Support from family and friends
Three quarters of patients receive care at home from informal carers in the last months of life. Patients without cancer are less likely than those with cancer to have someone to care for them, reflecting their older average age at death. For people with cancer, care may be needed for weeks or months; for conditions other than cancer it may be needed for years.
Informal carers often have high levels of anxiety and depression. Lack of sleep and fatigue are common problems, and the carer’s own health may suffer. Psychological morbidity while caring may be related to subsequent poor bereavement outcomes.
The degree of psychological distress is related to the amount of care patients need; the impact on carers’ lives; how well the family functions under stress; the availability of social support for the carer; the carer’s health status and their coping styles. Providing support for depressed, demented, or delirious patients is particularly difficult.
Carers are individuals and will respond in different ways to caregiving; there is no substitute for asking them directly about their experiences, fears, and needs. Not all the consequences of caregiving are negative: many carers report getting pleasure from being able to help someone they love. They—and the patient—will resent suggestions that the experience is wholly negative or, indeed, negative at all.
Fewer people die at home than would like to do so. Carers’ views on home deaths are largely unknown. One reason for admissions is that informal caregivers are unable to continue because of deteriorations in their own health, fatigue and psychological distress, patient’s increasing level of dependency, lack of confidence in their caring abilities, and the failure of health and social services to deliver appropriate care.
It is important to provide good support to informal caregivers to protect them from adverse health consequences both before and after bereavement, and to enable patients to stay at home for as long as they want. Health professionals should address carers’ needs for information, practical support and advice, and psychosocial support.
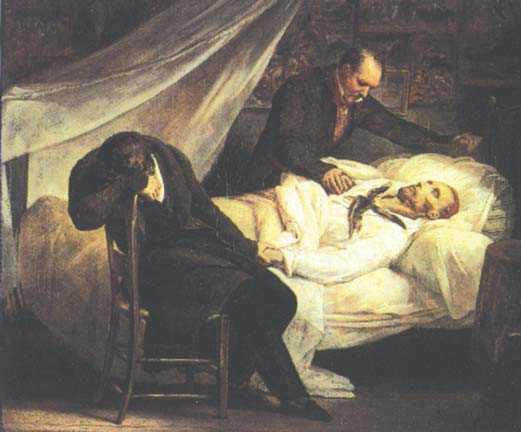
“The death of Theodore Gericault (1791–1824), with his friends Colonel Bro de Comeres and the painter” by Ary Scheffer (1795–1858). Until the start of the 20th century, most people died at home while being cared for by family and friends
- More patients want to die at home than currently do so
- Informal carers are vital to the support of patients at home
- Many informal carers are elderly and have their own health needs
- A third of caregivers provide all the informal care themselves
- Carers provide care without specialist knowledge and training, 24 hours a day, seven days a week
- Fatigue, anxiety, and depression are common among informal carers
- The patient’s diagnosis
- Causes, importance, and management of symptoms
- How to care for the patient
- Likely prognosis and how the patient may die
- Sudden changes in patient’s condition, particularly those which may signal that death is approaching
- What services are available and how to access them (including in emergencies)
- Practical and domestic
- Respite
- Night sitters
- Psychosocial
- Financial
- Spiritual
Information
Information about the illness, its likely course, and what to expect as the patient deteriorates enables patients and carers to make informed decisions and reduces anxiety. It is not good practice to inform only the relatives about the patient’s disease, its management, and prognosis. Exceptional circumstances may arise when patients (not relatives) clearly indicate they do not wish to discuss their illness or when patients are unable to understand the necessary information. Informing only relatives can lead to mistrust and impaired communication between patients and their relatives at a time when mutual support is most needed. Patients may choose to consult with their doctor alone, but joint consultations with both the patient and relatives avoid the problems that can arise when one or other party is informed first. Many carers report not having received all the information they wanted about the patient’s illness.
Practical support and advice
Most informal carers benefit from practical instructions on how to care for patients—for example, how to lift them safely. District and palliative care nurses have an important role here, as well as in providing information on and arranging financial benefits, practical support in the home, and respite and overnight care. Availability of these resources varies widely across the UK and other countries, which places an additional burden on carers.
Psychosocial support
Mild psychological distress usually responds to emotional support from frontline health workers with effective communication skills. This involves listening to carers’ concerns and fears, explaining physical and psychological symptoms, challenging false beliefs about death and dying, and helping carers reframe their experiences more positively. More severe psychological distress may benefit from specialist psychological assessment and treatment.
Healthcare professionals
Many different health professionals care for patients in their last year of life—in the community, in hospitals, and in hospices and other institutions. Some health professionals devote the whole of their working time to palliative care, while for many others it forms only a small part of their formal workload.
Psychiatric morbidity and burnout
Working in palliative care is widely believed to barrage staff with suffering and tragedy. The stress associated with caring for dying people, however, may be counterbalanced by the satisfaction of dealing well with patients and relatives. Psychiatric morbidity among palliative physicians and palliative care nurses is lower than among many other healthcare professionals.
Job stress and satisfaction
Palliative physicians and nurses report similar sources of stress as other healthcare professionals, with overload and its effect on home life being predominant. Poor management, resource limitations, and issues around care of the patients are also major sources of job stress. Palliative care nurses find difficulties in their relationships with other healthcare professionals a particular source of stress, often because their roles are poorly understood and sometimes poorly defined. Good relationships can, however, be a source of job satisfaction. Death and dying do not seem to be a major source of job stress.
Palliative physicians have significantly higher levels of job satisfaction compared with consultants working in other specialties, and palliative care nurses have significantly higher levels than most other nurses. Good relationships with patients, relatives, and staff, controlling pain and other symptoms, and improving patients’ quality of life are common sources of satisfaction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








