The Lower Extremity: Somatic Blockade
F. Kayser Enneking
Denise J. Wedel
Terese T. Horlocker
Lower extremity peripheral nerve blocks (PNBs) have traditionally been less popular and less utilized compared to other forms of regional anesthesia. Epidural and subarachnoid anesthesia, which provide rapid, reliable, and safe anesthesia of the lower extremities, are more widely taught to anesthesiologists than lower extremity peripheral neural blockade techniques. Unlike the upper extremity, the entire lower extremity cannot be anesthetized with a single injection, and injections are generally deeper than those required for upper extremity block. Over the past decade, several developments have led to an increased interest in lower extremity PNBs, including transient neurologic symptoms associated with spinal anesthesia, increased risk of epidural hematoma associated with more aggressive antithromboembolic prophylaxis regimens, and evidence of improved rehabilitation outcome with lower extremity single-injection and continuous PNBs (1).
Like other forms of neural blockade, lower extremity techniques are not new. As early as 1887, Crile performed amputations by exposing the sciatic nerve in the gluteal fold and the femoral nerve in the inguinal fold, and injecting cocaine intraneurally. Braun mentions that blockade of the lateral cutaneous femoral nerve was described by Nystrom in 1909 (2). Laewen expanded on this by describing the additional blockade of the anterior crural nerve, and Keppler improved both techniques by advocating the elicitation of paresthesias. Subsequently, no fewer than six others advocated percutaneous approaches to the sciatic nerve alone. Many of these same authors described blockade of other nerves of the lower extremity as well (Chapter 1). Importantly, many of the techniques currently utilized are nearly identical to the original descriptions. This emphasizes remarks made by Labat that: “Anatomy is the foundation upon which the entire concept of regional anesthesia is built”; and that “The anesthetist should attempt to visualize the anatomic structures traversed by the needle and utilize the tactile senses to determine the impulses transmitted by the point of the needle as it approaches a deep landmark (e.g., bone)” (3). Labat localized neural structures using fascial “pops” and the elicitation of one or more paresthesias, as well as field infiltration. Advances in needles, catheters, and nerve stimulator technology have facilitated localization of neural structures and improved success rates. Even more recently, direct imaging using ultrasound, fluoroscopy, computer tomography (CT), and magnetic resonance imaging (MRI) has been utilized.
Anatomy
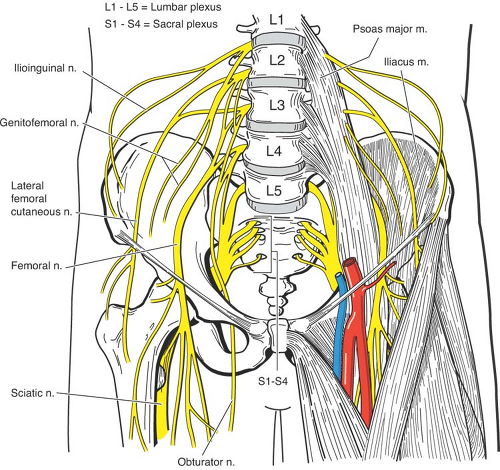
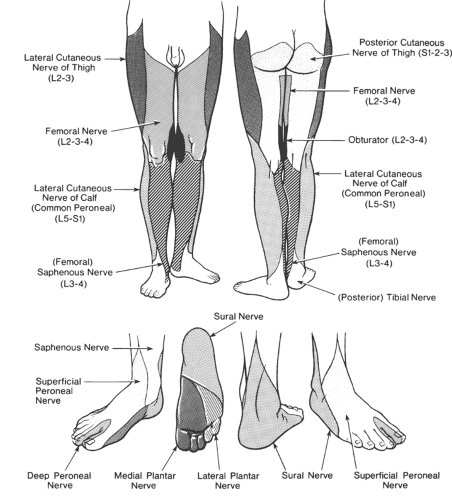
Anatomically, the lumbosacral plexus consists of two distinct entities: the lumbar plexus and the sacral plexus. Some communication exists between these plexus via the lumbosacral trunk, but for functional purposes these are distinct entities (4). The lumbosacral plexus arises from at least eight spinal nerve roots, each of which contains anterior and posterior divisions that innervate the embryologic ventral or dorsal portions of the limb. With the exception of a small cutaneous portion of the buttock (which is supplied by upper lumbar and sacral segmental nerves), the innervation of the lower extremity is entirely through branches of the lumbosacral plexus (Tables 14-1 and 14-2; Figs. 14-1 and 14-2). The nerves to the muscles of the anterior and medial thigh are from the lumbar plexus. The muscles of the buttocks, the posterior muscles in the thigh, and all the muscles below the knee are supplied by the sacral plexus.
Lumbar Plexus Anatomy
The lumbar plexus is formed within the psoas muscle from the anterior rami of T12–L4 (4,5,6,7) (Fig. 14-1). Although the lumbosacral plexus as a whole contributes to the nerve supply of the lower extremities, the upper part of the lumbar division supplies the iliohypogastric and ilioinguinal nerves, which are in series with the thoracic nerves and innervate the trunk above the level of the extremity (Chapter 16). Specifically, the iliohypogastric nerve provides cutaneous innervation to the skin of the buttock and the muscles of the abdominal wall. The ilioinguinal nerve supplies the skin of the perineum and adjoining portion of the inner thigh (see Chapter 16). A third nerve, the genitofemoral nerve, arises from the first and second lumbar nerves. It supplies filaments to the genital area and adjacent parts of the thigh. It also gives off a lumboinguinal branch, which supplies the skin over the area of the femoral artery and femoral triangle (Table 14-1). The branches of the lumbar plexus and the iliohypogastric, ilioinguinal, genitofemoral, lateral femoral cutaneous, femoral, and obturator nerves, emerge from the psoas laterally, medially, and anteriorly. Of these, the femoral nerve (sometimes called the anterior crural nerve), lateral femoral cutaneous nerve, and obturator nerve are most important for lower extremity surgery (Figs. 14-1 and 14-2).
Sacral Plexus Anatomy
The sacral plexus gives off two nerves important for lower extremity surgery, the posterior cutaneous nerve of the thigh and the sciatic nerve (Fig. 14-2). The posterior cutaneous nerve has sometimes been referred to as the “lesser sciatic” nerve. It derives from the first, second, and third sacral nerves, as does the larger sciatic nerve, which also receives branches of the anterior
rami of the fourth and fifth lumbar nerves. Inasmuch as the two nerves course through the pelvis together and out through the greater sciatic foramen, they are considered together when techniques for blocking the sciatic nerve above the gluteal fold are discussed.
rami of the fourth and fifth lumbar nerves. Inasmuch as the two nerves course through the pelvis together and out through the greater sciatic foramen, they are considered together when techniques for blocking the sciatic nerve above the gluteal fold are discussed.
Table 14-1 Lumbar plexus anatomy | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Table 14-2 Sacral plexus anatomy | |||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||
The sciatic nerve is really an association of two major nerve trunks. The first is the tibial, derived from the ventral branches of the anterior rami of the fourth and fifth lumbar and first, second, and third sacral nerves. The second is the common peroneal, derived from the dorsal branches of the anterior rami of the same five nerves. These two major nerve trunks pass as the sciatic to the proximal angle of the popliteal fossa, where they separate, with the tibial portion passing medially and the common peroneal (lateral popliteal) laterally. This division can occur more cephalad or caudad to the popliteal fossa. The smaller branches of these nerves, which provide distal innervation of the lower extremity, are discussed in detail in conjunction with techniques for nerve block at the knee and ankle.
Paravertebral Approaches to Blockade of the Lumbar Plexus
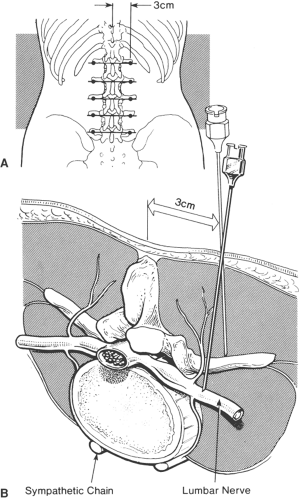
The lumbar plexus, as previously noted, is formed by the anterior (ventral) divisions of the first, second, third, and fourth lumbar nerves, with about 50% inclusion of a branch from the twelfth thoracic nerve and occasionally from the fifth lumbar nerve. The spinal nerve that leaves the spinal cord at each level is formed by the union of a ventral motor root with a dorsal sensory root. This mixed spinal nerve gives off a dorsal ramus, a ventral ramus, and a ramus communicans; the latter contributes to the formation of the sympathetic ganglion and trunk. The lumbar plexus is formed in front of the transverse processes of the lumbar vertebrae into a series of oblique loops that lie deep in the substance of the psoas major muscle and at the medial border of the quadratus lumborum muscle (Fig. 14-3). From here, the individual nerves form and course in the direction of their terminal innervation.
The relationship of the lumbar plexus to the sympathetic chain is important, since each may be blocked separately, but with a similar approach. The first and second lumbar spinal nerves, frequently the third, and sometimes the fourth, send communicating rami to form the lumbar portion of the sympathetic trunk. The sympathetic trunk lies on the ventrolateral surface of the lumbar and sacral bodies medial to the anterior foramina. It is apparent, therefore, that although these two nerve systems are separated by distance, muscle, and tissue planes, they have considerable intercommunication (Fig. 14-3).
Indications
The lumbar plexus supplies the cutaneous nerves not only to the upper thigh but also to the lower abdominal area. (Analgesia for the abdomen is covered more completely in Chapter 16.)
Branches of the first three lumbar nerves provide cutaneous distribution to the inner and outer aspects of the thigh and the posterior gluteal region, along with adjacent perineal and suprapubic areas. Complete lumbar plexus blockade may be accomplished by discretely blocking the five individual lumbar somatic nerves (assuring blockade of the iliohypogastric, ilioinguinal, genitofemoral nerves, if needed for the anticipated procedure) or with a single large injection (psoas compartment block). Recent applications have typically utilized the psoas compartment approach. Sacral blockade must also be performed to achieve complete blockade of the lower extremity.
Branches of the first three lumbar nerves provide cutaneous distribution to the inner and outer aspects of the thigh and the posterior gluteal region, along with adjacent perineal and suprapubic areas. Complete lumbar plexus blockade may be accomplished by discretely blocking the five individual lumbar somatic nerves (assuring blockade of the iliohypogastric, ilioinguinal, genitofemoral nerves, if needed for the anticipated procedure) or with a single large injection (psoas compartment block). Recent applications have typically utilized the psoas compartment approach. Sacral blockade must also be performed to achieve complete blockade of the lower extremity.
The psoas compartment block was first described by Chayen in 1976 (8). It can be performed as a single-injection technique or with a catheter placed for prolonged analgesia. It has been used to provide anesthesia for thigh surgery. In combination with parasacral nerve block, it has been used for hip fracture repair (9), to provide analgesia following total hip arthroplasty (THA) or total knee arthroplasty (TKA) (5,6,10,11), and also in the treatment of chronic hip pain (12).
Continuous psoas techniques have been described to provide analgesia following a variety of operations including THA, TKA, open reduction and internal fixation (ORIF) of acetabular fractures, ORIF of femur fractures, and anterior cruciate ligament reconstruction (5,10,11,13,14,15). Interest in this block developed as practitioners sought alternatives to neuraxial techniques that could provide consistent analgesia following hip, femur, and knee surgery.
Technique: Lumbar Paravertebral Nerve Block
The classic approach to blockade of the lumbar somatic nerves is paravertebral. The original block description of Labat advocates having the patient lie on the side opposite the one to be blocked (3). A soft roll placed between the iliac crest and the costal margin will minimize the lateral spinal curvature.
A preferred position, is that of having the patient lie prone over a soft pillow, which will flatten/minimize the lordotic curve. Regardless of patient position, the landmarks used are the spinous processes of the lumbar vertebrae. Skin wheals are raised opposite the cephalad aspect of the spinous processes, on a line 3 to 4 cm laterally from, and parallel to, the midline of the back (Fig. 14-4). Depending on the size of the patient, a 10- or 15-cm insulated needle is inserted through each of the skin wheals and advanced perpendicular to the surface of the skin until its tip comes into contact with the transverse process of the vertebral body, usually at a depth of 4 to 5 cm. The needle is then partially withdrawn and reintroduced slightly more cephalad and medially, making an angle of about 25 degrees with the sagittal plane of the body. This should allow the needle to pass just tangential to the superior aspect of the transverse process and to be advanced an additional 2 to 3 cm. Following elicitation of the appropriate motor response (abdominal wall versus lower extremity), 8 to 10 mL of the selected local anesthetic solution is injected.
A preferred position, is that of having the patient lie prone over a soft pillow, which will flatten/minimize the lordotic curve. Regardless of patient position, the landmarks used are the spinous processes of the lumbar vertebrae. Skin wheals are raised opposite the cephalad aspect of the spinous processes, on a line 3 to 4 cm laterally from, and parallel to, the midline of the back (Fig. 14-4). Depending on the size of the patient, a 10- or 15-cm insulated needle is inserted through each of the skin wheals and advanced perpendicular to the surface of the skin until its tip comes into contact with the transverse process of the vertebral body, usually at a depth of 4 to 5 cm. The needle is then partially withdrawn and reintroduced slightly more cephalad and medially, making an angle of about 25 degrees with the sagittal plane of the body. This should allow the needle to pass just tangential to the superior aspect of the transverse process and to be advanced an additional 2 to 3 cm. Following elicitation of the appropriate motor response (abdominal wall versus lower extremity), 8 to 10 mL of the selected local anesthetic solution is injected.
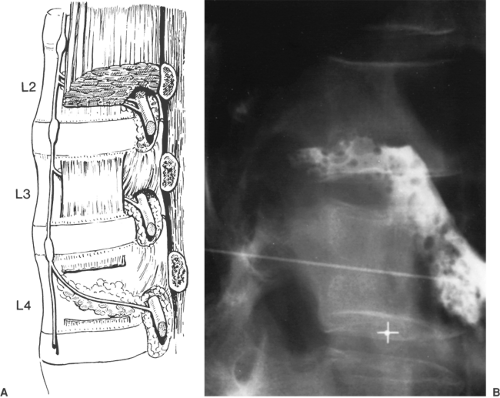 Figure 14-3. Relationship of lumbar somatic nerve roots to sympathetic chain. Note the separation of somatic and sympathetic nerves by the psoas major muscle; however, there is also a potential path of communication via the fibrous arch illustrated at the L4 level (see also Chapter 39). |
Importantly, the spinous processes of the lumbar vertebrae, unlike those of the thoracic vertebrae, do not slope downward, their upper and lower borders being more nearly horizontal. Their average thickness is from 0.5 to 1 cm. The distance between the tip of the lumbar spinous process and its attachment to the vertebral lamina is approximately 3 to 4 cm. A horizontal line drawn tangentially to the superior aspect of the spinous process will overlie the transverse process of that vertebrae. The transverse processes of the lumbar vertebrae are short, accounting for the paravertebral skin wheal being only 2 to 3 cm from the midline. The average depth of the transverse process to the skin is 5 cm, which varies with the size of the patient and the paraspinous musculature. The transverse processes of L4 and L5 are more deeply situated than are those of the vertebrae above. When the needle passes superior to the transverse process, it is in proximity to the somatic nerve of the preceding segment (the needle passing over the transverse process of L1 injects the T12 nerve root). The L5 root is blocked through the same skin wheal as L4, by redirecting the needle in a caudad direction until it passes from the lower border of the L4 transverse process and by injecting the nerve root in a manner similar to the technique used in other roots (Fig. 14-4, lower panel).
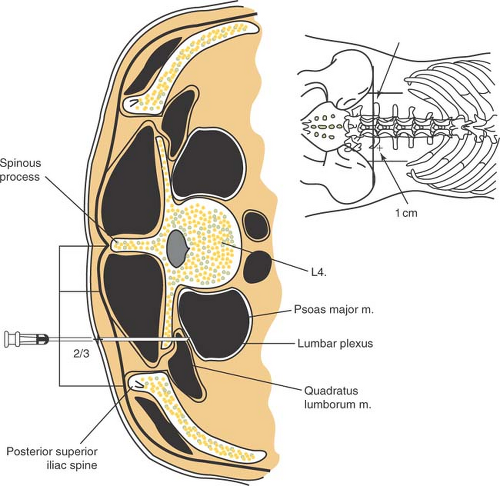
Technique: Psoas Compartment Block
Several descriptions of the needle entry site for the psoas compartment blocks have been described (5,7,16,17,18,19). All rely on bony contact with the transverse process as a guide to depth of needle placement. The patient is placed in the lateral position, hips flexed and operative extremity uppermost. A line is drawn to connect the iliac crests (intercristal line) identifying the fourth lumbar spine. After skin preparation, a skin wheal is raised 3 cm caudad and 5 cm lateral to the midline
on the side to be blocked. A 21-gauge, 10-cm stimulating needle is then advanced perpendicular to the skin entry site until it contacts the fifth lumbar transverse process. The needle is redirected cephalad until it passes the transverse process (Fig. 14-4, lower panel). Traversing from posterior to anterior at the level of L4–L5, the following structures would be encountered: posterior lumbar fascia, paraspinous muscles, anterior lumbar fascia, quadratus lumborum, and the psoas muscle (20). The common iliac artery and vein are situated anterior to the psoas muscle. The lumbar plexus is identified by elicitation of a quadriceps motor response, and 30 mL of solution is injected.
on the side to be blocked. A 21-gauge, 10-cm stimulating needle is then advanced perpendicular to the skin entry site until it contacts the fifth lumbar transverse process. The needle is redirected cephalad until it passes the transverse process (Fig. 14-4, lower panel). Traversing from posterior to anterior at the level of L4–L5, the following structures would be encountered: posterior lumbar fascia, paraspinous muscles, anterior lumbar fascia, quadratus lumborum, and the psoas muscle (20). The common iliac artery and vein are situated anterior to the psoas muscle. The lumbar plexus is identified by elicitation of a quadriceps motor response, and 30 mL of solution is injected.
Based on anatomic imaging studies, Capdevila et al. (5) modified the classic psoas technique. Needle insertion site is the junction of the lateral third and medial two thirds of a line between the spinous process of L4 and a line parallel to the spinal column passing through the posterior superior iliac spine (PSIS). (The spinous process of L4 was estimated to be approximately 1 cm cephalad to the upper edge of the iliac crests.) The needle is advanced perpendicularly to the skin until contact with the transverse process of L4 is obtained and advanced caudad off the transverse process until quadriceps femoris muscle twitches are elicited (Fig. 14-5). Despite a difference between men and women in the depth of the lumbar plexus (median values, 8.5 and 7.0 cm, respectively), the distance from the L4 transverse process to the lumbar plexus was comparable (median value, 2 cm) in both sexes. Thus, the authors stressed the importance of achieving contact with the L4 transverse process to establish appropriate needle depth and position.
Complications
The deep needle placement with the lumbar paravertebral and psoas compartment approaches increases the risk of possible renal hematoma, retroperitoneal hematoma, pneumocele, and unintended intra-abdominal and intervertebral disk catheter placement (5,21,22,23,24). Seizures have been reported following negative aspiration and intermittent injection (25). To ensure the proper position of the needle during these deep techniques and to avoid excessive needle insertion, it is recommended that the transverse process be intentionally sought. Peripheral nerve damage is also a potential risk with this technique. A side effect of the paravertebral approach to the lumbar plexus is the development of a sympathetic block secondary to spread of local anesthetic. This unilateral sympathectomy is usually of little consequence.
Epidural spread of local anesthetic is another common side effect of psoas compartment block, occurring in 9% to 16% of adult patients (7,26). In children, Dalens et al. reported a greater than 90% incidence of epidural spread when using the original landmarks of Chayen, compared to no epidural spread when using the landmarks as modified by Winnie (27). This side effect is usually attributed to retrograde diffusion of the local anesthetic to the epidural space when large volumes of local anesthetic are used (greater than 20 mL). In most cases, residual lumbar plexus blockade is apparent after the resolution of the contralateral block. However, there are case reports of total spinal anesthesia occurring during lumbar plexus blockade, and vigilance must be maintained during the management of this block (22,28,29).
Blockade of Branches of the Lumbar Plexus
Femoral Nerve Block
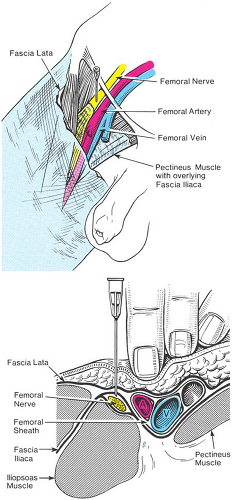
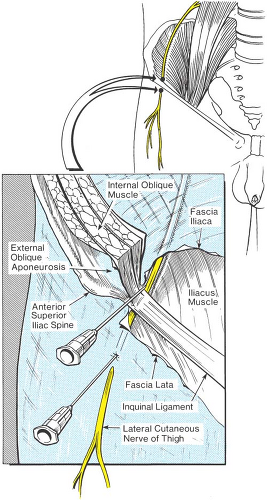
The femoral nerve is formed by the dorsal divisions of the anterior rami of the second, third, and fourth lumbar nerves. The femoral nerve emerges from the psoas muscle in a fascial compartment between the psoas and iliacus muscles, where it gives off articular branches to the hip. It enters the thigh posterior to the inguinal ligament. There it lies lateral and posterior to the femoral artery. This relationship to the femoral artery exists near the inguinal ligament, but not after the nerve enters the thigh. As the nerve passes into the thigh, it divides into an anterior and a posterior division and quickly arborizes. At the level of the inguinal ligament, dense fascial planes are present: the fascia lata and fascia iliaca (Fig. 14-6). The femoral nerve is situated deep to these fascial planes. The femoral artery, vein, and lymphatics reside in a separate fascial compartment medial to the nerve.
The anterior division of the femoral nerve gives off the medial and intermediate cutaneous nerves that supply the skin of the medial and anterior surfaces of the thigh. The muscular branches of the anterior division of the femoral nerve supply the sartorius muscle and the pectineus muscle and articular branches to the hip. The posterior division of the femoral nerve gives off the saphenous nerve, which is the largest cutaneous branch of the femoral nerve, and the muscular branches to the quadriceps muscle and articular branches to the knee.
The terminal nerves of the posterior division of the femoral nerve, the saphenous and the vastus medialis nerves, continue distally through the adductor canal. The saphenous nerve exits from the lower part of the canal, emerging between the sartorius and gracilis muscles, where is gives off an infrapatellar branch. The nerve becomes subcutaneous below the sartorius at the medial side of the knee. It descends down the medial border of the tibia immediately behind the long saphenous vein, although its course can be quite variable. The nerve crosses with the vein in front of the medial malleolus and extends as far as the base of the great toe. The saphenous nerve supplies an extensive cutaneous area over the medial side of the knee, leg, ankle, and foot (Fig. 14-2).
Indications
Indications for single-injection femoral nerve block include anesthesia for knee arthroscopy in combination with intra-articular local anesthesia, and analgesia for femoral shaft fractures, anterior cruciate ligament reconstruction (ACL), and TKA as a part of multimodal regimes (30,31,32,33,34,35). Their use in complex knee operations is associated with lower pain scores and fewer hospital admissions following same-day surgery (36).
Technique: Femoral Nerve Block
The patient lies supine with the anesthesiologist standing next to the side that is to be blocked. After careful palpation, a skin wheal is raised just lateral to the femoral artery, where it emerges distal to the inguinal ligament (Fig. 14-6). A 22-gauge 5-cm insulated needle is inserted just over the tip of the palpating finger in a cephalad direction. Commonly, the anterior branch of the femoral nerve will be identified first. Vloka et al. reported this to be the first motor response elicited 97% of the time (37). Stimulation of this branch leads to contraction of the sartorius muscle on the medial aspect of the thigh and should not be accepted, as the articular and muscular branches derive from the posterior branch of the femoral nerve. The needle should be redirected slightly laterally and with a deeper direction to encounter the posterior branch of the femoral nerve. Stimulation of this branch is identified by patellar ascension as the quadriceps contract. The needle is then fixed and a volume of 25 to 30 mL of local anesthetic is injected.
Three-in-One Block versus Femoral Block
During femoral nerve block, it has been advocated to use a higher volume of local anesthetic and apply firm pressure just
distal to the needle during and a few minutes after injection to block the femoral, lateral femoral cutaneous, and obturator nerves, the so named “three-in-one block” (38). However, despite many efforts to consistently produce a three-in-one block, the effectiveness of these maneuvers has not been demonstrated. In most reports, the femoral nerve is the only nerve consistently blocked with this approach (39,40,41,42). Blockade of the lateral femoral cutaneous nerve occurs through lateral diffusion of local anesthetic and not through proximal spread to the lumbar plexus (41). The obturator nerve is less frequently anesthetized during three-in-one block than the lateral femoral cutaneous nerve, which is not surprising given the number of fascial barriers between these structures at the level of the inguinal ligament. As a result of the lack of scientific support for the term “three-in-one,” the perivascular or three-in-one approach is now most often referred to as a femoral nerve block.
distal to the needle during and a few minutes after injection to block the femoral, lateral femoral cutaneous, and obturator nerves, the so named “three-in-one block” (38). However, despite many efforts to consistently produce a three-in-one block, the effectiveness of these maneuvers has not been demonstrated. In most reports, the femoral nerve is the only nerve consistently blocked with this approach (39,40,41,42). Blockade of the lateral femoral cutaneous nerve occurs through lateral diffusion of local anesthetic and not through proximal spread to the lumbar plexus (41). The obturator nerve is less frequently anesthetized during three-in-one block than the lateral femoral cutaneous nerve, which is not surprising given the number of fascial barriers between these structures at the level of the inguinal ligament. As a result of the lack of scientific support for the term “three-in-one,” the perivascular or three-in-one approach is now most often referred to as a femoral nerve block.
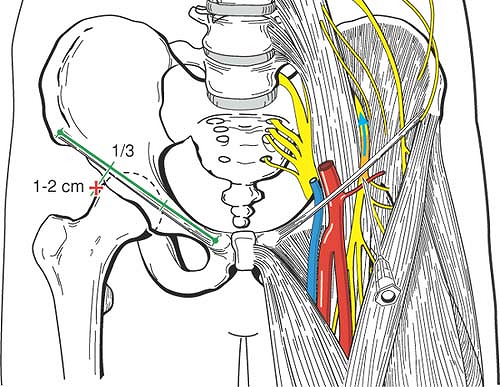
Technique: Modified Femoral (Fascia Iliacus) Block
Dalens originally described the fascia iliacus block in children (43). The indications for its use are the same as those for single-injection femoral nerve block (44). Advocates believe its utility lies in the “double-pop” technique for applying this block. The double-pop refers to the sensation felt as the needle traverses the fascia lata then the fascia iliaca. Penetration of both layers of fascia is important for successful fascia iliacus blockade. To facilitate the appreciation of the “clicks” or “pops,” the use of a short bevel- or pencil-tipped needle has been advocated to provide more tactile feedback than cutting needles. This technique does not require a nerve stimulator; however, confirmatory motor responses may be sought. The needle entry site for the fascia iliacus block is determined by drawing a line between the pubic tubercle and the anterior superior iliac crest and dividing this line into thirds. The needle entry point is 1 cm caudal to the intersection of the medial two-thirds and lateral one-third along this line. This site is well away from the femoral artery, making this useful for patients in whom femoral artery puncture is contraindicated (Fig. 14-7).
Continuous Femoral and Fascia Iliacus Blockade
Continuous femoral and fascia iliacus block have been shown to improve outcome following major knee and vascular surgery of the lower extremity compared to intravenous (IV) narcotic
therapy or continuous infusion or injection of analgesics (45,46,47,48,49,50,51,52,53).
therapy or continuous infusion or injection of analgesics (45,46,47,48,49,50,51,52,53).
However, both continuous techniques have been associated with a high rate of inaccurate catheter placement. In a prospective study, Capdevila et al. showed that continuous femoral nerve block using a standard approach led to unpredictable catheter placement, with only 25% of the catheters lying near the lumbar plexus (54). Most often the catheters tended to course medially in the direction of the psoas muscle or laterally in the direction of the iliacus muscle. The accuracy of final catheter placement correlated with the degree of analgesia following proximal lower limb surgery (54). Ganapathy et al. (52) reported similar results with final placement of fascia iliaca catheters; CT scans noted only 40% of catheters placed were ideally positioned (superior to the upper third of the sacroiliac joint in the psoas sheath). Comparing a stimulating catheter to a nonstimulating catheter, Salinas et al. were able to increase the success rate of continuous femoral nerve block in volunteers from 85% to 100% (55).
Technique: Saphenous Nerve Block
Saphenous nerve blocks are commonly performed as a component of knee and ankle blocks. Supplemental block of the saphenous nerve is required for surgical procedures to the medial aspect of the leg, ankle, and foot, or when a tourniquet or Esmarch bandage is applied. Patients with thigh tourniquet placement require a more proximal block near the saphenous nerve origin in the femoral triangle. Various nerve block approaches are described, from its origin in the femoral triangle to the medial malleolus.
Saphenous Nerve Block at the Level of the Femoral Triangle
The patient is positioned supine with the leg extended at the knee and the long axis of the foot at a 90-degree angle to the table. The anesthesiologist stands at the side to be blocked. The femoral artery pulse is palpated and marked. Needle insertion site is 1 to 2 cm lateral to the artery and medial to the upper border of the sartorius muscle. A 22-gauge 5-cm insulated needle is introduced perpendicular to the skin at the needle insertion site and advanced until an evoked vastus medialis muscle response is elicited at 0.5 mA or less. A total of 5 to 10 mL of solution is injected incrementally after negative aspiration. Alternatively, a more proximal block of the femoral nerve may be performed as described earlier if total volume of anesthetic solution is not of concern (see Fig. 14-6).
Saphenous Nerve Block at the Level of the Knee
Saphenous nerve blocks at the level of the knee are based on the relationship of the nerves to the superior pole of the patella, tibial tuberosity, medial head of gastrocnemius muscle, sartorius muscle, and saphenous vein. No motor response is sought with distal saphenous approaches, since the saphenous nerve is purely sensory, distal to the femoral triangle. However, the nerve may be localized using a nerve stimulator and eliciting sensory “electrical” pulsations (56,57).
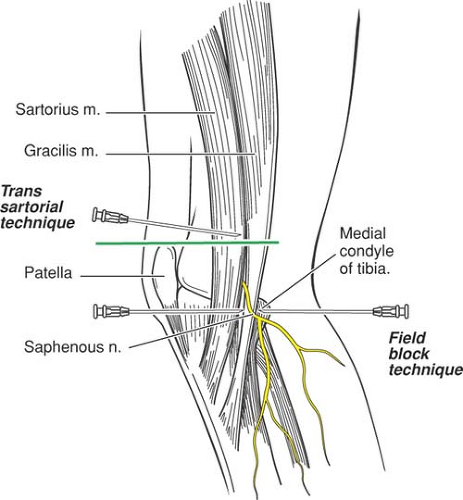
Field Block Technique
The patient is positioned supine with the leg extended at the knee. A 25-gauge 5-cm needle is inserted above the medial surface of the tibia and 5 to 7 mL of solution is infiltrated subcutaneously in a fan-like pattern. Classically, this saphenous nerve block was performed as a blind subcutaneous infiltration over the medial surface of the tibia (between the tibial tuberosity and the medial head of the gastrocnemius muscle) (Fig. 14-8). However, success rates with this technique ranged between 33% and 65%.
Transsartorial Technique
The patient is positioned supine with the leg extended at the knee. The sartorius muscle is palpated on the medial side, just above the knee joint. At the level of the upper pole of the patella, a 22-gauge 5-cm needle is advanced 45 degrees from the coronal plane, through the muscle belly of the sartorius, until a fascial pop or click is noted (1.5–3 cm) (Fig. 14-8). After negative aspiration, 10 mL of local anesthetic is injected. Success rates for the transsartorial approach are 70% to 80% (58).
Paravenous Technique
The patient is placed supine with the leg extended at the knee. Below the knee, the saphenous nerve is immediately adjacent to the saphenous vein. The saphenous vein is identified by placing a thigh tourniquet and allowing the leg to dangle for at least 60 seconds. Ultrasound guidance also may be helpful. A subcutaneous paravascular injection is performed using a 25-gauge 5 cm needle with 5 mL of local anesthetic on each side of the vein, taking care to avoid IV injection. The success rate is approximately 100%. However, painless hematomas often occur with this approach (59).
Complications
Intravascular injection and hematoma are possible because of the close proximity of vascular structures throughout the
course of the nerve. However, anatomically, the nerve and femoral artery are located in separate sheaths approximately 1 cm apart (Fig. 14-6). In most patients with normal anatomy, the femoral artery can be easily palpated, allowing correct, safe needle positioning lateral to the pulsation. The presence of femoral vascular grafts is a relative contraindication to femoral block; however, the fascia iliacus approach may be utilized in these patients because of the lateral needle insertion site. Nerve damage is rare with this technique (60). Both local inflammation and proximal abscess have been reported with indwelling catheters (1). Finally, the presence of femoral or combined femoral–sciatic block may lead to lateral gait instability, resulting in difficulty with pivoting maneuvers and patient falls (61).
course of the nerve. However, anatomically, the nerve and femoral artery are located in separate sheaths approximately 1 cm apart (Fig. 14-6). In most patients with normal anatomy, the femoral artery can be easily palpated, allowing correct, safe needle positioning lateral to the pulsation. The presence of femoral vascular grafts is a relative contraindication to femoral block; however, the fascia iliacus approach may be utilized in these patients because of the lateral needle insertion site. Nerve damage is rare with this technique (60). Both local inflammation and proximal abscess have been reported with indwelling catheters (1). Finally, the presence of femoral or combined femoral–sciatic block may lead to lateral gait instability, resulting in difficulty with pivoting maneuvers and patient falls (61).
Obturator Nerve Block
The obturator nerve (L2–L4) derives its major source from L3–L4—the portion coming from L2 is very small and sometimes even lacking. The nerve appears at the medial border of the psoas muscle, covered anteriorly by the external iliac vessels, and passes downward in the pelvis. It continues with the obturator vessels along the obturator groove and passes through the obturator foramen into the thigh. As the nerve passes through the obturator canal, it divides into posterior and anterior branches. The anterior branch supplies an articular branch to the hip joint, the anterior adductor muscles, and cutaneous branches to the lower inner thigh (Fig. 14-2). The size or existence of this cutaneous innervation is small and variable depending on which anatomic reference material is quoted; recent investigations suggest that the only way to effectively evaluate obturator nerve function is to assess adductor strength (62,63). The posterior branch innervates the deep adductor muscles and frequently sends an articular branch to the knee joint, which may be important in providing analgesia for knee surgery.
Some anatomic descriptions include an accessory obturator nerve that leaves the medial border of the psoas muscle in company with the obturator nerve. It has been said to be incorrectly named, having much more in common with the femoral nerve (64). Like the femoral nerve, it passes over, not under, the pubic ramus where it supplies the pectineus muscle. It is present in about one third of individuals.
Indications
Indications for a single-injection obturator nerve block are generally limited to diagnostic applications or therapeutic relaxation of the adductor muscles of the thigh (65). Despite the significant amount of literature that has been devoted to anesthetic sparing of this nerve with many approaches to the lumbar plexus, only two studies have examined the effect of the addition of an obturator nerve block to improve analgesia after major knee surgery (66,67). Both studies reported a decrease in opioid consumption and pain scores in patients undergoing TKA receiving obturator nerve block in addition to a femoral or femoral and sciatic nerve block.
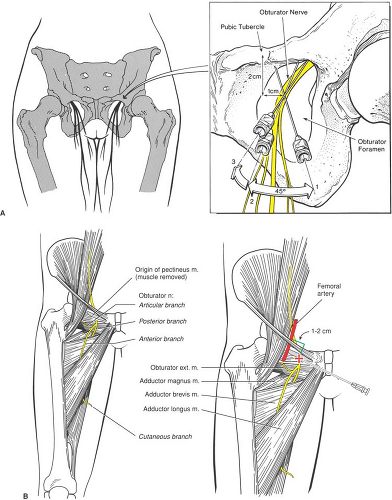
Technique: Obturator Nerve Block
The patient is placed supine with the leg to be blocked in slight abduction. Caution should be taken to protect the skin of the genitalia from irritating antiseptic solutions used in preparing the area. It is not necessary to shave the pubic area. A skin wheal is raised at a point 1 to 2 cm lateral and 1 to 2 cm caudad to the pubic tubercle, and a 22-gauge, 8- to 10-cm needle is advanced perpendicular to the skin entry site with a slight medial direction. The inferior pubic ramus is encountered at a depth of 2 to 4 cm, and the needle is walked in a lateral and caudad direction, until it passes into the obturator canal. Identification of the bony wall verifies that the needle has passed into the canal rather than into the soft tissues (e.g., bladder or vagina) medially or superiorly (Fig. 14-9A). The obturator nerve is located 2 to 3 cm past the initial point of contact with the pubic ramus. After negative aspiration, 10 to 15 mL of local anesthetic is injected. A nerve stimulator is helpful in locating the obturator nerve; correct needle position is evidenced by contraction of the adductor muscles of the medial thigh. The presence of successful obturator nerve block is determined by demonstrating paresis of the adductor muscles, since the cutaneous distribution is small and inconstant.
The classic approach to obturator nerve block involves painful periosteal contact and multiple needle redirection. An alternate interadductor approach was described by Wasseff (65). In this technique, the needle is inserted behind the adductor tendon, near its pubic insertion, and is directed laterally toward a mark on the skin 1 to 2 cm medial to the femoral artery and immediately below the inguinal ligament, representing the obturator canal. The nerve is identified by a motor response to peripheral nerve stimulation in the adductor muscle (Fig. 14-9B).
A modification of this technique advocates searching for paresthesias to the area of the inner thigh (68). If paresthesias are not elicited, then it is suggested that a fan-like wall of anesthesia be deposited. The major difference in the two techniques lies in a greater attempt to palpate the tendon on the adductor longus muscle, which constitutes the upper medial aspect of the obturator foramen. With gentle, deep palpation, one may be able to palpate the entire foramen and, placing the skin wheal inferior to the midpoint of the superior pubic ramus, gain a more precise location of the obturator nerve.
Complications
Obturator nerve block has vascular and neural complications and side effects nearly identical to those of the femoral nerve.
Lateral Femoral Cutaneous Nerve Block
The lateral femoral cutaneous nerve (L2–L3) emerges at the lateral border of the psoas muscle at a level lower than the ilioinguinal nerve. It passes obliquely under the fascia iliaca and across the iliac muscle to enter the thigh deep to the inguinal ligament, at a point approximately 1 to 2 cm medial to the anterior superior iliac spine (Fig. 14-10). It then crosses or passes through the tendinous origin of the sartorius muscle, and courses downward beneath the fascia lata. It emerges from the fascia lata at a point 7 to 10 cm below the anterior superior iliac spine, where it branches into anterior and posterior branches. The anterior branch supplies the skin over the anterolateral aspect of the thigh as low as the knee. The posterior branch pierces the fascia lata and passes backward to supply the skin on the lateral side of the thigh from just below the greater trochanter to about the middle of the thigh (Fig. 14-10).
Indications
The lateral femoral cutaneous nerve of the thigh is a purely sensory nerve that supplies a large but variable area from the inguinal ligament to the knee on the lateral aspect of the thigh (69). Lateral femoral cutaneous nerve block is most commonly used as the sole anesthetic during diagnostic muscle biopsy and harvesting of split thickness skin grafts (70,71). It has also been used to provide analgesia in elderly patients undergoing hip fracture repair (72). However, in a study comparing lateral femoral cutaneous nerve block, femoral nerve block, and patients receiving no block following femoral neck repair, lateral femoral cutaneous nerve block was not as effective at controlling postoperative pain as femoral nerve block (73). Femoral nerve block has been reported following lateral femoral cutaneous block (74). This is not surprising given the bulk of data reporting spread to the lateral femoral cutaneous nerve during femoral nerve block (Fig. 14-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree