where h is ventricle thickness, EDV is the end diastolic volume, and EDR is the end diastolic radius.
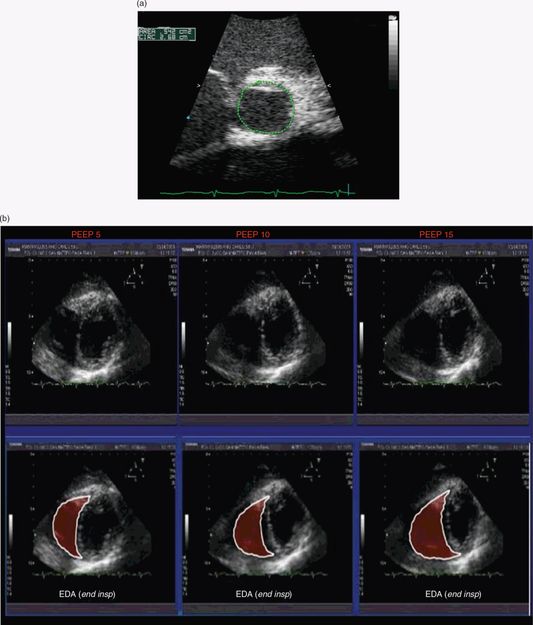
Figure 24.1 Left ventricular end diastolic area (EDA) as an estimation of preload. (a) Parasternal short-axis view. Using the caliper trace along the endocardium to measure the area of the LV at end diastole. (b) The effect of PEEP on EDA. Effects of PEEP of 5, 10, and 15 cm H2O on the right ventricle.
Trans-mitral flow estimation of LV end diastolic pressure (EDP) can be utilized during the weaning process from mechanical ventilation.
When encountering difficulties weaning or extubating a child from ventilatory support, it is often useful to evaluate the vocal cords and diaphragm for dysfunction. During spontaneous respirations, the clinician should be able to see the movement of the diaphragm, so as to differentiate between paradoxically moving, non-moving, or a weakly moving hemidiaphragm. Evaluation by M-mode can also be helpful in determining whether diaphragmatic dysfunction is present (Figure 24.2). Vocal cord paralysis can also be evaluated (Figure 24.3).

Figure 24.2 Diaphragm imaging. (a) The diaphragm in B-mode (arrow). (b) The evaluation of the diaphragm in M-mode, with normal movement of the diaphragm. (c) No movement of the diaphragm on M-mode.
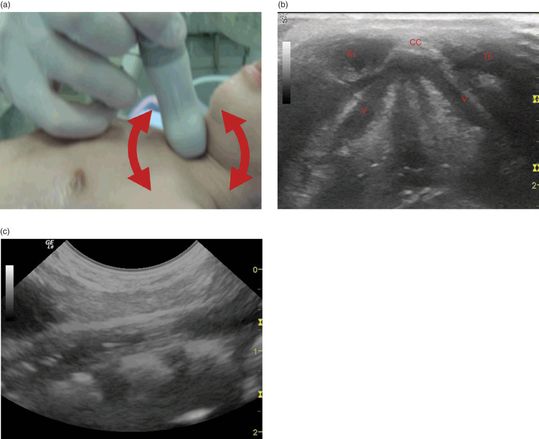
Figure 24.3 Vocal cord imaging. (a) Positioning of the transducer. The transducer may be rotated in order to obtain optimal imaging. (b) Transverse ultrasound view of the hypoechoic vocal cords (V). The vocal cords are bound anteriorly by the cricoid cartilage (CC) and the thyroid gland (Th). (c) Longitudinal view of the vocal cords.
Scanning tips
Pitfalls
- The EDA is only an approximation of the cardiac preload.
- Positive pressure ventilation will constitute, in general, a burden on the impaired right ventricle (RV) because of the reduction of the preload and increase in RV afterload.
Tips to improve scanning
Hemodynamic management
Background
In order to assess for cardiovascular function, the heart rate, and invasive blood pressure monitoring, are often utilized. Clinical signs such as the capillary refill time and skin turgor are often unreliable. Indirect measurements such as urine output and serum lactate are also utilized, but are nonspecific. Functional echocardiography can be a valuable tool for assessing a rapidly changing hemodynamic status. It can characterize acute physiology, identify the exact nature of cardiovascular compromise, and guide therapeutic decisions. Functional echocardiography has become prevalent in neonatology, in particular, and can be utilized in order to assess cardiovascular physiology and function, and how they change over time. This involves the longitudinal assessment of myocardial function, systemic and pulmonary blood flow, intracardiac and extracardiac shunts, organ blood flow, and tissue perfusion. In neonates with a PDA, response to treatment may also be monitored (see Chapter 23). In addition, in those neonates and children with a high oxygen requirement, ultrasonography may be utilized to exclude the presence of structural heart disease, and monitor response to therapy. However, as with other applications of point-of-care ultrasonography, this is not meant to replace formal echocardiography performed by pediatric cardiologists. This bedside evaluation is meant to be an extension of the physical examination, and to be a functional evaluation over time.
The basic components of the hemodynamic assessment include cardiac function and fluid status. Goal-directed ultrasound may also be incorporated into the evaluation of undifferentiated hypotension in ICU patients. Lichtenstein introduced the FALLS protocol (Figure 24.4), which involves cardiac and lung ultrasonography in order to distinguish between the different types of shock: obstructive shock (tamponade, pulmonary embolism), cardiogenic shock, hypovolemic shock, and septic shock. As a result of findings found on ultrasonography, fluid therapy can be targeted, with the constant monitoring of lung artifacts. Moreover, point-of-care ultrasonography can facilitate the assessment, diagnosis, and optimization of interventions and follow the adequacy of interventions of these two components. Chapter 5 discusses the overall cardiac contractility. More in-depth measurements of the left ventricle and global systolic function include fraction shortening and ejection fraction, either by global visual assessment or by actual measurement. Additional parameters that are helpful in ICU settings include the Doppler assessment of trans-mitral flow that reflects the LV EDP and hence the left atrial pressure. This can be very useful in the assessment of different etiologic causes of pulmonary edema, and in titrating fluid and inotropes.
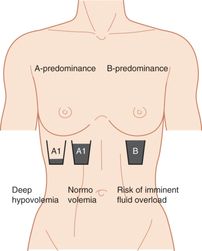
Figure 24.4 The FALLS protocol. Artwork created by Emily Evans. Based on: Lichtenstein, D.(2012) Fluid administration limited by lung sonography: the place of lung ultrasound in assessment of acute circulatory failure (the FALLS protocol). Expert Rev Resp Med 6(2): 155–62.
Technique
Point-of-care questions
Transducer selection and orientation
The assessment of the hemodynamic status in critically ill neonates and children includes the cardiac examination (Chapter 5) and the IVC evaluation (Chapter 7). A low-frequency, phased-array or micro-convex transducer with a small footprint should be utilized. In order to assess for cardiac function, all views of the cardiac assessment should be obtained: the subxiphoid, parasternal long-axis, parasternal short-axis, and apical four-chamber (Figures 5.5–5.8), or five-chamber views. In neonates, an additional suprasternal view should be obtained in order to assess for the presence of a PDA (Figure 23.14). For the evaluation of the IVC, the transducer should be oriented towards the patient’s right and the patient’s head in order to visualize the IVC in the transverse and longitudinal orientations (Figures 7.2, 7.3).
Ultrasound imaging
The hemodynamic assessment involves the global ventricular function (Chapter 5), and overall volume status (Chapter 7), as previously described. The combination of these two evaluations is essential in distinguishing between the different types of shock, and in monitoring the adequacy of therapy. This may be performed through four steps:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








