Synthesis of Migraine Mechanisms
Jes Olesen
Peter J. Goadsby
Mechanisms of disease are rarely simple. Many years after the description of the nigral pathology of Parkinson disease and the introduction of L-DOPA, there are perhaps as many questions unanswered as answered. A simple explanation for migraine is similarly unlikely. In attempting a synthesis of migraine mechanisms, we try to integrate what we know of the clinical science with what has been observed in the clinic to provide an overview of the systems that are involved. Specifically, we shall consider:
Genetic factors
Environmental predisposition
Interictal physiologic and biochemical traits
Precipitation of attacks
Pathophysiology, both peripheral and central, of the pain of the attack
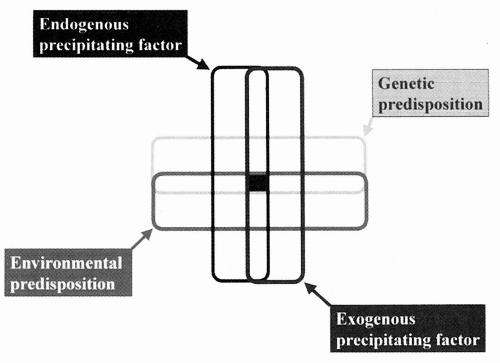
Figure 42-1 illustrates how some of these factors interact to express migraine as a disease and to initiate the individual attack.
GENETIC FACTORS
If a person on average has seven first-degree relatives, then, because of the high lifetime prevalence of migraine, there should be an average of one affected first-degree relative just by chance. Because of random unevenness of distribution, many probands by chance have two, three, or even four affected relatives, and such families have a high likelihood of being reported as cases of dominant inheritance. Therefore, genetic-epidemiologic studies are critical. They have shown a twofold increased risk of migraine without aura among first-degree relatives and a fourfold increase in migraine with aura (33). Furthermore, twin studies have recently provided convincing evidence of a genetic component to migraine. Thus, the concordance rate of migraine in monozygous twins was significantly higher than in dizygous twins (38,39).
Missense mutations in the CACNA1A gene on chromosome 19 encoding the α1 subunit of the voltage-gated P/Q calcium channel explain many cases of familial hemiplegic migraine (30). Other families harbor mutations in the ATP1A2 gene on chromosome 1 encoding the NaK-ATPase (10). Yet others do not map to either. Remarkably there seems little correlation between the mutations and the clinical expression of these disorders (11). As described in Chapter 27, linkage studies in migraine with and without aura have suggested linkage to a number of other sites in migraine with aura (MA) and migraine without aura (MO). Almost certainly genes for MA and MO will be identified in the next decade.
ENVIRONMENTAL PREDISPOSITION
The genetic predisposition to migraine does not always express itself. Thus, monozygotic twins with migraine were only concordant in 20 to 50% of cases (33). At least 50% of those carrying a genetic disposition to migraine thus never manifest attacks because of favorable environmental conditions, or the 50% who do manifest the condition experience headache because of unfavorable conditions. Furthermore, apparent carriers express migraine only during part of their lifetime because the prevalence of migraine increases up to age 40 and decreases in old age (25). In a meticulous longitudinal cohort study, children with migraine often became migraine free for years or decades, but many later had recurrence of attacks (5). Some of the predisposing or triggering factors for the expression of the disease include:
Female gender
Psychosocial stress
Biochemical changes
Alcohol
The most important predisposing or priming factor seems to be the female hormonal environment, although it has
not been established beyond question that the male hormonal environment is in some way protective. The sex ratio is approximately equal before puberty, whereas females suffer from migraine three times more frequently than males after puberty (see Chapter 35). What happens after menopause has not been completely defined, although it seems likely that there is improvement (25). Psychosocial stress also seems to be an important predisposing factor (see Chapter 41). Patients reporting to a doctor as a consequence of increased attack frequency often do so at times of psychosocial stress, and the attack frequency returns to the usual pattern after removal of, or adaptation to, the stressor. It seems likely that psychosocial stress can also cause the onset of migraine in persons who have not previously expressed it. Similar but less solid evidence indicates that certain foods, alcoholic drinks, and perhaps biochemical and myogenic changes may enhance expression of any genetic predisposition and thereby cause expression or worsening of migraine (see Chapters 33, 34, and 36). Several researchers have discussed the existence of a migraine threshold that may be high or low, depending on genetic as well as environmental predisposing factors. A particularly elegant and penetrating discussion of this concept was given by Welch et al. (41).
not been established beyond question that the male hormonal environment is in some way protective. The sex ratio is approximately equal before puberty, whereas females suffer from migraine three times more frequently than males after puberty (see Chapter 35). What happens after menopause has not been completely defined, although it seems likely that there is improvement (25). Psychosocial stress also seems to be an important predisposing factor (see Chapter 41). Patients reporting to a doctor as a consequence of increased attack frequency often do so at times of psychosocial stress, and the attack frequency returns to the usual pattern after removal of, or adaptation to, the stressor. It seems likely that psychosocial stress can also cause the onset of migraine in persons who have not previously expressed it. Similar but less solid evidence indicates that certain foods, alcoholic drinks, and perhaps biochemical and myogenic changes may enhance expression of any genetic predisposition and thereby cause expression or worsening of migraine (see Chapters 33, 34, and 36). Several researchers have discussed the existence of a migraine threshold that may be high or low, depending on genetic as well as environmental predisposing factors. A particularly elegant and penetrating discussion of this concept was given by Welch et al. (41).
One interpretation is that migraine sufferers inherit a lack of ability to adapt to physiologic changes, particularly those of a sensory nature. Stimuli or behavior that present no problem to the nonmigraineur may therefore trigger an attack in those predisposed to migraine. A migraineur may trigger attacks by sleeping late or getting up too early, by skipping meals or overindulging in certain foods, by experiencing too much stress or during periods of relaxation, such as early in a holiday. The migraine sufferer’s brain is more sensitive to change, and although there is no fixed trigger, the broad principle of unstable sensory processing, which is probably intimately linked to dysfunction of aminergic control pathways, serves us well when advising patients about lifestyle changes (14).
PHYSIOLOGIC AND BIOCHEMICAL ABNORMALITIES OUTSIDE OF ATTACKS
Physiologic and biochemical abnormalities in migraine sufferers outside of attacks may be genetic or environmental, but the former is most likely when changes are present weeks after the last attack and when they persist for years. The interictal hypersensitivity to nitroglycerine (Chapter 30) and calcitonin gene-related peptide (CGRP; Chapter 31), and abnormal contingent negative variations; the interictal biochemical, platelet, and magnesium abnormalities described in Chapter 34; and the interictal inhomogeneity of regional cerebral blood are important examples. Regardless of the genetic or environmental cause of these changes, it is likely that migraine patients have both a biochemical and a physiologic preparedness for developing attacks. This explains why precipitating factors cause attacks in some persons and not in others.
PRECIPITATION OF ATTACKS
Some migraine patients get attacks as rarely as once a year, some as often as once a week, but most do not have it all the time (see Fig. 42-1). Why does the attack come at a particular time in a particular patient? The answer is sometimes known, such as with red wine, stress, or food, but in most cases it is not. Even in those cases where one or more precipitating factors are thought to explain the migraine attack, relationships are complicated. Not every exposure to the precipitant induces an attack, and it seems most likely that endogenous and exogenous factors must coincide to precipitate attacks in most individuals (see Fig. 42-1). This fact may explain why most patients have rare attacks. How and where do these precipitating factors exert their migraine-triggering effects? More specifically, are these effects generated within or outside of the central nervous system (CNS)? Could both indeed be possible? Some factors such as emotional disturbances, psychosocial stress, and strong light undoubtedly act primarily on the CNS. Other factors are more likely to work systemically, such as fasting and the effects of various foods. All of these may, however, affect the CNS either by
substances crossing the blood-brain barrier or via sensory afferent impulses projecting to the CNS. Most recently the discovery of many different endothelial receptors on the brain and extracerebral arteries (26) has revealed new possibilities for changes in blood chemistry, such as changes in plasma serotonin (5-HT) or glutamate, to trigger migraine by affecting cerebral arteries.
substances crossing the blood-brain barrier or via sensory afferent impulses projecting to the CNS. Most recently the discovery of many different endothelial receptors on the brain and extracerebral arteries (26) has revealed new possibilities for changes in blood chemistry, such as changes in plasma serotonin (5-HT) or glutamate, to trigger migraine by affecting cerebral arteries.
HOW AND WHERE PAIN FIBERS (NOCICEPTORS) BECOME EXCITED DURING MIGRAINE ATTACKS
In this section, we discuss the mechanisms of the migraine aura and the mechanisms of the pain phase of the attack. We propose that aura mechanisms are unique to MA, and that MA and MO are identical in terms of the painful phase of the attack. This view is based on the similar clinical characteristics of pain and associated symptoms (34), the frequent co-occurrence of the two conditions (34), a number of pathophysiologic similarities (19), and the identical response of both forms to prophylactic and acute treatment (19).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree