CHAPTER 9
Tension-Type (Muscle Contraction) Headache
Presentation
The patient complains of a mild to moderate, dull, steady (nonpulsating) pain, described as a pressing, tightening, squeezing, or constricting band, located bilaterally anywhere from the eyes to the occiput, perhaps including the neck or shoulders. Often the headache is a bilateral tightness or sensation of pressure around the temples. Most commonly, the headache develops near the end of the day or after some particularly stressful event. There is usually no photophobia, nausea, or vomiting, although photophobia and phonophobia can occur (but not both), and the patient may be anorexic. These headaches may also be associated with lightheadedness and feeling tired. Tension-type headache pain can last from 30 minutes to several days and can be continuous in severe cases. It is classified as infrequent episodic (<1 day per month), frequent episodic (1 to 14 days per month), and chronic (>15 days per month and can occur with or without muscle spasm). The pain may improve with rest or administration of nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, or other medications. The physical examination is unremarkable, except for possible cranial or posterior cervical muscle spasm or tenderness and difficulty relaxing.
What To Do:
 Obtain a complete general history (including environmental factors and foods that precede the headaches) and perform a physical examination (including a neurologic and funduscopic examination).
Obtain a complete general history (including environmental factors and foods that precede the headaches) and perform a physical examination (including a neurologic and funduscopic examination).
 If the patient complains of a sudden onset of the “worst headache of my life”—a thunderclap headache that reaches maximal intensity within 1 minute or a headache accompanied by any change in mental status, weakness, seizures, stiff neck, or persistent neurologic abnormalities— suspect a cerebrovascular cause, especially a subarachnoid hemorrhage, intracranial hemorrhage, aneurysm, or arteriovenous malformation. The usual initial diagnostic test for these is CT. Other indications for a CT scan are changes in frequency, severity, or clinical features of the headaches or a new, daily, persistent headache.
If the patient complains of a sudden onset of the “worst headache of my life”—a thunderclap headache that reaches maximal intensity within 1 minute or a headache accompanied by any change in mental status, weakness, seizures, stiff neck, or persistent neurologic abnormalities— suspect a cerebrovascular cause, especially a subarachnoid hemorrhage, intracranial hemorrhage, aneurysm, or arteriovenous malformation. The usual initial diagnostic test for these is CT. Other indications for a CT scan are changes in frequency, severity, or clinical features of the headaches or a new, daily, persistent headache.
 A CT scan is also needed in evaluating the first headache in a patient 35 years old or older, or when exertion precipitates a headache that persists after the exertion stops, or when pain awakens the patient from sleep, or when the headache pain is unilateral or focal.
A CT scan is also needed in evaluating the first headache in a patient 35 years old or older, or when exertion precipitates a headache that persists after the exertion stops, or when pain awakens the patient from sleep, or when the headache pain is unilateral or focal.
 If the headache is accompanied by fever and stiff neck or change in mental status, rule out bacterial meningitis as soon as possible by performing a lumbar puncture (LP).
If the headache is accompanied by fever and stiff neck or change in mental status, rule out bacterial meningitis as soon as possible by performing a lumbar puncture (LP).
 If there is a history or suspicion of head injury, especially in elderly patients or those on anticoagulants or with a bleeding diathesis, obtain a CT scan to rule out an intracranial hemorrhage. Chronic alcoholic patients must be presumed to be coagulopathic in these circumstances.
If there is a history or suspicion of head injury, especially in elderly patients or those on anticoagulants or with a bleeding diathesis, obtain a CT scan to rule out an intracranial hemorrhage. Chronic alcoholic patients must be presumed to be coagulopathic in these circumstances.
 If the headache is nonspecific or was preceded by ophthalmic or neurologic symptoms that are now resolving, which is suggestive of a migraine headache, try prochlorperazine, sumatriptan, or ergotamine therapy (see Chapter 6). If vasospastic neurologic symptoms persist into the headache phase, the cause may still be a migraine, but it becomes more important to rule out other cerebrovascular causes.
If the headache is nonspecific or was preceded by ophthalmic or neurologic symptoms that are now resolving, which is suggestive of a migraine headache, try prochlorperazine, sumatriptan, or ergotamine therapy (see Chapter 6). If vasospastic neurologic symptoms persist into the headache phase, the cause may still be a migraine, but it becomes more important to rule out other cerebrovascular causes.
 If the headache follows prolonged reading, driving, or television watching, and decreased visual acuity is improved when the patient looks through a pinhole, the headache may be the result of a defect in optical refraction, which is correctable with new eyeglass lenses.
If the headache follows prolonged reading, driving, or television watching, and decreased visual acuity is improved when the patient looks through a pinhole, the headache may be the result of a defect in optical refraction, which is correctable with new eyeglass lenses.
 If the temporal arteries are tender, check for visual defects, jaw claudication, myalgias, and an elevated erythrocyte sedimentation rate, which accompany temporal arteritis.
If the temporal arteries are tender, check for visual defects, jaw claudication, myalgias, and an elevated erythrocyte sedimentation rate, which accompany temporal arteritis.
 If there is a history of recent dental work or grinding of the teeth, tenderness anterior to the tragus, or crepitus on motion of the jaw, suspect arthritis of the temporomandibular joint.
If there is a history of recent dental work or grinding of the teeth, tenderness anterior to the tragus, or crepitus on motion of the jaw, suspect arthritis of the temporomandibular joint.
 If there is fever, tenderness to percussion over the frontal or maxillary sinuses, purulent drainage visible in the nose, or facial pain exacerbated by lowering the head, consider sinusitis.
If there is fever, tenderness to percussion over the frontal or maxillary sinuses, purulent drainage visible in the nose, or facial pain exacerbated by lowering the head, consider sinusitis.
 If pain radiates to the ear, inspect and palpate the teeth for tenderness. Dental pain is a common cause of such headache pain.
If pain radiates to the ear, inspect and palpate the teeth for tenderness. Dental pain is a common cause of such headache pain.
 Finally, after checking for all other causes of headache, palpate the temporalis, occipitalis, and other muscles of the calvarium and neck to look for areas of tenderness and spasm that sometimes accompany muscle tension headaches. Watch for especially tender trigger points (Figure 9-1) that may resolve with gentle pressure, massage, or trigger-point injection (see Chapter 123). Such trigger-point injection may completely relieve symptoms within 5 to 10 minutes. Pain relief helps to make the diagnosis more certain.
Finally, after checking for all other causes of headache, palpate the temporalis, occipitalis, and other muscles of the calvarium and neck to look for areas of tenderness and spasm that sometimes accompany muscle tension headaches. Watch for especially tender trigger points (Figure 9-1) that may resolve with gentle pressure, massage, or trigger-point injection (see Chapter 123). Such trigger-point injection may completely relieve symptoms within 5 to 10 minutes. Pain relief helps to make the diagnosis more certain.
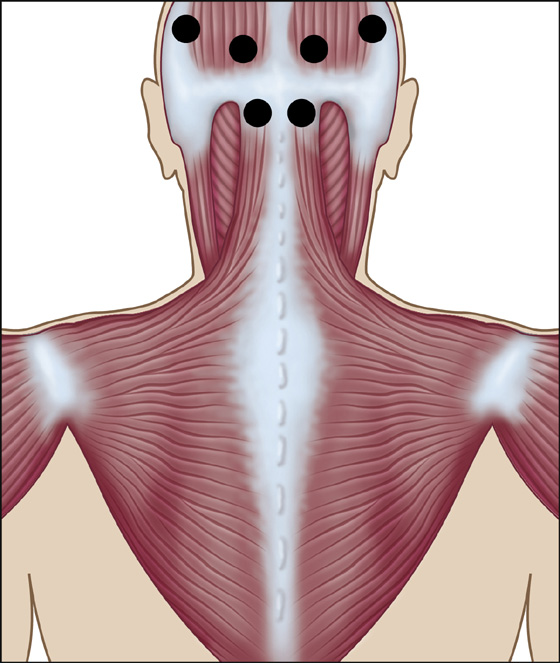
Figure 9-1 Tension headache trigger points.
 If there are no contraindications, prescribe anti-inflammatory analgesics (e.g., ibuprofen, naproxen) which, in recent studies, have been shown to be more efficacious than acetaminophen. Recommend rest, and have the patient try applying cool compresses and massaging any trigger points. If NSAIDS are contraindicated, acetaminophen may also be effective.
If there are no contraindications, prescribe anti-inflammatory analgesics (e.g., ibuprofen, naproxen) which, in recent studies, have been shown to be more efficacious than acetaminophen. Recommend rest, and have the patient try applying cool compresses and massaging any trigger points. If NSAIDS are contraindicated, acetaminophen may also be effective.
 Explain the cause and treatment of muscle spasm of the head and neck.
Explain the cause and treatment of muscle spasm of the head and neck.
 Tell the patient that there is no evidence of other serious disease (if this is true); especially inform him that a brain tumor is unlikely. (Often this fear is never voiced.)
Tell the patient that there is no evidence of other serious disease (if this is true); especially inform him that a brain tumor is unlikely. (Often this fear is never voiced.)
 Arrange for follow-up. Instruct the patient to return to the emergency department or contact his own physician if symptoms change or worsen.
Arrange for follow-up. Instruct the patient to return to the emergency department or contact his own physician if symptoms change or worsen.
What Not To Do:
 Do not discharge the patient without providing follow-up instructions. Many serious illnesses begin with minor cephalgia, and patients may postpone necessary early follow-up care if they believe that they were definitively diagnosed on their first visit.
Do not discharge the patient without providing follow-up instructions. Many serious illnesses begin with minor cephalgia, and patients may postpone necessary early follow-up care if they believe that they were definitively diagnosed on their first visit.
 Do not obtain CT scans for patients who have long-term recurrent headaches with no recent change in pattern, no history of seizures, and no focal neurologic findings.
Do not obtain CT scans for patients who have long-term recurrent headaches with no recent change in pattern, no history of seizures, and no focal neurologic findings.
 Do not overlook possible subarachnoid hemorrhage or meningitis. Most CT scans and LP results should be normal. LP may be more sensitive than CT for detecting subarachnoid hemorrhage within 12 hours of the onset of headache.
Do not overlook possible subarachnoid hemorrhage or meningitis. Most CT scans and LP results should be normal. LP may be more sensitive than CT for detecting subarachnoid hemorrhage within 12 hours of the onset of headache.
 Do not prescribe analgesics combined with butalbital (Fioricet) or opiates. Initially, they may be useful, but they increase the risk for chronic daily headache.
Do not prescribe analgesics combined with butalbital (Fioricet) or opiates. Initially, they may be useful, but they increase the risk for chronic daily headache.
 Do not prescribe sumatriptan or ergotamine without knowledge of the patient’s previously prescribed medications, nor without arranging appropriate follow-up.
Do not prescribe sumatriptan or ergotamine without knowledge of the patient’s previously prescribed medications, nor without arranging appropriate follow-up.
 Do not treat with muscle relaxants. There are no data to support their use, and there are side effects and habituation.
Do not treat with muscle relaxants. There are no data to support their use, and there are side effects and habituation.
Discussion
Headaches are common and usually benign, but any headache brought to medical attention deserves a thorough evaluation. Screening tests are of little value; a laborious history and physical examination are required.
Tension-type headache is not a wastebasket diagnosis of exclusion but a specific diagnosis. (Tension refers to muscle spasm more than life stress.) Although tension-type headaches are common, the pathophysiology and likely mechanism remain unclear. The cause of these headaches is most likely multifactorial, including myofascial factors and heightened sensitivity of nerve fibers, both centrally and peripherally. Tension-type headache is often dignified with the diagnosis of “migraine” without any evidence of a vascular cause and is often treated with minor tranquilizers, which may or may not help. It should be appreciated that migraine and tension-like headaches share some features that may make it difficult to distinguish one from the other. In fact, there seems to be support for the theory that tension-type headache and migraine are distinct entities, as well as for the suggestion that these disorders are the extremes of a continuum.
Focal tenderness over the greater occipital nerves (C2, C3) can be associated with an occipital neuralgia or occipital headache and can be secondary to cervical radiculopathy resulting from cervical spondylosis. This tends to occur in older patients and should not be confused with tension headache.
Thunderclap headaches have been described with both ruptured and unruptured intracranial aneurysms. Even if a CT scan and LP are normal, magnetic resonance angiography is needed to rule out an unruptured aneurysm.
Other causes of headache include carbon monoxide exposure from wood-burning heaters, fevers and viral myalgias, caffeine withdrawal, hypertension, glaucoma, tic douloureux (trigeminal neuralgia), and intolerance of foods containing nitrite, tyramine, or xanthine.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


