FIG. 16.1 The digestive system and its associated structures.
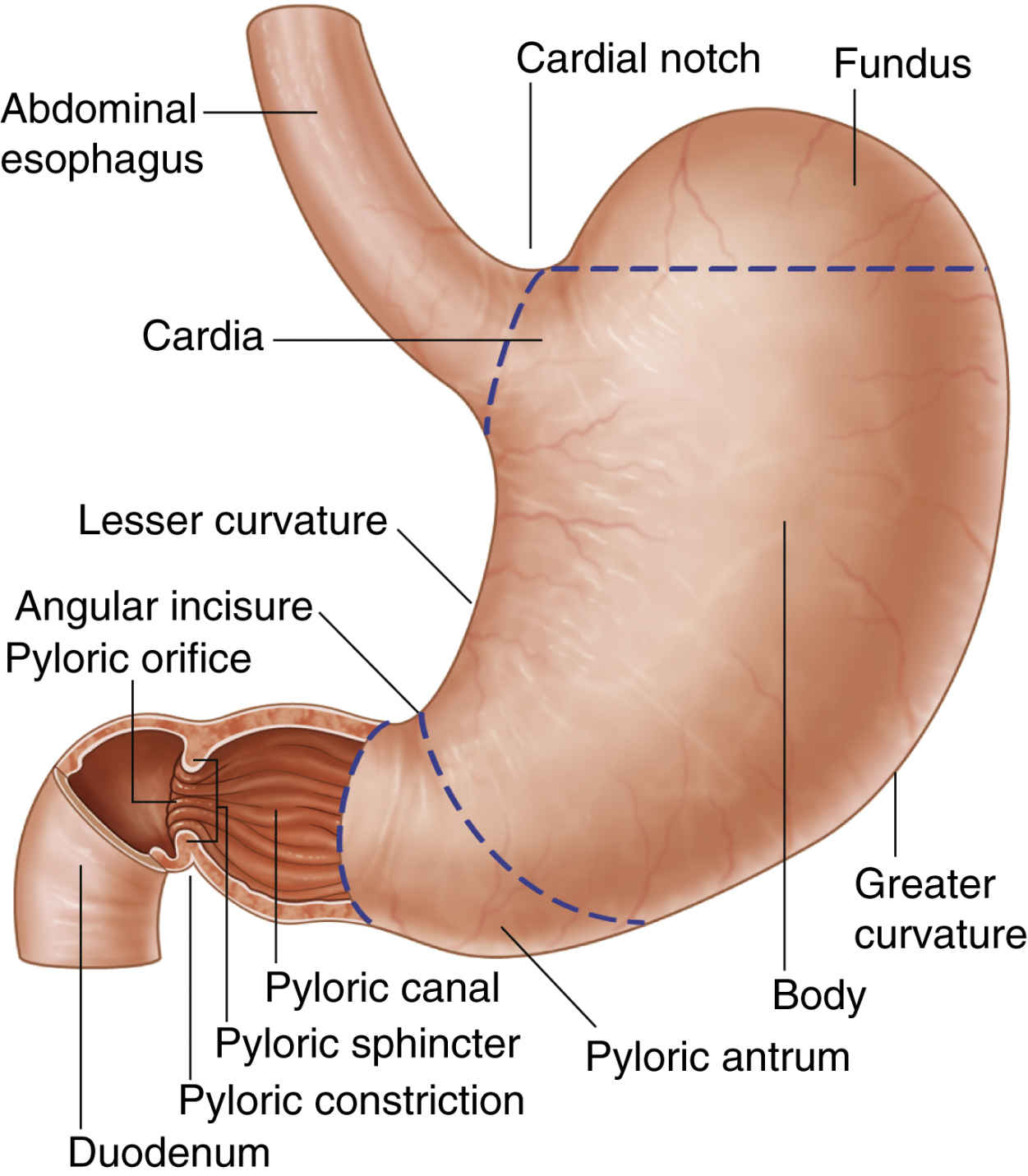
The Stomach
The stomach can be anatomically divided into the following three sections: the fundus, the body, and the pyloric portion (Fig. 16.2). The fundus is the dome of the stomach where peptic juice is secreted. The body is the middle portion of the stomach and is lined with parietal cells that secrete hydrochloric acid. The pH of the solution as secreted is approximately 0.8, which is extremely acidic. The total gastric secretion on a 24-hour basis is approximately 2 L with a normal pH of 1 to 3.5. The production of hydrochloric acid by the parietal cells is mediated by histamine, vagal stimulation, and the hormone gastrin. Blocking the histamine receptor (H2) by drugs such as cimetidine or ranitidine to reduce acid production is a common treatment for acid reflux. The third portion of the stomach is the pyloric portion where thick viscous mucus and the hormone gastrin are secreted. At the end of the antrum is the pylorus, an opening surrounded by a strong band of smooth muscle creating the pyloric sphincter that controls the amount of gastric contents that enter the duodenum.4
The vagus nerves (the primary nerves for the outflow of the parasympathetic nervous system) provide the predominant nerve supply to the stomach. Stimulation of the vagus causes increased motility of the stomach and the secretion of stomach acid, pepsin, and gastrin. As a result, a vagotomy is sometimes performed during gastric surgery to decrease gastric motility and acid production. This procedure used to be a common surgical treatment for peptic ulcer disease but is rarely performed now because of great improvements in the medical management of this disorder.
Nervous and hormonal stimulation have profound effects on gastric volume and pH. More specifically, stimulation of the parasympathetic nervous system causes increased gastric secretion, and stimulation of the sympathetic nervous system causes decreased gastric secretion. Consequently, pain and fear, which activate the sympathetic nervous system, decrease gastric emptying. In addition, the administration of opioids and active labor prolong gastric emptying. Food, depending on the type and amount, passes through the stomach at a variable rate. For example, foods rich in carbohydrates pass through the stomach in a few hours, whereas proteins exit more slowly. The emptying time for fats is the slowest. Fluids, however, pass through the stomach rather rapidly. In fact, 90% of 750 mL of ingested saline solution exits the stomach within 30 minutes. In addition, 150 mL of fluids taken 1 or 2 hours before induction of anesthesia stimulates peristalsis and facilitates gastric emptying. Consequently, the small sips of water taken with the preoperative oral medications may in fact contribute to lower intraoperative and postoperative gastric volumes. It must be emphasized that fasting, regardless of the duration, does not guarantee that the stomach is completely empty of fluids or food. Current guidelines for preoperative fasting are discussed fully in Chapter 14.5,6
Effect of Pregnancy on Gastric Motility and Secretions
During pregnancy, many alterations occur as a result of the enlarged uterus and altered hormonal state. Because of the enlarged uterus, the stomach and intestine are moved cephalad, and the axis of the stomach is shifted to a more horizontal position. The gastric emptying time is increased in women who are at least 34 weeks pregnant. In regard to the gastric volume and pH, no difference between pregnant and nonpregnant states seems to exist. Consequently, pregnant patients who have had nothing by mouth (NPO) for elective surgery do not have any additional risk of aspiration pneumonitis than do nonpregnant patients. However, research findings suggest that pregnant patients who have heartburn may be at greater risk for regurgitation and subsequent development of aspiration pneumonitis. In addition, if intramuscular opioids are given during labor, gastric emptying time is substantially delayed. Epidural anesthesia with local anesthetics does not seem to affect gastric volume or pH; however, if opioids are introduced into the epidural space, a delay in gastric emptying occurs.7,8
Postoperative Nausea and Vomiting
PONV continues to be ongoing concern to anesthesia providers and patients alike. Occurring in as many as one third of all surgical patients and in 80% of high-risk patients, PONV is the most commonly occurring postoperative complication. Nausea and vomiting involves a complex interplay among various structures in the body including the vomiting center in the brainstem, the closely associated chemoreceptor trigger zone, the vestibular labyrinth in the ear, vagal afferent neurons in the gastrointestinal tract, the limbic system, and the cerebral cortex. Each of these sites contributes to the triggering of vomiting by releasing single or multiple neurotransmitters including serotonin (5HT), acetylcholine, histamine, dopamine, and neurokinins. Adding to the complexity, these anatomic structures often possess a variety of receptors for each of the neurotransmitters, each receptor producing its own specific physiologic result when stimulated. Current practice guidelines covering the prevention and management of PONV and the care of patients experiencing PONV are presented in Chapter 29.9
The Intestine
The duodenum, the first part of the small intestine, arises at the pylorus of the stomach and stretches 25 to 30 centimeters to the duodenojejunal junction. The duodenum is a C-shaped tubular structure located below the stomach. The ampulla of Vater located in the duodenum is the confluence of the common bile duct draining bile from the gallbladder and the pancreatic duct draining digestive enzymes from the pancreas. The main functions of the stomach and the duodenum are to transform solid food into liquid slurry, regulate the entry of this slurry into the rest of the digestive tract, and supply enzymes for digestion.
The jejunum begins at the distal end of the duodenum at the duodenojejunal angle. It constitutes the first two fifths of the small intestine, and the ileum occupies the distal three fifths of the small intestine. The mesentery, which contains blood vessels, nerves, lymphatics, lymph nodes, and fat, stabilizes the small bowel and prevents it from twisting and constricting its blood supply.
The majority of digestion and nutrient absorption occurs in the small intestine. With the digestive enzymes from the stomach and the additional enzymes from the pancreas and bile salts from the gallbladder, most of the breakdown and digestion of food take place in the duodenum. The jejunum and ileum have special microscopic structures called microvilli that increase the surface area of these portions of the small intestine, allowing for absorption of nutrients, vitamins, minerals, and medications. By the time the remnants of a meal have reached the end of the small intestine almost all of the nutritional value has been removed.10,11
Sodium is absorbed by the small intestine at a rate of 25 to 35 g/day. This absorption accounts for approximately 16% of all the sodium in the body. When a patient has extreme diarrhea, sodium can be depleted to a lethal level within a few hours.10,11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree