Key Clinical Questions
How do you initially manage a patient with a hemodynamically unstable wide complex tachyarrhythmia?
What are the electrocardiographic features that suggest that a wide complex tachyarrhythmia is of ventricular origin?
What are the electrocardiographic features that suggest that a wide complex tachyarrhythmia is of supraventricular origin?
What is the differential diagnosis for short RP tachycardia? What is the differential diagnosis for long RP tachycardia?
Radiofrequency ablation often cures which tachycardias?
Introduction
This chapter will review the initial bedside approach to a hospitalized patient with a new, potentially life-threatening tachycardia, defined as a heart rate ≥ 100 beats per minute (bpm). The reader is then referred to the cardiology chapters for definitive management of specific arrhythmias.
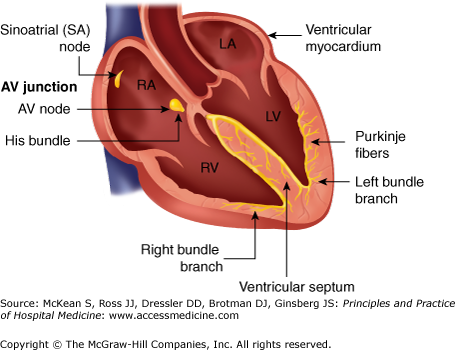
Normally, the sinoatrial node spontaneously activates the right atrium, then the interatrial septum, and then the left atrium. The initial portion of the P wave represents depolarization of the right atrium and the last portion depolarization of the left atrium. Normally, the atrioventricular (AV) node, His bundle, and bundle branches transmit impulses anterogradely from the atria to the ventricles. The QRS complex represents ventricular depolarization and the ST-T-U complex represents repolarization (Figure 100-1).
Unlike the normal AV conducting pathway, anomalous bands of tissue—accessory pathways—may be able to conduct in both directions between the atria and ventricles in a retrograde and antegrade fashion. Some anomalous bands of tissue, concealed bypass tracts, can conduct in a retrograde direction only from the ventricles to the atria.
Supraventricular tachycardias (SVTs) include all tachycardias that arise above the bifurcation of the bundle of His or that have mechanisms depending on the bundle of His.
Paroxysmal supraventricular tachycardias usually have narrow complexes with a normal QRS duration of < 90 ms; some, however, may have aberrant conduction notable for a different QRS configuration from the baseline ECG. Intraventricular conduction disturbances may be incomplete (100–120 ms) or complete bundle branch blocks (QRS ≥ 120 ms in duration) and may be rate related. A right bundle branch block (RBBB) configuration is more common than a left bundle branch block (LBBB) aberrant pattern. The altered depolarization causes secondary repolarization ST-T abnormalities, discordance of QRS-T wave vectors. Ischemia, electrolyte disturbances, and digitalis cause primary depolarization ST-T abnormalities independent of the QRS vector. Sudden death from SVT is rare.
Initial Approach
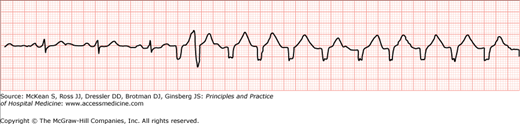
POSTOPERATIVE TACHYCARDIA A 65-year-old female with past medical history of hypertension, rheumatoid arthritis, osteoarthritis, and GERD underwent elective left total hip replacement. After transfer to the floor, at 11:00 PM she had an asymptomatic 15-beat run of wide-complex tachycardia with a variable heart rate ranging from 60–120 beats per minute (bpm). Initial data: Telemetry (Figure 100-2) showed a wide-complex tachycardia at a heart rate of 120. Vital signs: Systolic blood pressure was 110–140 mm Hg, O2 saturation 98–100% shovel mask, afebrile. |
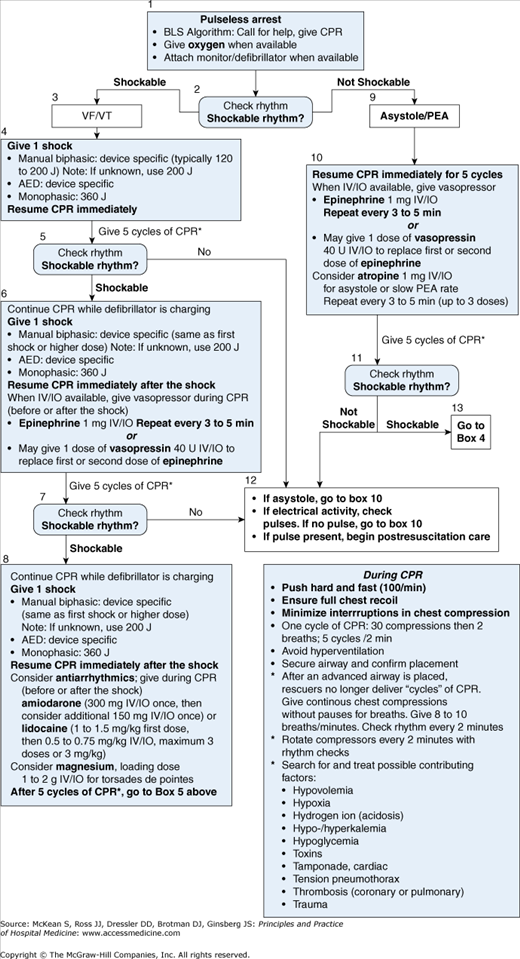
Critical assessment of a tachyarrhythmia requires a determination of whether the patient has a potentially life-threatening arrhythmia. The first step always begins with reviewing the patient’s vital signs and identifying any artifacts that may have produced ECG findings mimicking cardiac arrhythmias. For example, motion artifact from muscle tremors or rigors may produce ECG changes that simulate cardiac tachyarrhythmias on a cardiac monitor tracing. When hemodynamic instability exists, VT is assumed as the cause of the wide-complex tachycardia, and clinicians should proceed promptly to direct-current cardioversion according to ACLS protocols (Figure 100-3).
|
In hemodynamically stable patients with sustained SVT, clinicians should try to determine the mechanism of the tachycardia before initiating treatment.
The goal of ECG interpretation is to identify the location of the ectopic impulse formation and to look for evidence of myocardial ischemia. (See Chapter 102: The Resting Electrocardiogram).
|
During the assessment of hemodynamic stability, clinicians examine the monitor strip to determine whether the QRS complex is narrow (<90 ms) or wide (> 90 ms). A SVT with intraventricular aberrant conduction, a SVT conducting to the ventricles over an accessory pathway, and a VT can all produce wide complex regular tachycardia. Distinguishing VT from SVT with aberrancy or SVT over an accessory pathway has important management implications.
Until proven otherwise, patients who have a wide QRS complex tachycardia and a history of structural heart disease (coronary artery disease or cardiomyopathy) are assumed to have VT. Application of the Brugada criteria may help differentiate VT from SVT with aberrant conduction, but requires interpretation of a 12-lead ECG.
Brugada criteria
|
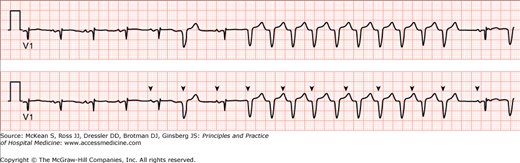
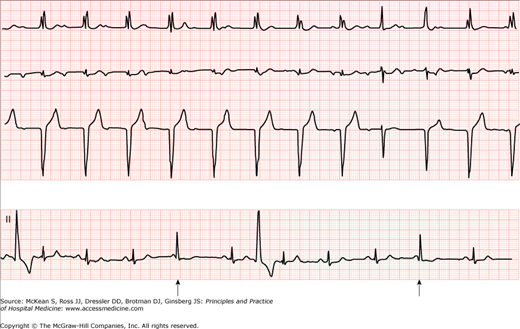
The presence of atrioventricular (AV) dissociation, fusion beats, and capture complexes generally favor the diagnosis of VT. AV dissociation, when the atrial and ventricular rhythms are independent of each other, is present when the P waves “march” through the tachycardic sequence and surface at the appropriate time interval after the last QRS complex of the tachycardia. The ventricular rate is greater than or equal to the atrial rate. The absence of P waves in up to 70% of the VT cases, should not, therefore, reassure the examiner that the arrhythmia is supraventricular in origin. In addition, AV dissociation may occur in the presence of an accelerated junctional rhythm that is faster than sinus rhythm and hence is not specific for VT (Figure 100-4).
Fusion beats, arising from simultaneous activation of the ventricle from two sources, have a QRS configuration that is intermediate between supraventricular and ventricular complexes, and arise when the ventricle is depolarized simultaneously via the normal conduction system and a ventricular focus (Figure 100-5).
A markedly widened QRS > 140 ms supports the diagnosis of VT, especially if associated with a left axis of the QRS complex in the frontal plane. Activation of the ventricles over an accessory pathway generally proceeds from the base toward the apex resulting in predominantly positive QRS complexes in the precordial leads V4 to V6. The finding of negative QRS complexes in leads V4 to V6 makes VT more likely, since an LBBB conduction pattern has negative QRS complexes in these leads (Table 100-1).
| Ventricular Tachycardia More Likely… | SVT with Aberrancy More Likely… |
|---|---|
|
|
| VPC | APC |
|
|
In patients with SVT, the heart rate must be ≥ 100 bpm but ventricular rates can be lower due to the presence of AV block. Sinus tachycardia is a regular narrow complex rhythm with a rate > 100 bpm. P waves are usually visible unless the rate is so rapid that they are buried in the T waves. Physiologic stress commonly causes sinus tachycardia, which should lessen with treatment of the underlying problem (such as postoperative pain, hypovolemia from blood loss or insufficient oral intake, sepsis, or withdrawal states).
Most patients with atrial flutter (AFl) have an atrial rate around 300 beats per minute, so with 2:1 conduction, the ventricular rate will be about 150 bpm and characteristic negatively directed “sawtooth” atrial waveforms are present in the inferior leads. The mechanism of this common form of Type I classic AFl is a macro reentrant circuit around the entire right atrium in a counterclockwise direction. A less common form of classic AFl occurs when a macro reentrant circuit proceeds around the right atrium in a clockwise direction, producing positive atrial waveforms in the inferior leads. Type II AFl has faster atrial rates in the range of 340 to 440 bpm. Sometimes the P wave can get buried in the T wave and be missed unless multiple leads from the ECG are examined. Carotid sinus pressure or adenosine administration may transiently slow the ventricular rate so that atrial waveforms can be appreciated (Figure 100-6).