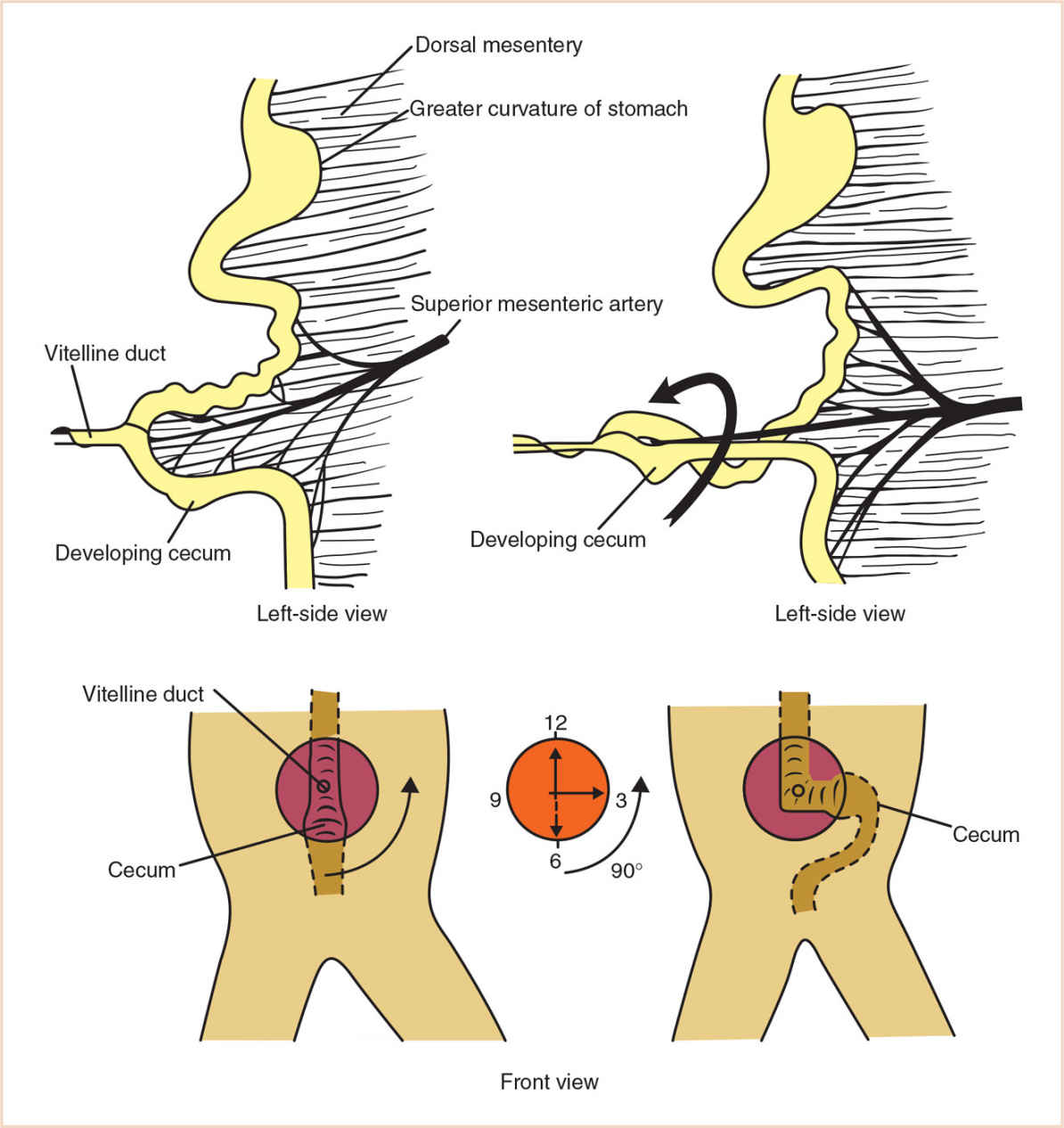
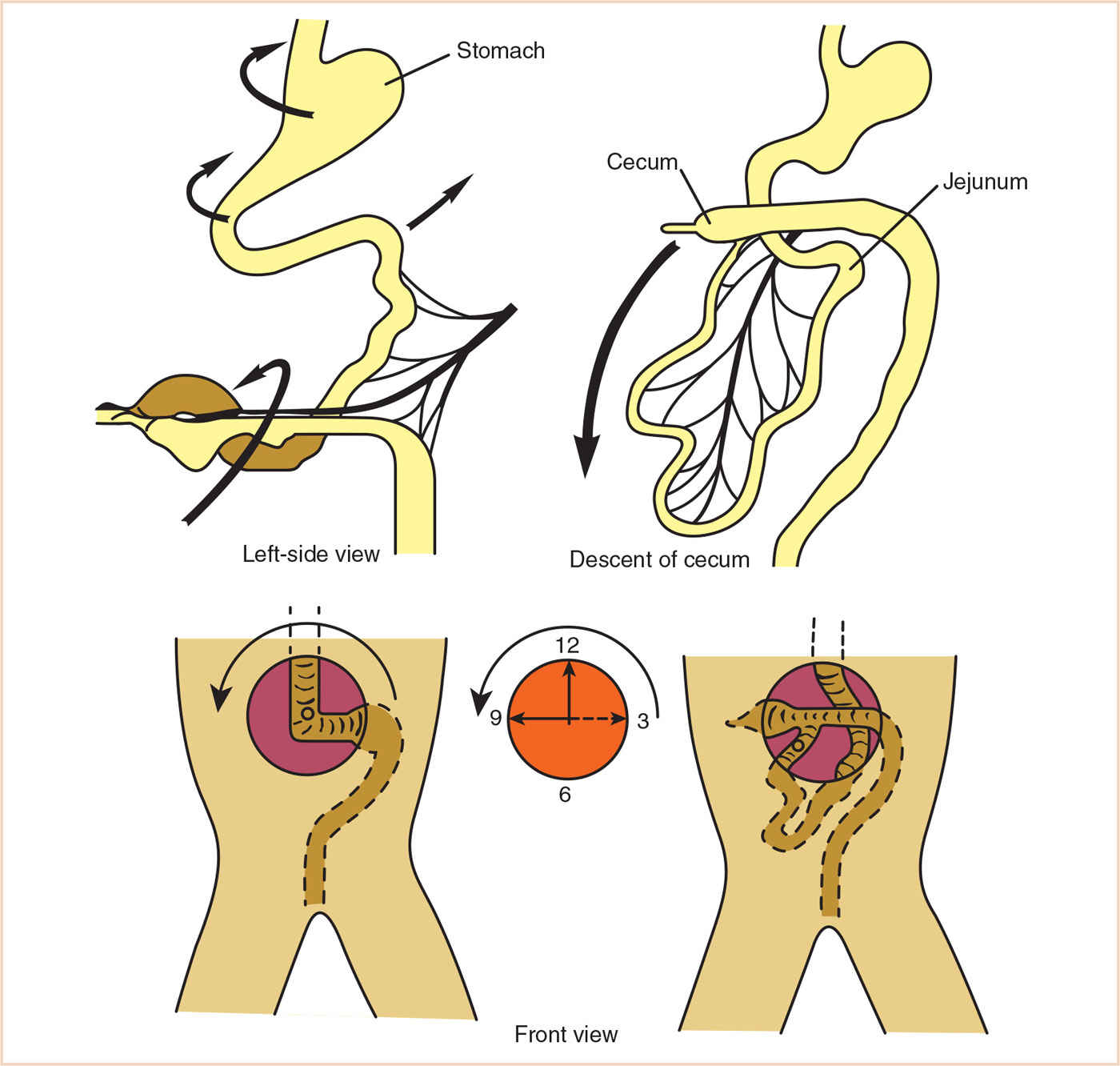
1. The midgut lengthens so rapidly that it herniates into the umbilical cord, rotating approximately 90 degrees about a counterclockwise axis and returns to the abdominal cavity after rotating another 180 degrees counterclockwise for a total of 270 degrees.
2. Abnormalities of midgut formation may therefore be the result of abnormalities of rotation, residuals of embryological structures, and atresias or stenoses of normal postnatal structures.
3. Common features include respiratory distress, sepsis, volume depletion, contraction alkalosis, metabolic acidosis, hypoglycemia, inanition, coagulopathy, and pain.
4. Readiness for surgery is established by fluid resuscitation and restoration of intravascular volume, availability of blood and blood products, adequacy of ventilation, protection of the airway, and adequate access (intravenous, and if needed, intra-arterial and central venous).
INTRODUCTION
Midgut abnormalities: second half of the duodenum, jejunum, ileum, cecum, appendix, ascending colon, and proximal two thirds of the transverse colon.
The small bowel caudal to the second half of the duodenum, as well as the large bowel up to the left colic flexure, is derived from the midgut, which lengthens so rapidly that it herniates into the umbilical cord. This midgut loop rotates approximately 90 degrees about a counterclockwise axis (ventral view of the fetus). In the third month of fetal life, the herniated bowel returns to the abdominal cavity after rotating another 180 degrees counterclockwise for a total of 270 degrees of rotation (Figs. 22.1 and 22.2). Abnormalities of midgut formation may therefore be the result of abnormalities of rotation, residuals of embryological structures, atresias or stenoses of normal postnatal structures, as well as other problems.
1. Complete obstruction in 1:5,000 live births
CLINICAL PEARL Intestinal obstruction results in vomiting, abdominal distention, decreased bowel sounds, and gas-filled loops of bowel.
2. Associated with few other anomalies
3. Prematurity in 50% of cases
4. Polyhydramnios in 25%
5. Cystic fibrosis in 20%
6. May take several forms, including stenosis, true atresias of only the small bowel, atresias involving the mesentery, and multiple atresias.
ENTERIC CYSTS/GASTROINTESTINAL DUPLICATIONS (3)
1. Enteric cysts and intestinal duplications are both considered gastrointestinal duplications.
2. 75% do not even communicate with the intestinal lumen and are typically cystic in form.
3. 25% will contain ectopic gastric tissue and therefore significant ulceration and bleeding can occur.
4. Partial intestinal obstruction is due to the cyst or tubular malformation causing extrinsic compression of the adjacent normal intestine.
CLINICAL PEARL This obstruction leads to electrolyte imbalance (initially contraction alkalosis; in severe cases will lead to metabolic acidosis), respiratory embarrassment, aspiration, intestinal perforation, bowel necrosis, and septicemia.
5. Technetium scanning may be helpful in the presence of ectopic gastric mucosa.
6. Surgical treatment is accomplished by partial or complete excision, partial excision with mucosal stripping, or a reentry procedure, providing internal drainage.
1. Present in approximately 2% of the population; only 50% are symptomatic.
2. The most common persistent remnant of the gut having passed through the omphalomesenteric duct during extrusion of the bowel.
3. Usually found 2 feet from the ileocecal valve, not more than 2 inches in length, and may contain two heterotopic tissue types (hence the rule of 2s, along with the 2% incidence). Most commonly pancreatic or gastric mucosal tissue.
MALROTATION/VOLVULUS
1. Problems with the normal return, positioning, and fixation of the gut may result in midgut volvulus, internal hernias, duodenal and colonic obstruction.
2. Twice as common in boys as in girls.
3. While it usually presents in the first several months of life, it may not present until adulthood. There may be other accompanying anomalies as well.
4. Classical X-ray findings are a duodeno-jejunal junction to the right of the spine.
INTUSSUSCEPTION
1. Typically occurs in infants less than 1 year old, following a viral gastroenteritis or upper respiratory infection (URI). When “leading” points occur, they can be a polyp, Meckel diverticulum, duplication cyst, or tumor (lymphoma, sarcoma).
2. Initially, venous compression of the invaginated bowel occurs along with its mesentery, and venous stasis and edema may eventually lead to arterial vascular compromise and bowel necrosis.
3. Patient may have currant jelly or bloody mucus stools.
4. Most commonly, it is the bowel just proximal to the ileocecal valve. A sausage-shaped mass may be palpated in the right upper quadrant.
5. Barium enema may be diagnostic as well as therapeutic in over 80% of cases.
6. Laparoscopic approaches for surgical reduction of the intussusception are now the standard approach, with laparotomy for failed laparoscopy (6).
MECONIUM ILEUS
1. Intraluminal obstruction, typically of the distal small bowel, by meconium.
2. Almost exclusively found in patients with cystic fibrosis (CF), but only 20% of patients with CF have meconium ileus.
3. Respiratory symptoms of CF are not present.
4. If medical management (enemas with acetylcysteine) fails, then surgery is done.
CROHN DISEASE: Submucosal edema, fibrous and lymphatic dilation and small slit-like ulcers produce a cobblestone appearance in the mucosa, thickening the intestinal wall (see IBD section).
PHYSIOLOGIC CONSIDERATIONS (7)
Respiratory distress
Sepsis
Volume depletion
Contraction alkalosis
Systemic acidosis
Hypoglycemia/inanition
Coagulopathy
Pain
SURGICAL REPAIR
1. Exploratory laparotomy/laparoscopy with possible derotation and closure (8–10)
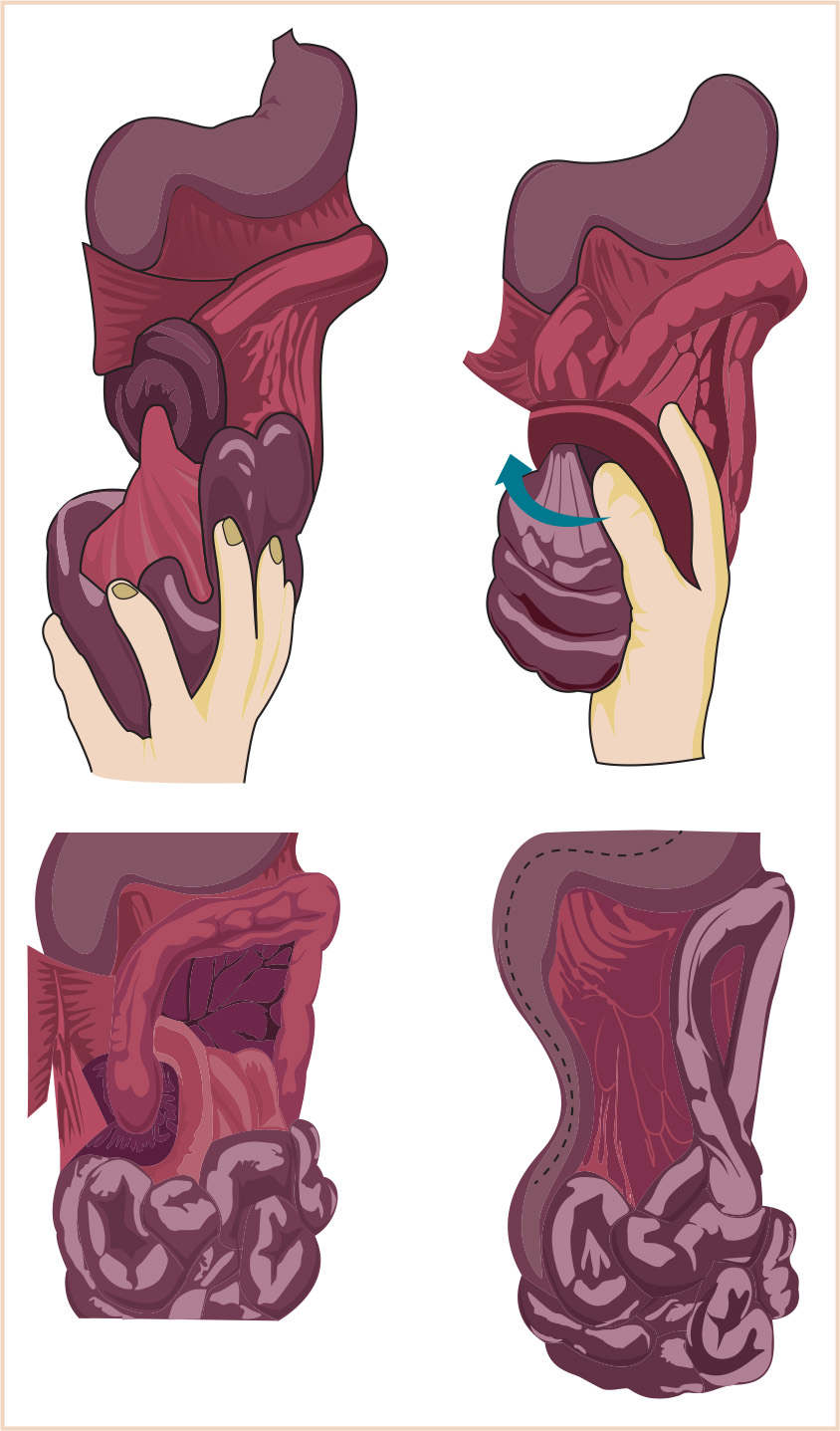
2. Derotation and Ladd’s procedure (Fig. 22.3)
a. Following exploratory laparotomy/laparoscopy, the small bowel must be derotated in a counterclockwise direction.
b. Peritoneal folds are then divided separating the duodenum from the ascending colon in order to widen the mesenteric pedicle.
c. Peritoneal folds (Ladd’s bands) passing from the ascending colon to the duodenum and into the right lateral gutter are incised along the medial aspect of the duodenum.
d. An appendectomy is typically performed because of the unusual position of the appendix in the left upper abdomen.
e. Second-look surgery in order to examine previously ischemic bowel is not unusual.
3. Small-bowel resection with primary anastomosis
4. Small-bowel resection with stoma creation
5. Insertion of central venous line or peripherally inserted central catheter (PICC) line for access and nutrition.
ANESTHESIA ISSUES
READINESS FOR SURGERY
Fluid resuscitation/restoration of intravascular volume
Availability of blood/blood products
Adequacy of ventilation
Airway protection
Access (intravenous, primarily; intra-arterial and central venous when needed)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree