FIG. 17.1 Layers of epidermis. (From Monahan FD, et al.: Phipps’ medical-surgical nursing health and illness perspectives, ed 8, St. Louis, MO, 2007, Elsevier.)
The granular layer, or stratum granulosum, contains three or four layers of cells. It is composed of cells called keratinocytes, which undergo a maturation process called keratinization. This process produces lipid granules that form waterproof structures and helps prevent fluid loss and evaporation through the skin into the environment.
Dermis
The dermis, or corium, lies under the epidermis and consists of collagen, elastic, and reticular fibers. It also contains blood vessels, nerves, the lymphatics, and smooth muscle. It is responsible for the stretching of skin during movement as well as being the location that the structures for hair growth are located.
Hypodermis
The hypodermis, also called the subcutaneous layer, functions as a shock absorber and heat insulator. Located under the dermis, it comprises fat or adipose tissue, smooth muscle, and adipocytes. These cells store and accumulate necessary fats. The hypodermis acts as a site of energy production and insulation. This area of the body stores fat in characteristic locations: the hips on women and the abdomen in men.1,2
Integumentary Functions
The skin has many functions, the most important of which is to act as a barrier between the internal and external environments. In addition, the skin has an essential role in body temperature and fluid regulation, excretion, secretion, vitamin D production, sensation, appearance, and probably many other functions that have yet to be determined.
Thermoregulation
Skin, subcutaneous tissue, and fat in the subcutaneous tissue provide heat insulation for the body. Heat is lost from the body to the surroundings through radiation, conduction, convection, and evaporation (Fig. 17.2).3 Radiation of heat from the body accounts for approximately 60% of total heat loss. In this method, heat is lost in the form of infrared heat waves. Conduction of heat to objects represents approximately 3% of the total heat loss, whereas conduction of heat to the air represents approximately 15% of the total heat loss. When water is carried away from the skin by air currents, convection of heat occurs. Evaporation constitutes approximately 22% of the heat loss. Even without sweating, water still evaporates from the skin and the lungs; this is called insensible loss and totals approximately 600 mL/day.3
The skin regulates body temperature by conserving heat in a cold environment and lowering the temperature in hot environments through sweating. The sweat glands are innervated by the sympathetic and parasympathetic nervous systems. When the anterior hypothalamus in the preoptic area of the brain is stimulated by excess heat, impulses are sent from this area by way of the autonomic pathways to the spinal cord. From the spinal cord through the sympathetic outflow tracts, the impulses go to the skin all over the body. The sweat glands are innervated by sympathetic nerve fibers. However, in these specific fibers, the neurotransmitter is acetylcholine. Consequently, these fibers are actually sympathetic cholinergic nerve fibers and are stimulated by epinephrine or norepinephrine. Norepinephrine is a catecholamine that is both a hormone and neurotransmitter that assists with the fight-or-flight response. It is responsible for cutaneous vasoconstriction and has been associated with the pain of fibromyalgia.4
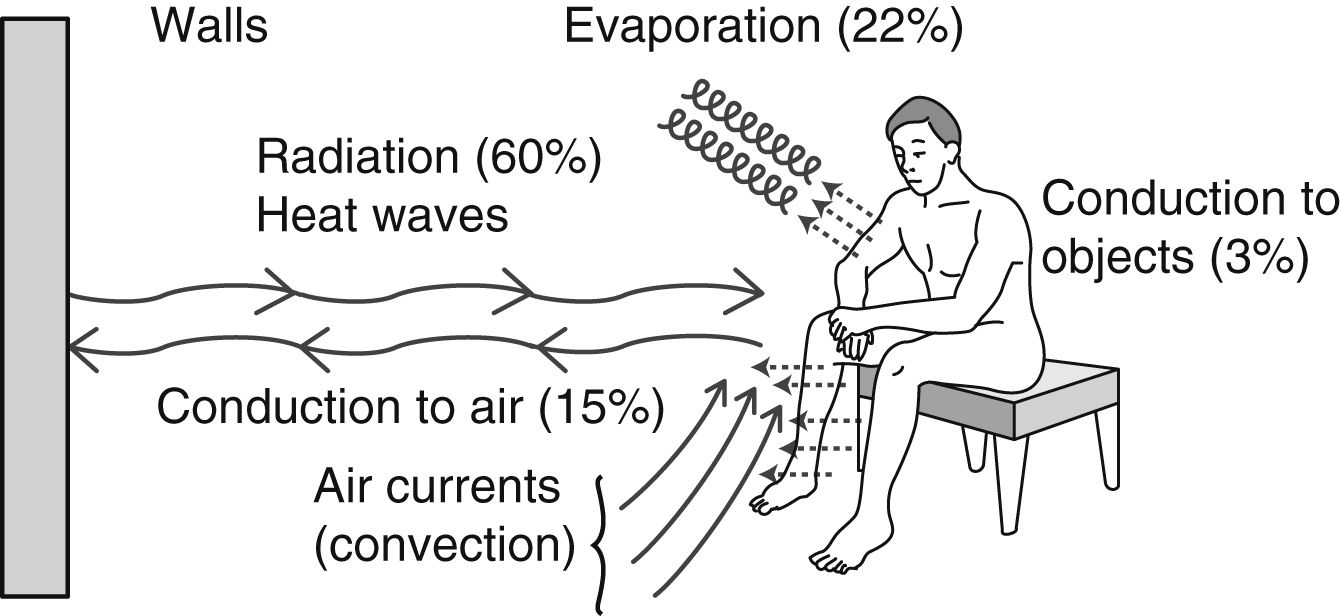
FIG. 17.2 Major mechanisms of heat loss from body. (From Hall JE: Guyton and Hall textbook of medical physiology, ed 13, St. Louis, MO, 2016, Elsevier.)
The sweat gland consists of two portions: a deep subdermal coiled portion that secretes sweat and a duct portion that conducts sweat to the skin. Sweat has a pH of 3.8 to 6.5 and contains sodium, chloride, potassium, calcium, lactic acid, and urea; therefore, sweating is an act of excretion and secretion.
Protection
The skin protects the body from injurious physical, chemical, electric, thermal, or biological stimuli. Of particular importance to the perianesthesia nurse is the presence of bacteria and viruses on the skin that can cause infection when a patient’s skin barrier is broken. Normal florae of the skin include Staphylococcus, Streptococcus, and Corynebacterium organisms. Diphtheroids are also widely distributed on the skin, especially in moist areas. The normal pH of the skin is an acidic 4 to 6.5 resulting from production of lactic acid and residues of amino acids. This slightly acid environment serves as a protective mechanism by inhibiting bacterial growth. Diabetic, cardiac, and renal patients tend to have more alkaline skin surfaces, thus being at higher risk for skin infections.5
When intact, the skin stops unwanted organisms from entering the body and, at the same time, prevents the loss of water, electrolytes, and proteins to the external environment. When the skin is broken (e.g., surgical incision, ulceration, abrasion, rash, venipuncture), the barrier between the internal and external environments is broken, which is why aseptic technique is important whenever a break of the skin is anticipated or has occurred.
Importance of Aseptic Technique
Because all skin has disease-causing organisms on its surface, skin can never be sterile. Precautions should be taken to reduce the number of pathogenic organisms that may be introduced into a wound. Good handwashing remains the most important activity in the prevention of disease transmission. The development and use of alcohol-based gel handwashing solutions has led to improved rates of handwashing compliance by health care providers. Nonetheless, establishment and availability of these products alone—without associated behavioral modification programs—have proven unsuccessful. Hands should be washed at the very least according to the World Health Organization’s Guidelines (“Five Moments for Hand Hygiene”) using either traditional handwashing techniques or using one of the new sanitizing gels before caring for any patient.6 When hands are visibly soiled, traditional washing should occur (Box 17.1).7 (See Chapter 5 for more information on handwashing and prevention of infection.)
A patient’s surgical wound site should be kept clean, and the dressings should remain sterile, dry, and intact. If any question arises about sterility or dressing integrity because of excess bleeding, fluid, or physical contamination, the dressing should be changed per protocol. Special precautions to reduce the introduction of opportunistic organisms should be taken with patients prone to infection. This group includes patients who are obese, anemic, or debilitated; those with vascular insufficiency, chronic obstructive pulmonary disease, and diabetes mellitus; and those with an immune deficiency including patients who are undergoing chemotherapy or chronic steroid therapy or who have acquired immunodeficiency syndrome. Aseptic technique in wound care for these patients should include isolation techniques such as wearing a surgical mask and using sterile gloves and drapes. Additionally, all gloves should be removed and discarded and hands washed after every single patient care encounter.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








