Chapter 6 The approach to the patient with chest pain, dyspnoea or haemoptysis
Chest pain, dyspnoea and haemoptysis are common and important symptoms which bring patients to the emergency department. The role of the emergency medical team is to rapidly identify high risk patients, commence resuscitation if necessary, arrive at an accurate diagnosis, initiate appropriate therapies and arrange appropriate disposition. Some therapies are extremely time-dependent (e.g. reperfusion therapy for myocardial infarction) and good outcomes depend on early recognition of these seriously ill patients. However, the clinician must be aware of the costs associated with inappropriate admissions and investigations.
CHEST PAIN
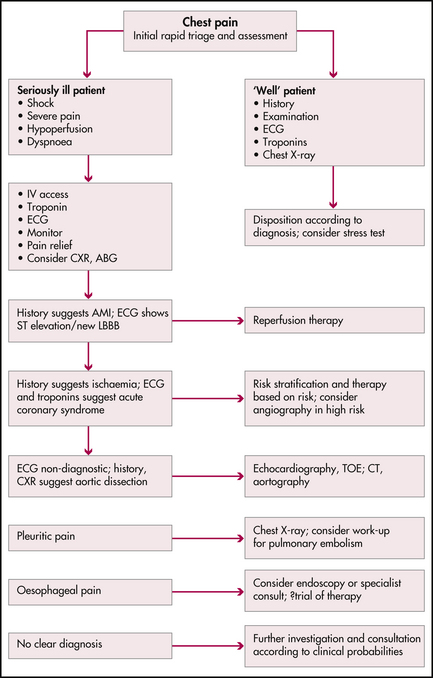
The general public is increasingly aware of the importance of chest pain and the need for early presentation with this symptom. In American emergency departments, up to 7% of all presentations are for chest pain, prompting changes in the organisation of emergency departments so that many high volume departments have specialised chest pain units where patients with this symptom are rapidly triaged and treated according to defined protocols. While there are many causes of chest pain, clinicians should be aware of disorders which are potentially life threatening (Figure 6.1). Before any chest pain patient is discharged, each of these diagnoses should at least be considered.
Myocardial ischaemia
(See also Chapter 7, ‘Acute coronary syndromes’.)
History
Take time to question the patient, using non-leading questions, to clarify the nature of the patient’s pain. The pain of myocardial ischaemia is classically a deep visceral pain felt in the anterior chest but not localised to any part of the chest. Patients may describe heaviness, constriction, a sensation like a heavy weight or a dull ache. Pain usually comes on gradually, reaching a peak over a few minutes, and lasts at least a few minutes. Patients prefer to lie still and the pain is not exacerbated by the respiratory cycle, posture or food intake. Classical radiation patterns include spread to the neck, jaw or arms. Pain radiating to the left arm is more common than to the right. Heaviness (rather than pain) in both arms is also very suggestive. Autonomic accompaniments such as sweating, nausea and anxiety are also concerning. While the pain of myocardial ischaemia may be severe, the severity of the pain is not consistently related to the extent of ischaemia. Angina usually lasts less than 20 minutes and there may be some benefit from oxygen and sublingual nitrates. The temporal pattern of angina is of prognostic significance (Table 6.1).
Table 6.1 Unstable angina—Braunwald classification
| Class | Description | Risk of AMI/death in next year |
|---|---|---|
| I | New onset exertional angina; angina with less effort; no rest pain | 7% |
| II | Angina at rest within the last month but no pain in last 48 hours | 10% |
| III | Angina at rest in the last 48 hours | 11% |
There may be overlap with other chest pain syndromes. Some patients describe burning pain suggestive of gastro-oesophageal reflux, and while sharp, stabbing or even pleuritic-type pain makes myocardial ischaemia unlikely, it does not exclude this diagnosis. Pope et al found up to 22% of patients with the principal complaint of sharp stabbing pain had an acute coronary syndrome.1,2
A number of diagnostic decision tools using history and ECG findings to assist with diagnosis have been proposed (e.g. the acute cardiac ischaemia (ACI) predictive instrument), which probably increase the accuracy of diagnosis.3 However a high index of suspicion is the most useful safeguard.
Other potentially life-threatening causes of chest pain
Pulmonary embolism
(See also Chapter 10, ‘Pulmonary emboli and venous thromboses’.)
Pleuritic pain can also be caused by pulmonary embolism, where there is a complicating pulmonary infarction and pleural irritation; however, massive pulmonary embolism can also cause central chest discomfort suggestive of angina. This is often associated with dyspnoea and haemodynamic collapse, and may reflect acute right ventricular dysfunction.
Pneumonia
Pleuritic chest pain is a common feature of respiratory tract infections which involve the pleura.