disease. Cushing’s disease is a subtype of Cushing’s syndrome (i.e., hypercortisolism) and is reserved for hypercortisolism resulting from excessive production of ACTH by a pituitary adenoma. Signs and symptoms include the following:
1. Rapid weight gain, especially in the trunk and face (i.e., moon facies)
2. Growth of fat pads on the upper back (i.e., buffalo hump)
3. Hypertension
4. Hyperglycemia
5. Hypokalemic alkalosis
6. Impaired wound healing
7. Thinning of the skin and development of acne
8. Development of purple striae
9. Proximal muscle weakness
10. Osteoporosis
11. Psychological effects such as insomnia, depression, and psychosis
Cushing’s disease is diagnosed based on the presence of clinical signs and symptoms and via laboratory tests. These tests include increase in 24-hour urinary cortisol concentrations or failure of serum cortisol concentrations to decrease following the administration of dexamethasone—a potent inhibitor of the hypothalamic–pituitary–adrenal axis (i.e., the dexamethasone suppression test). The location of the adenoma is often confirmed with pituitary imaging. Treatment generally involves surgical removal of the adenoma. For patients who are not surgical candidates, radiation therapy or medical therapy with drugs which suppress cortisol biosynthesis and secretion (e.g., ketoconazole, aminoglutethimide, metyrapone, mitotane, cyproheptadine) may be initiated.
D. Management of anesthesia. Preoperative management of blood pressure, serum glucose concentration, electrolyte abnormalities, and the presence of fluid retention should be assessed, optimized, and managed. Obesity, moon facies, and buffalo hump may theoretically predispose to a challenge with mask ventilation and laryngoscopy; however, data suggest that Cushing’s disease itself does impair airway management [5]. Careful attention should be paid to positioning and placement of adhesive dressings as skin damage can easily occur. The specific choice of anesthetic agents is not influenced by hypercortisolemia. However, etomidate may transiently decrease secretion of cortisol by the adrenal gland; it is unknown if this effect has clinical relevance. The presence of pre-existing muscle weakness may increase sensitivity to nondepolarizing muscle relaxants.
3
IV. Acromegaly
A. Physiology and regulation of growth hormone. Growth hormone is a peptide hormone secreted by the somatotropic cells of the anterior pituitary gland. Secretion is regulated by the hypothalamus via the secretion of both growth hormone–releasing hormone (GHRH) and somatostatin, that respectively stimulate or inhibit secretion of growth hormone by the adenohypophysis. Once in the systemic circulation, the effects of growth hormone are mediated either directly via its action at growth hormone receptors or via hepatic production of insulin-like growth factor (ILGF, also known as somatomedin C). Together, the actions of growth hormone and ILGF include the following:
1. Stimulation of cell growth and proliferation within all major organ systems except the central nervous system
2. Stimulation of muscle protein synthesis and sarcomere hyperplasia
3. Chondrocyte proliferation
4. Increased bone ossification
5. Effects on metabolism
a. Increased hepatic gluconeogenesis
b. Lipolysis
c. Increased protein synthesis
6. Immune system stimulation
B. Pathophysiology of growth hormone excess. Although both manifestations of the same disorder, pituitary gigantism occurs when growth hormone excess occurs prior to ossification of the epiphyseal cartilage and acromegaly results when the onset of growth hormone excess occurs following epiphyseal ossification. Despite the difference in stature, pituitary gigantism and acromegaly share many features. Bone and soft tissue growth results in enlargement of the hands and feet, coarse facial features, and jaw hypertrophy leading to prognathism and malocclusion. Other airway manifestations include enlargement of the tongue, tonsils, epiglottis, and larynx. As such, patients often develop obstructive sleep apnea. Vocal cord dysfunction can occur due to stretching of the recurrent laryngeal nerves and impaired mobility of the cricoarytenoid joints. Cardiovascular system effects account for most deaths from untreated acromegaly. Hypertension is common. Cardiac hypertrophy is due to direct effects of growth hormone on cardiac muscle and secondary to increased afterload from hypertension and often leads to diastolic dysfunction [6,7]. The combination of increased cardiac mass (hence increased oxygen requirements) and diastolic dysfunction predisposes to coronary insufficiency. Patients can also exhibit dysrhythmias and electrocardiographic abnormalities [8]. Peripheral neuropathies are common and are due to demyelination and perineural edema [9]. Metabolic abnormalities include glucose intolerance or frank diabetes mellitus secondary to increased gluconeogenesis.
4
Diagnosis is often based on the presence of signs and symptoms in addition to laboratory tests. As growth hormone is secreted in a pulsatile fashion, single random serum growth hormone values are often not helpful in establishing the diagnosis. Serum concentrations of ILGF in fasting patients are more reliable as normal values are 0.3 to 1.4 U/mL whereas those found in patients with acromegaly are 2.6 to 21.7 U/mL [10]. The diagnosis of a tumor is then confirmed via radiologic imaging of the sella.
Treatment usually involves surgical resection of the adenoma. For patients who are not candidates for surgery, or in whom surgery has failed, radiation or medical therapy with either octreotide (a somatostatin analog) or dopamine agonists (e.g., bromocriptine, cabergoline, pergolide, lisuride) may be beneficial at preventing further progression.
C. Management of anesthesia. Hypertrophy of the mandible and enlargement of the tongue and other soft tissues in the mouth and airway, including glottic structures, can not only increase the difficulty of laryngoscopy, but may make mask fit and mask ventilation difficult [5]. The most conservative means to secure an airway in an acromegalic patient is via awake fiberoptic bronchoscope. If the decision is made to induce general anesthesia prior to laryngoscopy, the clinician should have appropriate back-up equipment readily available in the event that either mask ventilation or direct laryngoscopy is difficult or impossible. This may include oral or nasal airways, an assistant to help with two-person bag-mask ventilation, and various airway devices (e.g., laryngeal mask airway, video laryngoscope). As mandibular hypertrophy can increase the distance between the mouth and glottis, and glottic narrowing may be present, a full-length endotracheal tube with a smaller diameter should be available. Hypertrophy of the costal cartilage can lead to restrictive pulmonary mechanics. As hypertension, diastolic dysfunction, coronary insufficiency, and dysrhythmias may be present or occur, direct arterial blood pressure monitoring may be warranted. Despite beliefs to the contrary, hypertrophy of the transverse carpal ligament does not increase the risk of ischemic complications of the hand with radial artery cannulation [11].
CLINICAL PEARL
Clinical manifestations of acromegaly are likely to impact mask ventilation and laryngoscopy as standard preoperative airway assessment may not reliably predict ease of mask ventilation and laryngoscopy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







