Symptomatology of Chronic Tension-Type Headaches
Rigmor Jensen
Werner J. Becker
Except for its frequency, chronic tension-type headache (CTTH) is similar to frequent episodic tension-type headache (ETTH) in most of its clinical features. The International Classification of Headache Disorders (ICHD) II (21) distinguished between these two headache types mainly because of the differences in management rather than because of differences in the clinical features. However, it has recently been suggested that the chronic type may be due to a different pathophysiology (1,5,23), is associated with more severe pain and more accompanying symptoms, and is less influenced by daily hassles and stress than ETTH (31,45,55).
The headache syndromes with frequent headaches were the most controversial part of the ICHD-I. They have been much discussed and strong efforts have been made to improve the diagnostic criteria (6,16,41,53). The revised diagnostic criteria for CTHH as published in IHCD-II are shown in Table 78-1 (21).
These criteria are somewhat more specific than those in the ICHD-I (20). For example, whereas the length of headache suffered per day was not specified previously, it is now specified that the headache lasts hours or may be continuous. To make a diagnosis of CTTH, these headaches need be present only for a period of at least 3 months (not 6 months as specified in IHCD-I [20]). In the revised version, it is also specified that no more than one of photophobia, phonophobia, or mild nausea may be present (21). Moderate or severe nausea or vomiting precludes the diagnosis.
In the ICHD-II, CTTH is also described as a disorder evolving from ETTH (21). It is further specified that if the headache is continuous from the start or becomes continuous within 3 days of first onset, then headaches of this type should be coded to new daily persistent headache rather than to CTTH (see Chapter 103).
It must also be kept in mind when making a diagnosis that when medication overuse is present to a degree that fulfills the amounts specified in the diagnostic criteria for medication overuse headache in Chapter 8 of the ICHD-II, a diagnosis of probable CTTH should be made. In addition, such a patient would also receive a diagnosis of probable medication overuse headache, and a definitive diagnosis would not be possible until medication overuse has ceased for 2 months. When this has occurred, if the patient no longer has headache more than or equal to 15 days per month, then the patient in retrospect had medication overuse headache. If the chronic headache persists despite stopping medication overuse, then the patient should be reclassified as CTTH.
The diagnostic criteria for probable CTTH therefore are identical to those for CTTH, except that criterion E reads “not attributed to another disorder but there is, or has been within the last 2 months, medication overuse fulfilling criterion B for any of these subforms of 8.2 Medication-overuse headache” (21).
CLINICAL PICTURE OF CHRONIC TENSION-TYPE HEADACHE
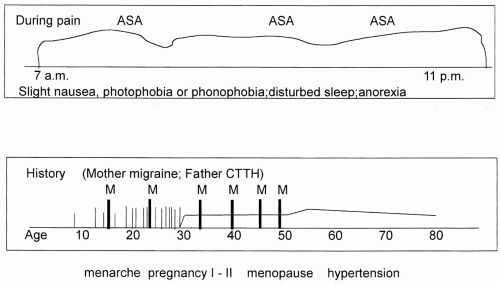
The typical patient with CTTH is a middle-aged female patient with a headache history for 10 to 20 years (6,24,49,51,54) and with a more or less continuous daily headache that has proven largely refractory to numerous treatment strategies and that is quite independent of daily activities (Fig. 78-1). The majority of patients have a history of an episodic headache disorder in their adolescence, either migraine or ETTH or both. Their headaches have then gradually increased in frequency over several years without any obvious explanation, and at the time of diagnosis have been chronic for several years (57). No specific associations to other diseases can be detected, although, as in other chronic pain disorders, depression and anxiety are frequently reported (19,33,40). Most of these patients
have adapted to their chronic headache and have lost any hope of finding new effective therapeutic strategies. They are primarily seeking specialist consultation because of a change in their headache pattern or because of other neurologic complaints. These patients therefore represent a great clinical and therapeutic challenge.
have adapted to their chronic headache and have lost any hope of finding new effective therapeutic strategies. They are primarily seeking specialist consultation because of a change in their headache pattern or because of other neurologic complaints. These patients therefore represent a great clinical and therapeutic challenge.
TABLE 78-1 Diagnostic Criteria for Chronic Tension-Type Headache | |
|---|---|
|
A minimum headache frequency of at least 15 days per month during at least 3 months is required in the ICHD-II for a diagnosis of CTTH (21) (Table 78-1), but significant headache symptoms have usually been present for a much longer time when patients seek a specialist. The number of days with headache per month in CTTH is usually very high. The mean frequency in prospective diary studies was between 23 and 30 days per month (8,29). These studies support the clinical observation that if the headache frequency is above 15 days per month it very often becomes a daily or almost daily pain. On the other hand, it is important to emphasize that patients may overreport the frequency of their TTH during an initial clinical interview as compared to the frequency recorded in a prospective headache diary (48). It is therefore recommended that a diagnostic headache diary be used in the diagnosis of both ETTH and CTTH.
The reported median age at onset is in the second decade (46,51), with a declining prevalence with increasing age in one study (46) and an increasing prevalence with increasing age in other more recent studies (51) (Lyngberg et al. 2004). The presumed evolution of CTTH from the episodic form is indirectly indicated by an older mean age in CTTH (>50 years) than in ETTH (51) (Fig. 78-1). (For further details see Chapter 67 on the epidemiology of TTH.)
Because CTTH is a condition defined purely by clinical diagnostic criteria and not by a specified pathology, its clinical features are constrained by these. For CTTH, negative diagnostic criteria specifying what is not present play an important role, in contrast to migraine, where positive symptoms play a more prominent role in the diagnostic criteria (21).
The sensitivity and specificity of the diagnostic criteria of CTTH are not fully elucidated. In an attempt to allow research on completely pure groups of TTH patients without any migrainous features, very strict diagnostic criteria have been defined in the ICHD-II appendix (21). In future genetic and pathophysiologic studies it may also be of major importance that coexisting TTH is identified in migraine patients and that completely pure groups of migraineurs and TTH patients are studied separately.
CHARACTER OF PAIN
Patients often describe their pain as “wearing a tight hat, wearing a tight band around the head, or bearing a heavy burden on the head” (22,34). This pressing pain quality
was confirmed by 83% of CTTH sufferers in a general population study (47) and was present in 72 to 95% of patients with daily or almost daily TTH from specialized headache clinics (22,38).
was confirmed by 83% of CTTH sufferers in a general population study (47) and was present in 72 to 95% of patients with daily or almost daily TTH from specialized headache clinics (22,38).
LOCATION OF PAIN
The bilateral location of the pain is considered to be a frequent characteristic of TTH and is also a part of the IHCD-II diagnostic criteria (Table 78-1). However, the location of pain may vary considerably within and between patients (17). Rasmussen et al. (47) have reported that bilateral location was present in 88% of subjects with CTTH from the general population. Similarly, in a specialized headache clinic 98% of 100 consecutive patients reported bilateral location (54). Bilateral location was also reported by 79 to 85 % of CTTH patients from two European clinical studies (8,38). Anterior-posterior pain location has not been examined in recent studies but was reported as frontal, temporal, or frontotemporal in 66% of patients and was limited to the occipital region in 25% of the patients in older clinical studies (17,22,34).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree