Link: Pericardiocentesis | Constrictive Pericarditis |
A life-threatening, slow or rapid compression of the heart due to the accumulation of fluid, pus, blood, clots or gas as a result of trauma or rupture of the heart. Often occurs secondary to penetrating injuries, can also occur when a central line 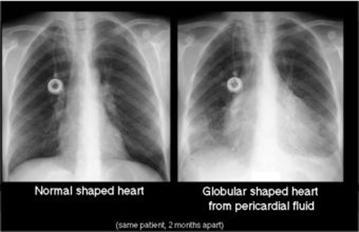 penetrates the wall of the right atrium. A form of cardiogenic shock.
penetrates the wall of the right atrium. A form of cardiogenic shock.
Etiology: malignancy, uremia, Pericarditis, Tamponade and Contusion, cardiac perforation at diagnostic procedure, TB.
PP: Tamponade occurs when the pressure in the pericardial sac exceeds the normal filling pressure of the right ventricle, resulting in restricted filling and decreased cardiac output. A consequences of pericardial fluid depend on rate of accumulation, pericardial compliance, and pt blood volume. Compensatory mechanisms include increased right-sided pressures to maintain cardiac filling, tachycardia, increased ejection fraction, and increased peripheral vascular tone, all sympathetically mediated. With decompensation, get low cardiac output and hypotension.
S/s: The most common complaints are dyspnea and decreased exercise tolerance. Other nonspecific sx’s include weight loss, pedal edema, and ascites. Pt’s tend to have tachycardia, low systolic blood pressure, and a narrow pulse pressure. Pulsus paradoxus (see below), neck vein distension, distant heart sounds, and right upper quadrant pain (due to hepatic congestion) may also be present.
Beck’s Triad –> incr systemic venous pressure (JVD), decr BP (hypotension), small quiet heart (muffled heart sounds). Also may have hypovolemic shock, PEA (= electrical alternans, a beat-to-beat variability in the amplitude of the P and R waves unrelated to inspiratory cycle) is a classic but uncommon finding (~20% of cases), decreased voltage on ECG, enlarged cardiac silhouette on CXR.
Pulsus paradoxus: (decr SBP >10 during inspir): The key diagnostic finding. = an inspiratory fall in SBP of >10mgmHg during normal breathing.
Step #1: measure BP.
Step #2: 30 sec after reinflate to 20 mmHg >SBP and deflate until hear 1st Korotkoff sound during exp.
Step #3: Deflate slowly until hear K sound throughout resp cycle, + if exp-insp >10). Pulsus paradoxus or elevated venous pressure may be absent when associated with hypovolemia. May be palpable in the muscular arteries, but of very low cardiac output, a catheter might be needed to identify. Pulses may be absent in extreme hypotension (shock), acute LV infarction, pericardial adhesions, RVH w/o pulmonary HTN, or if pt has an ASD. Some describe it as apparent dropped beats in the peripheral pulse during inspiration.
Kussmaul’s Sign: Rise in venous pressure with inspiration.
Ewart’s sign: Large pericardial effusion compression of the lung that causes an area of dullness between the angle of the scapula and spine, along with bronchial breathing and egophony in that region.
Dx: Echocardiogram to document pericardial fluid and look for RV collapse indicative of tamponade. ECG shows low voltage with electrical alternans. CXR may show increased cardiac silhouette (“water bottle”).
Purulent Pericarditis: likely to recur rapidly and progress to constrictive pericarditis, usually requires a surgical drainage procedure.
Drug-Induced Pericarditis: procainamide (SLE), minoxidil, methysergide.
Postcardiotomy syndrome: acute pericarditis.
Low Pressure Tamponade: Seen in pt’s with hypovolemia and severe systemic dz’s, hemorrhage, cancer or after diuresis. Seen with diastolic pressures of 6-12mmHg.
Hypertensive Tamponade: occurs at a high arterial BP due to excessive beta-adrenergic drive.
Regional Cardiac Tamponade: due to localized loculated effusions compressing a cardiac zone. Seen with pericardial adhesions after cardiac surgery.
Tx: Fluids and vasopressor agents are temporizing measures. Definitive therapy is removal of pericardial fluid: pericardiocentesis, pericardial window.
Malignant effusion: In men r/o lung Ca, in women r/o breast cancer. Lymphoma and melanoma also metastasize to pericardium. Cytologic examination of the pericardial fluid is highly accurate in diagnosing common carcinomas but less accurate in diagnosing other neoplasms, especially the lymphomas and leukemias. Can be managed conservatively when no sx’s directly related to the effusion are present. If sx’s, manage palliatively with pericardiocentesis, although recurrent effusion is more likely to form in such cases than in many other types of pericardial effusion. Subxiphoid pericardiostomy is often the preferred procedure, leading to a pericardial reaction that produces adhesion of the parietal and visceral layers of pericardium and thus prevents recurrent effusion. Balloon pericardiostomy is an alternative. Chemo or XRT may be of value, depending on the neoplasm. Intrapericardial instillation of chemotherapeutic agents has often been used with success. (Acute cardiac tamponade. NEJM 2003;349:684-90)









