The Child Athlete: Preparticipation Screening and Common Issues
Keith Reinsdorf MD
Dennis Cardone DO
INTRODUCTION
The 21st century athlete encounters a vast array of options and information unavailable even a few short years ago. Knowledge in the areas of strength training, sports nutrition, and sports psychology is increasing. Common medical conditions, clearance issues, the use of anabolic steroids, the role of weather conditions in training, eating disorders, and problems unique to the female athlete are addressed in an effort to promote provider awareness and ultimately the healthy growth and development of the child athlete.
The child or adolescent intent on participating in athletics should undergo a preparticipation history and physical evaluation. This will enable the provider to determine the patient’s general health status and to screen for any conditions that may limit participation or put the patient at risk for injury or sudden death. This encounter also establishes a relationship that will help address any problems should they arise over the course of athletic involvement. The examination of patients younger than 18 years should include parental input, because often children’s versions of their history will differ from that provided by parents (Bratton & Agerter, 1995). Featured components of the preparticipation evaluation (PPE) include the patient’s cardiopulmonary and injury histories in addition to a comprehensive orthopedic evaluation and assessment of the child’s growth and development (Display 14-1) (Smith, Kovan, Rich, & Tanner, 1998). This evaluation is not a well child visit, nor is it meant to be exclusive of the components that constitute a general medical history and physical examination. The aim of providers is to assess a patient’s ability to participate in a sport with only limited risk.
DISPLAY 14–1 • Standard Components of the Preparticipation Evaluation
Height
Weight
Eyes
Visual acuity (Snellen chart)
Differences in pupil size
Oral cavity
Ears
Nose
Lungs
Cardiovascular system
Blood pressure
Pulses (radial, femoral)
Heart (rate, rhythm, murmurs)
Abdomen
Masses
Tenderness
Organomegaly
Genitalia (males only)
Single or undescended testicle
Testicular mass
Hernia
Skin
Rashes
Lesions
Musculoskeletal system
Contour, range of motion, stability, and symmetry of neck, back, shoulder/arm, elbow/forearm, wrist/hand, hip/thigh, knee, leg/ankle, foot
Reprinted with permission from Smith, D. S., Kovan, J., Rich, B., & Tanner, S. (1998). The physician and sports medicine (2nd ed.). Minneapolis, MN: McGraw-Hill Healthcare.
• Clinical Pearl
The ultimate goal is not to screen the patient with the idea of finding cause to exclude the individual from play, but rather to suggest more appropriate sports if indicated by the individual’s presentation (Andrews, 1997).
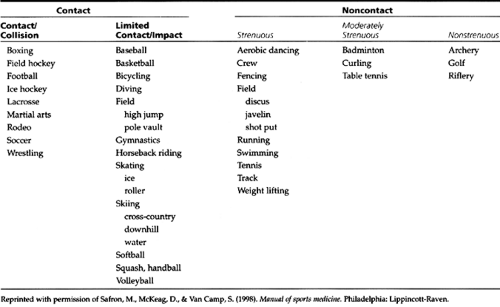
Most patients will derive numerous benefits from athletics; thus, it is part of the provider’s role to help the patient remain active. Table 14-1 provides a classification of sports according to their degree of contact and activity intensity. Fortunately, only about 1% of PPEs result in denied clearance. Roughly 10% of those visits require further evaluation (Bratton & Agerter, 1995).
EPIDEMIOLOGY
While many factors affect a patient’s ability to participate in athletics, certain common conditions require familiarity from primary care providers, because they often lead to questions regarding clearance to play. In addition, suggested guidelines exist for many conditions in terms of athletic participation (Appendix 14-1). Regardless of the illness, the provider must view each patient individually, including whenever possible parents, coaches, and athletic trainers who will be monitoring the child’s well-being while he or she participates in the chosen sport.
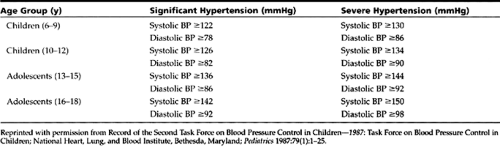
An increase in physical activity leads to an increased demand on the cardiopulmonary system and can be associated with potential limitations. Hypertrophic cardiomyopathy, with a prevalence of 0.1% to 0.2%, is the leading cause of sudden cardiac death in athletes younger than 30 years and requires patients to restrict themselves to low-intensity athletics (Safran, McKeag, & Van Camp, 1998). Hypertension, as diagnosed by three separate elevated readings on separate occasions, varies according to criteria for each age group and is relatively uncommon in children. This condition generally results in limitation only if severe or associated with extensive secondary illness (Table 14-2).
Valvular disease and arrhythmias, while not uncommon, generally do not result in significant limitation unless they are seen together or cause symptoms. Mitral valve prolapse, present in about 5% of the population, can have associated exercise limitations, depending on family history, associated symptoms, and degree of regurgitance.
Individuals with Marfan syndrome should not participate in contact or collision sports but are otherwise cleared if they do not have aortic root dilation, mitral reguritation, or a family history of early sudden death. Monitoring of the aortic root dimensions every 6 months is recommended.
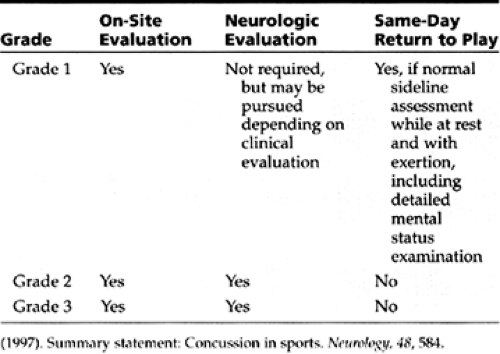
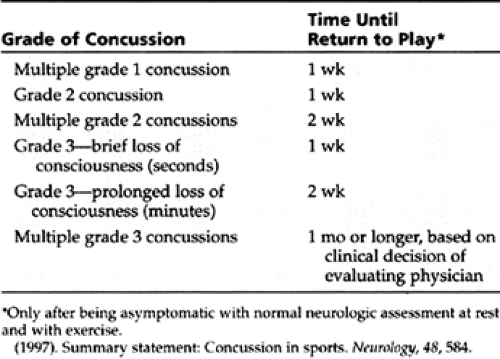
Patients with seizure disorders are allowed to participate in all sports as long as medication well controls their condition. High-risk sports, such as skiing, diving, swimming, auto racing, and high bar gymnastics, most likely should involve consultation with a neurologist. Athletes who suffer a concussion, a transient loss of consciousness with amnesia, are treated individually. Table 14-3 and Table 14-4 discuss the initial management of concussion and guidelines for when to return to play (Quality Standards Subcommittee, 1997). Two certainties in concussion management are that patients with prolonged symptoms (ie, longer than 1 or 2 weeks) necessitate a workup and that all patients must be withheld from activity while they are symptomatic to prevent potentially fatal “second impact syndrome.”
Exercise-induced bronchospasm, ranging in prevalence from 10% to 40% of the general population, is an extremely common problem. The use of peak flow meters and knowledge of exacerbating factors are critical to management. Diabetes mellitus, unless poorly controlled, is not a contraindication to exercise. Patients who have had the disease for at least 10 years, however, warrant close evaluation and follow-up, because they are more likely to experience complications (Fields & Fricker, 1997). Sickle
cell trait, which has been associated with exertional rhabdomyolysis and heat illness, also is not a contraindication to athletic participation.
cell trait, which has been associated with exertional rhabdomyolysis and heat illness, also is not a contraindication to athletic participation.
Acute viral illness of the upper respiratory tract is perhaps the most common condition seen by the primary care provider, with the average child affected as often as 10 to 12 times per year. Patients often are able to continue to participate unless fever, tachycardia, or other systemic signs are present. Patients with fever must be withheld from participation due to the increased likelihood of heat illness and the possibility of a potentially fatal myocarditis.
Infectious mononucleosis, with an attack rate of approximately 3% to 5% (Richmond & Shahady, 1996) of adolescents per year, requires that patients be restricted from activity for at least 3 weeks and 4 weeks if the patient is involved in a contact sport. This allows for resolution of any splenomegaly, which examination may not always detect. Patients with human immunodeficiency virus (HIV) must be viewed individually in terms of their general health and sport of interest. HIV alone is not a contraindication for any sport; however, sports such as boxing, football, soccer, wrestling, and rugby, where risk of exposure is high, should be viewed with more caution.
Common conditions in children and adolescents, such as Osgood-Schlatter disease and Sever’s disease, are viewed in the same manner as acute sprains or strains. That is, clearance should be withheld if signs of inflammation, decreased range of motion, instability, or strength less than 85% relative to the unaffected side are present (Smith et al., 1998). Stress and avulsion fractures are more commonly seen in children than in adults. It is important to note that knee pain in children often is due to hip disease. A thorough examination can visually differentiate the etiology of symptoms.
HISTORY AND PHYSICAL EXAMINATION: THE PREPARTICIPATION EVALUATION
The primary goal of the PPE is to help promote safe participation in an activity that is enjoyable and suitable to the patient so that the patient can reap the many benefits that athletic involvement offers. The PPE should occur yearly in individuals younger than 18 years due to the relatively rapid and significant physical changes that occur during childhood and adolescence. Also, the evaluation should occur 1 month before the sport season starts so that any issues that arise can be addressed without the athlete having to miss much time from the sport. While one of the objectives is to determine general health, the PPE is not a substitute for a well child examination or vice versa. The PPE and the well child visit can be combined in one visit, however, if proper time is allotted.
The PPE is perhaps best completed in the primary care provider’s office to foster confidentiality and disclosure of any private concerns. This can help maintain continuity of a therapeutic provider–patient relationship. Hopefully, the provider will be familiar with current PPE recommendations and clearance issues. In individuals younger than 18 years, parental input is encouraged regarding history taking, but certain sensitive issues may cause problems regarding confidentiality. Most states require that each child undergo a PPE prior to each school year. This results in a large number of individuals needing to be evaluated at the same time. Station-based examinations are suitable for mass screening and often occur at local high schools and middle schools before the school year begins.
One unfortunate disadvantage of station-based examinations is a relative loss of privacy and possible nondisclosure of more sensitive concerns.
States and governing bodies (the NCAA and United States Olympic Committee) have rules and regulations concerning the frequency of PPEs and allowable pharmaceuticals of which the provider needs to be aware to avoid inadvertently disqualifying an athlete. Please see Appendix 14-2, which has been endorsed by the American Academy of Family Physicians (AAFP), the American Academy of Pediatrics (AAP), the American Medical Society of Sports Medicine, the American Orthopedic Society for Sports Medicine, and the American Osteopathic Academy of Sports Medicine as a comprehensive preparticipation screening evaluation (Smith et al., 1998). Many major universities and athletic institutions also have adopted this sample for the screening of their athletes.
It is important to recognize that routine history and physical examination will never detect certain life-threatening conditions, such as idiopathic hypertrophic subaortic stenosis,
prolonged QT syndrome, or anomalous coronary artery syndrome. Only further investigation, such as with a 2-D echocardiogram or electrocardiogram (ECG), may identify these conditions.
prolonged QT syndrome, or anomalous coronary artery syndrome. Only further investigation, such as with a 2-D echocardiogram or electrocardiogram (ECG), may identify these conditions.
History
At least 70% of potential problems are uncovered during the history, which is designed to screen for conditions that might lead to injury or death due to sports participation (Bratton & Agerter, 1995). The history must be reviewed with the child’s parents to help prevent the omission of potentially significant information. The history consists mainly of questions pertaining to the cardiopulmonary, musculoskeletal, and neurologic systems. Also, questions regarding history of heat illness; drug, medication, or supplement usage; and chronic or congenital medical conditions are included. Appendix 14-2 provides a suggested history in further detail. This is adapted from the PPE monograph put forth by Smith et al. in 1998.
Physical Examination
The physical examination is similar to a general examination, with attention paid to blood pressure and the cardiopulmonary and musculoskeletal systems in particular. It is suggested that children with mild to moderate elevations of blood pressure be rechecked and, if cleared, followed up during the season. Elevations in blood pressure can be a sign of drug and supplement usage, especially with products that enhance the sympathic nervous system (weight loss products).
The cardiac examination focuses on the detection of murmurs and irregular rhythms. All diastolic murmurs are abnormal, and the systolic murmur of IHSS increases in intensity with maneuvers that decrease venous return (eg, standing, Valsalva’s maneuver). Irregular heartbeats warrant ECG evaluation, and the provider must ask about recent viral infections due to the possibility of a potentially fatal myocarditis.
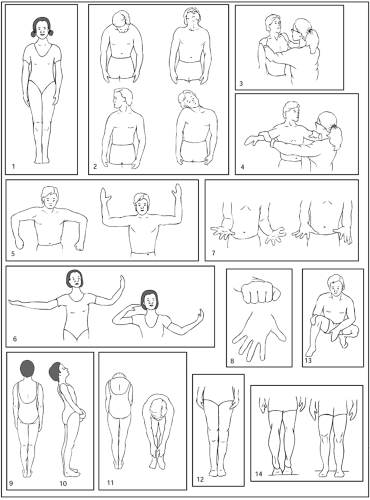
A thorough musculoskeletal examination involves the 14-step screening examination (Fig. 14-1), which takes no longer than 2 minutes to administer. It also should include sports-specific evaluations of the knee for football and soccer players, the shoulder for swimmers and baseball pitchers, and the ankle, which is heavily involved in almost all sports. Examining the ears of swimmers for chronic otitis externa and the skin of wrestlers for rashes (ie, herpes gladiatorum) is helpful not only to treat the patient, but also to promote disease prevention. No evidence supports obtaining routine blood or urine specimens for analysis during the PPE (Smith et al., 1998).
ANTICIPATORY GUIDANCE
Common Questions
The following are common questions asked of providers:
What aspect of participation should the coach emphasize?
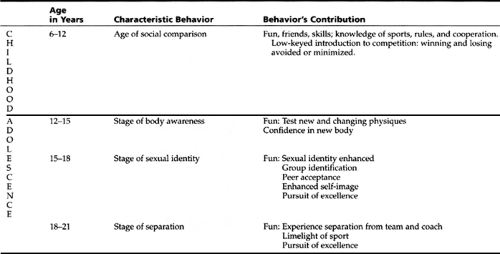
While teaching proper techniques and strategy is important, the coach should emphasize having fun and learning to function as a member of a team. Admittedly, winning does contribute to the enjoyment; however, it must remain a secondary goal for young athletes to foster an environment for children and their families to grow together and develop positive self-esteem. Table 14-5 and Display 14-2 refer to the behavioral goals of sports participation in childhood and adolescence (Mellion, 1999; Smith & Stanitski, 1987).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree