(1)
Aschaffenburg, Germany
1.1 Introduction
1.3 Epidemiology
1.5 Diagnostics
1.6 Classification
1.8 Therapy
1.8.3 Postoperative Treatment
1.9 Results
1.1 Introduction
The problem of tennis elbow (TE), also called epicondylitis lateralis humeri, epicondylalgia or epicondylopathy, has been known since 1834. Sir Charles Bell (ct. according to Narakas and Bonnard) described writing cramps in office employees and blamed muscle-tendon stress as the cause, due to the continuous use of a pen. Runge (1873), however, blamed a periostitis at the epicondyle extensor origins and under this aspect recommended to cut a deep scar by cauterisation. Morris (1882) detected a strain of the pronator teres muscle as cause of pain, triggered by fast and forced pronation movement of the forearm, necessary in backstroke swimming. Winckworth (1883) opposed to this opinion, remarking a strain of this muscle could hardly be responsible for all symptoms of TE.
Winckworth, however, found the pain originally resulted from a pressure damage of the deep radial branch at the supinator muscle, “where the nerve is pressed by diverse actions of the muscular fibres”. After this first hint at a possible neurological pathogenesis of TE, this opinion was for the first time supported by Bernhart (1896), who conceived this symptom as consequence of an occupational neuralgia. Finally Major (1883) localised the origin of TE at the annular radial ligament; at the end of the nineteenth century as many as three theories of tennis elbow pathogenesis existed, namely, the tendinogenous, neurogenous and arthrogenous theories, a solid base for an ongoing intense discussion on aetiology and pathogenesis of this disease. Up to now, agreement was only reached concerning the primary conservative treatment of TE.
Regarding terminology, it has to be remarked that the term “epicondylitis” is misleading and incorrect, as in the area mentioned no inflammatory changes were found in case of TE (Dunkow et al. 2004; Theis et al. 2004; Faro and Wolf 2007). Also the terms epicondylalgia, epicondylopathy and supinator syndrome are not satisfactory, as diverse extents of pain in TE and the corresponding trigger points are not surveyed at all. The term tennis elbow is much better, as two essential points of this disease are characterised, namely, the aetiologically important pressure stress of the deep radial branch by acute or chronic trauma. And the second point is taking into account the fact that among diverse professions and sports, tennis players show one of the highest incidences, up to 51 % (Kipai et al. 1986, cited according to Narakas and Bonnard 1993). In only 1–3 % of the population (Goguin and Rush 2003) and among those in just about 5–10 % of patients, tennis players are found (Theis et al. 2004); still the term TE is adequate.
1.2 Surgically Relevant Anatomy and Physiology
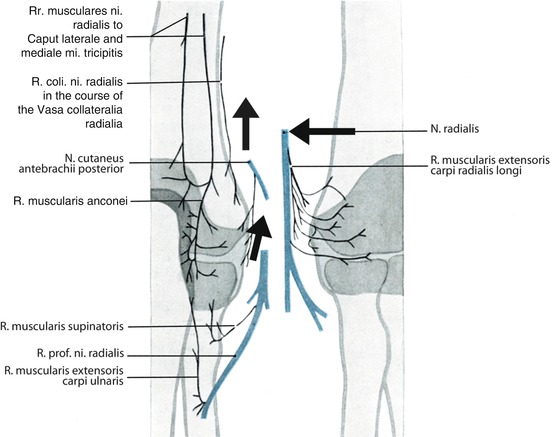
Anatomic and clinical examinations showed the maximum pain area of TE is exclusively innervated by fibres of the radial nerve (Figs. 1.1 and 1.2).
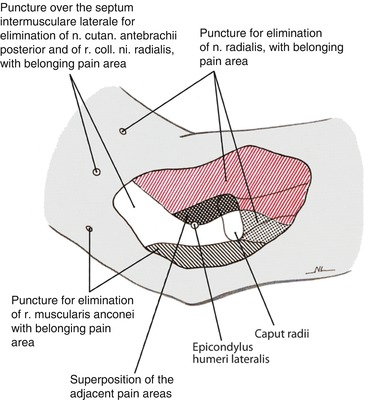
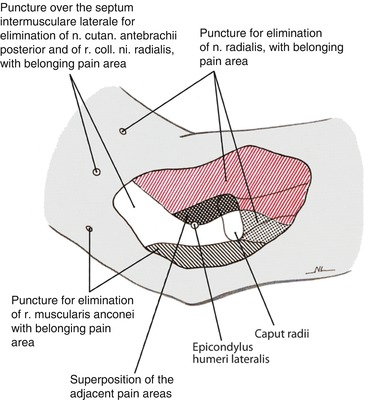
Fig. 1.1
Typical pain area of a severe lateral humeral epicondylitis. Aimed blockades can help distinguish individual pain areas and their innervations. (From Wilhelm (2000))
This is also true for coincident pain areas at the back of the hand with pain radiationto the basic finger joint (neuralgia of the posterior interosseous nerve; Wachsmuth and Wilhelm 1967; Fig. 1.3). The coincident pain areas above the radial styloid process and in the first interosseous space, however, are innervated by branches of the superficial radial nerve. This nerve is also responsible for the dorsolateral sensibility disorder found in 19 %.


Fig. 1.3
Synopsis of irritation syndrome of radial nerve. Punctured line: pain area in TE. Dotted line: hypaesthetic zone at the superficial branch of the radial nerve. Punctured area: pain area in radial styloiditis. Area of intermetacarpal pain also punctured. Pain areas in neuralgia of posterior interosseous nerve above the lunate bone and base of second and third intermetacarpal bone punctured. (From Wilhelm 1972)
The supraepicondyle and posterior pain areas, reaching to the outer side of the elbow, are innervated by branches of the subfascial collateral lateral radial nerve branch, running behind the lateral brachial intermuscular septum and the anconeus muscle branch. The last mentioned develops from a union of the triceps muscle lateral and medial head muscular branches (Fig. 1.2), the references of which originate from the radial nerve at the upper arm, proximal to the radial nerve hiatus. The posterior antebrachii cutaneous nerve with a small branch innervates the epicondyle and the ERCB origin. Irritations of the radial nerve and its references in the region of the upper arm, the thoracic outlet and the intervertebral foramina C5–7 are responsible for pain manifestation in this area.
These three nerves are not involved in the original compression mechanism of the deep radial branch, but they may hint at the just mentioned areas of disturbance, possibly causing a “double nerve lesion”.
Distally, at the extension side, an essential recurrent branch of the supinator muscle branch is found, being responsible for pain transfer in epicondyle direction. Digital pressure over the supinator gap serves as a proof.
On the flexion side, the final muscular branch fibres of the long radial carpi extensor (ECRL) and the short radial carpi extensor (ECRB) innervate the humeroradial joint area (Fig. 1.2, right side). One of these branches (the third from above) does innervate not only the origin of ECRB tendon, where it spreads extensively, but also the epicondyle and the lateral collateral ligament. Distally a recurrent articular branch of the supinator muscle branch joins, the function of which can also be taken over by a very strong branch of the radial nerve (Fig.1.2 right side, last branch from above).
The anterior pain area extends over the epicondyle, the bulging of the radial extensors and over the course of the radial nerve, especially at the height of the humeral capitulum, the radial head and the supinator gap.
1.3 Epidemiology
The incidence of tennis elbow (TE) is hard to estimate, as many patients with minor complaints do not consult a physician. Generally the incidence is estimated to be 1–3 or 3–4 %, the dominant arm being affected in 90 %. The ratio male/female is 5:1. Surgical intervention due to therapy resistance is necessary in 3–8 % (Demmer and Rettig 1982). Average age of patients is between 35 and 55 years.
1.4 Aetiology and Pathogenesis
Aetiology and pathogenesis of TE are discussed controversially as of today. Since the beginning of the nineteenth century, a diversity of surgical techniques has been developed, based on different concepts of pathogenesis. The most important surgical methods are summarised in Table 1.1.
Table 1.1
Surgical treatment of resistant TE – survey of literature
Author | Surgical method |
|---|---|
Frank (1910) | Epicondylectomy |
Fischer (1923) | Excision of subcutaneous tissue above epicondyle |
Hohmann (1927) | Notching of ECRB tendon |
Tavernier (1946) | Mononeurotomy of radial nerve lateral collateral branch |
Bosworth (1955) | Partial resection of annular radial ligament |
Kaplan (1959) | Partial anterior denervation |
Garden (1961) | Distal lengthening of ECRB tendon |
Wilhelm and Gieseler (1962) | Complete denervation |
Goldie (1964) | Excision of subtendon pathologic tissue |
Capener (1966) | Decompression of deep radial nerve branch |
Roles and Maudsley (1972) | Decompression of radial nerve (radial tunnel) |
Boyd and McLeod (1973) | Epicondylectomy and partial excision of annular radial ligament |
Wilhelm (1977) | Decompression of radial nerve (upper arm) |
Nirschl and Pettrone (1979) | ¾ resection of ECRB tendon, release |
van der Beken and Joveneau (1983) | Z-graft at ECRB and EDC |
Narakas (1987) | Lengthening of ECRB and decompression of radial nerve |
Wilhelm (1989) | Denervation and direct decompression of radial nerve |
Denervation and indirect decompression of radial nerve (method of choice since 1991) | |
Almquist et al. (1998) | Resection of ECRB and EDC at epicondyle–anconeus graft |
Rayan et al. (2001) | V-Y graft of ECRB and EDC origins |
Double nerve lesion | |
Wilhelm (1996) | Transaxillar decompression of nerve-vessel bundle in TOS and Sudeck’s dystrophy |
Decompression of radial nerve at upper arm (PRKS) | |
The most prominent supposition is based on functional stress together with micro-trauma and degenerative changes of tendon tissue. According to Bosworth there is an intraarticular cause of TE. Turning of the unevenly formed radial head—sometimes combined with an impingement of a synovial fold—leads to typical complaints. Recently a neurogenous genesis based on the work of Wilhelm has been discussed frequently.
The following facts and conclusions point towards a neurogenous aetiology:
1.
Anamnestic details concerning the cause of development: sudden hyperactivity, caused by strong pronation in tennis, for example, and chronic strain of pronators and supinators as well as radial extensors, especially against resistance.
4.
Anatomic findings can be proved by aimed nerve blocks, thus analysing the corresponding pain area (Fig. 1.1).
5.
A supraepicondyle and posterior pain area, little regarded up to now, is found in 31 %, innervated by the collateral lateral branch of the radial nerve and the muscular anconeus branch, both already originating from the upper arm radial nerve (Fig. 1.2).
6.
The epicondyle peak and the originating tendon of ECRB are additionally innervated by fibres of the posterior antebrachii cutaneous nerve, also originating from the upper arm (Fig. 1.2). This proves that in TE also pain radiation from farther proximal areas of radial nerve disturbance can be expected.
7.
By checking the trigger points of the radial nerve at the level of the radial head in 67.8 % and above the supinator gap in 77 %, pain radiation can be triggered in the direction of the epicondyle peak and the radial nerve proximally and distally (Fig. 1.7). Analogous symptoms can be triggered by the D3 test.
8.
9.
Coincident sensibility disorders are found at the superficial branch of the radial nerve in 19 %, as well as a so-called radial styloiditis in 16.7 % (Fig. 1.3).
10.
The compressive effect of the supinator arcade on the deep radial branch can be shown by a pronation and supination test, which in 86 and 93 % absolutely tops the D3 test in 74 % (Werner 1979).
11.
Normally the supinator arcade is stretched in passive pronation, leading to a clearly visible pressure stress of the deep radial branch (Fig. 1.4) at about 40–50 mmHg (Werner 1979). This pressure suffices to stop the intraneural venous blood flow as well as the axonal flow. Due to a coupling effect of the supinator tendon with the ECRB a tension stress of the originating tendon of this muscle, which thus shows a stretched course. In supination, however, the arcade and all remaining parts of the supinator muscle relax completely, as well as the ECRB tendon, then running dorsally in a more bow-shaped course (Fig. 1.4). Intraoperatively the diversity of strain stress of ERCB by the supinator arcade in pronation and supination of the forearm can be demonstrated well, slinging the additional origin of the supinator muscle proximally with a rubber rein, straining the ECRB tendon in opposite direction, where the tension stress by the rein has to remain below that of the supinator muscle (Fig. 1.4).
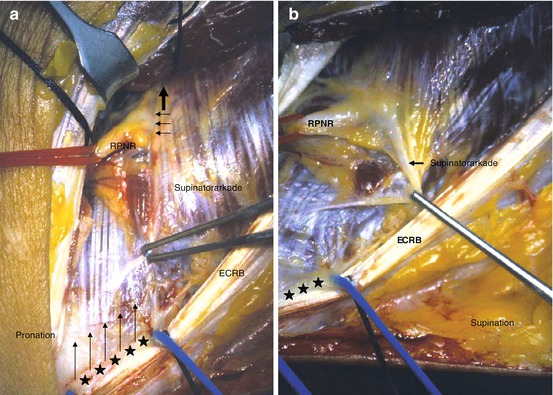
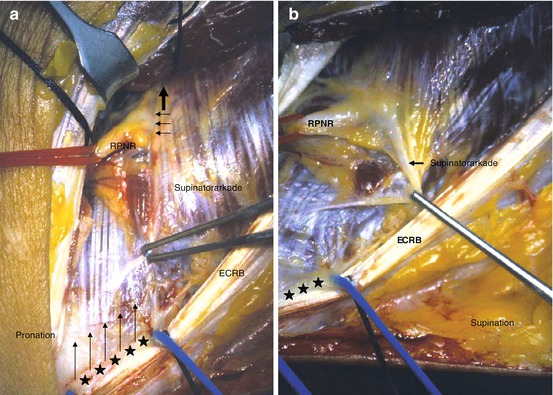
Fig. 1.4
Intraoperative presentation of supinator arcade. (a) In passive pronation: significant tension of the arcade and the strong superficial fascia of the supinator muscle (thick arrow above) with compression of the deep radial branch (RPNR) and the crossing vessels (“Henry’s leash”); traction stress of ERCB tendon (thin arrows) by additional origin of supinator muscle from their tendon, marked by stars and rubber rein. (b) Complete relaxation of supinator muscle arcade and ERCB tendon in passive supination; no pressure stress on radial nerve
12.
In a continuous series of 164 denervations (1980–2009) in 96.9 %, fibrous arcades of diverse strengths were found. In two cases, the arcade was situated below the deep radial branch; in three cases, it was not developed at all.
13.
After direct decompression of the radial nerve (1980–1990, 87 cases), in 85 % diverse pressure damages were found. In 15 % only a disturbance of the subepineural blood flow was found (Table 1.2). But even this minor change results in an impairment of intraneural flow. Severe tension stress of the arcade can even result in major pressure damage, resulting in flattening of the nerve diameter and a bow-shaped change in the course of the nerve. Only after resection of the arcade you see the exact extent of the damage. The nervous strands stripped from the epineurium remain next to each other, but again they take a normal course (Fig. 1.5).
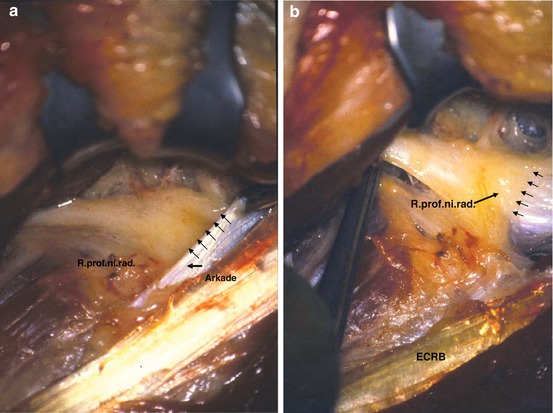
Table 1.2
Intraoperative findings in decompression of deep branch of radial nerve – results in group B (N op = 87)
1. Frohse–Fränkel arcade | |
Delicate | |
Structure | 23 (26.4 %) |
Strong | 64 (73.6 %) |
2. Pressure damage of deep branch of radial nerve | |
Flattening | 59 (67.8 %) |
Indentation | 8 (9.2 %) |
Constriction ring | 7 (8.0 %) |
Pseudoneuroma | 26 (30.0 %) |
Lack of subepineural blood flow | 13 (15.0 %) |
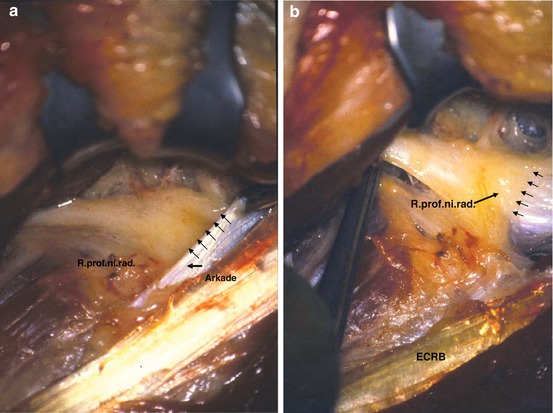
Fig. 1.5
Deep branch of radial nerve at the entrance of supinator channel (thick arrow). (a) Triple broadening of nerve diameter at the arcade under tension with thickening of epineurium (thin arrows). (b) After resection of arcade nerve fascicles lie together; the thickened epineurium has been pushed back (thin arrows)
14.
Two years later, these pressure damages were confirmed via electronic diagnostics; in 84 % (Kupfer et al. 1998) pathological reactions were found in EMG examinations of the forearm in neutral position as well as in passive pronation and supination (Table 1.3).
Table 1.3
Development of pain level in D3 test in passive pronation and supination N; Pat. = 46 (08/04–12/07)
Pronation – EJ extended | Supination – EJ extended | Supination – EJ flexed | ||||||
|---|---|---|---|---|---|---|---|---|
n 1 | % | n 2 | % | N 3 | % | |||
6× | +++ | 13.8 | 20× | – | 43.5 | 42× | – | 91.3 |
13× | ++ | 27.6 | 12× | (+) | 26.0 | 4× | ((+)) | 8.7 |
24× | + | 51.7 | 14× | ((+)) | 30.5 | |||
3× | (+) | 6.9 | ||||||
15.
The immediate pain reaction in the region of origin of the common forearm extensors, triggered via D3 test, is localised in the area of the common origin of the extensor tendons by the primary description of Roles and Maudsley (1972) and is interpreted as stress of the ECRB tendon. This pain reaction can be turned off by blocking the radial nerve in the cubital fossa in 90 % (Ishii and Nakashita 1985). This surprising result negates the tendinogenous origin of this syndrome, as in this case after a blockade, still pain conduction, primarily via fibres of the posterior antebrachii cutaneous nerve would have been possible, as these innervate the lateral epicondyle and the region of origin of the ECRB tendon (Wilhelm 1999).
16.
Diverse effects of forearm positions on the tension condition of the arcade also explain why crude strength in TE is massively reduced due to pain in pronation, at the same time being much better in supination due to a reduction of the extent of pain (Fig. 1.6). In severe pain, however, crude strength is reduced in both positions; in some cases, it cannot be measured at all. If, preoperatively, the D3 test is negative in pronation and supination, this calls for a non–existent coupling mechanism of supinator muscle and ECRB tendon.
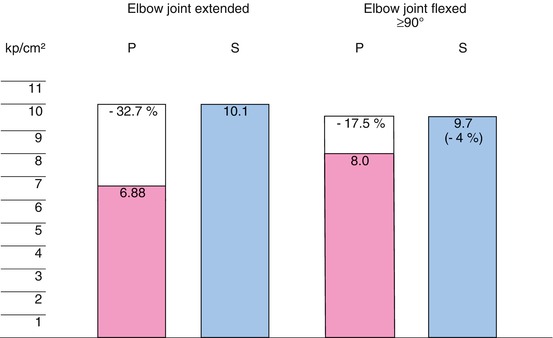
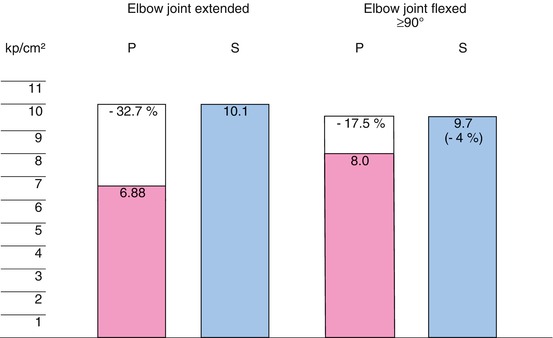
Fig. 1.6
Behaviour of crude strength in pronation (P) and in supination (S) (N p = 28; 01/2007–05/2009)
17.
The compressive effect of the ligamentary arcade on the deep radial branch, already shown in pronation, increases in this position as soon as the tendon of the ECRB is used and stressed. The cause of this phenomenon is found in an additional origin of the supinator muscle from the inner side of the tendon of origin of the ECRB (Fig. 1.7, asterisk) which has not yet been mentioned in anatomic literature. Supinator muscle and ECRB are functionally connected by the origin. Since 1991 this effect was found in 74 (91.1 %) out of 77 cases, finally explaining not only the pain reaction in D3 test but also the pathogenic significance of radial extensor overexertion, especially the ECRB. Additionally it has to be remarked that Heyse-Moore (1984) mentioned the origins of the supinator muscle and the tendon of origin of the ECRB have melted, and thus the supinator muscle has a higher tension on the epicondyle; this tension could be diminished by separating the superficial head of this muscle. Quite the contrary is the case, however! The increased tension of the ECRB tendon, triggered as a reflex in the D3 test, leads to an increase of tension in the supinator arcade in passive pronation, due to the coupling mechanism described. Clinically this can be proven by the D3 test.
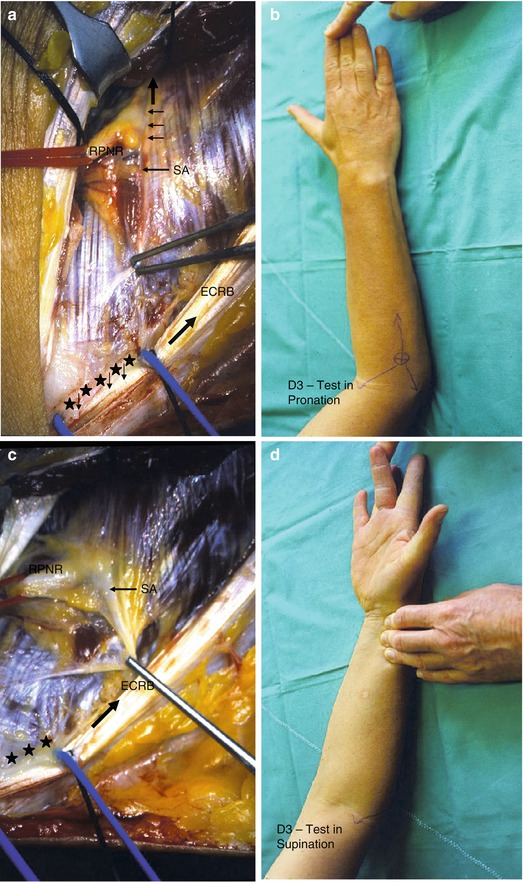
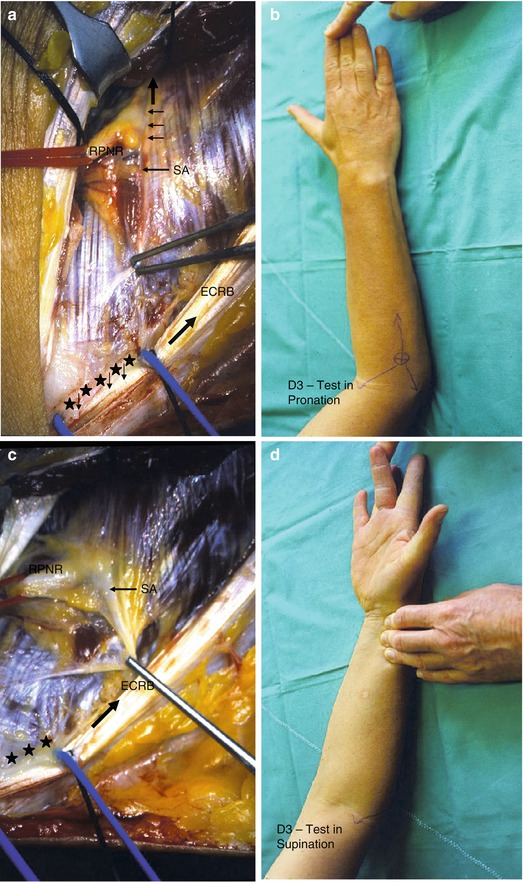
Fig. 1.7
D3-test according to Roles and Maudsley. (a) D3-test is performed in passive pronation of the lower arm: In D3-test there is an extensive reflectory tension of the ECRB-tendon, wherby normal tension-stress is slightly reduced by the supinator muscle. Tendon tension is so intense, however, that the coupling mechanism even results in an additional stress of the supinator-arcade, leading to an immediate pain reaction. Deep radial branch and crossing vessels are already compressed by the supinator-arcade in this position; whereas the ECRB-tendon suffers from a heightened tension-stress by the coupling mechanism, described. (b) D3-test in pronation: In this case we can find a typical radiation of pain to the lateral epicondyle and in proximal and distal direction of the radial nerve, s. arrow; supinator cleft: s. ring with asterisk. (c) Position in passive supination: Due to the slackening of the supinator muscle and its arcarde the effect of the above mentioned coupling mechanism does not work in supination. (d) D3-test in passive supination: In this position supinator muscle and its arcade are completely relaxed, whereby the pain is reduced clearly
18.
D3 test is negative after denervation with indirect decompression of the radial nerve, as in this surgical procedure a disconnection of the common origins of supinator and ECRB tendon has to be performed in order to prepare and cut the anterolateral portion of origin of the supinator muscle whereby the essential pain conducting structure of the recurrent branch of the R. muscularis supinatoris is cut simultaneously (Fig. 1.7).
19.
D3 test finally turns negative in passive supination of the forearm, in 43.5 % at simultaneous extension of the elbow joint and in 91.3 % in flexion. Minor pain remains only in 8.7 % (Table 1.3)
20.
Reason being that an additional strength conduction via ECRB tendon in forearm supination cannot lead to results though there is a coupling mechanism, as in this position the arcade is completely relaxed (Fig. 1.4).
21.
TE has a special meaning in a so-called double nerve lesion. Thus in PRKS according to Wilhelm (1999), surgical decompression of the radial nerve at the upper arm showed excellent and good results in 9 (69 %) out of 13 cases (Table 1.4). Also surgical treatment of an overlying TOS as well as Sudeck’s dystrophy in 65 (76 %) out of 86 cases (Table 1.5) and in 7 (70 %) out of 10 cases showed significant improvement of classical TE symptoms (Table 5.3; Wilhelm 1996). The intervertebral foramina C5–C7 can also cause a double nerve lesion.
Table 1.4
Tennis elbow in proximal compression of radial nerve (PRKS) results after decompression (1969–1988: N p = 13 − N op = 13)
Preoperative findings | n | Postoperative results | |
|---|---|---|---|
Excellent | No change | ||
Pain regions | |||
Epicondyle region | 13 | 9 | 2 (+2) |
Neuralgia of posterior interosseous nerve | 5 | 3 | 1 (+1) |
Radial styloiditis | 4 | 3 | 0 (+1) |
Sensibility disorders (superficial branch of radial nerve) | 19
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| ||