Introduction
Surgical drains are used to monitor for a postoperative leak or abscess, collect normal physiologic fluid or to minimize dead space. Table 47-1 lists various types of drains, as well as their locations and indications. Although caregivers should know the location and purpose of drains, they should not manipulate surgical drains without input from the surgeon who placed them.
| Type | Location | Clinical Indication | Clinical Scenario |
|---|---|---|---|
| Chest tube | Pleural space | Pneumothorax | Trauma, cardiac surgery, malignant effusion |
| Mediastinal space | Hemothorax | ||
| Pleural effusion | |||
| Nasogastric tube | Stomach | Intestinal decompression, gastric feeding | Small bowel obstruction, temporary dysphagia |
| Gastric tube (gastrostomy) | Stomach | Prolonged enteral access, or gastric decompression | Prolonged mechanical ventilation, malignant gastric outlet obstruction |
| Jejunal tube (jejunostomy) | Jejunum | Prolonged postgastric feeding in the setting of gastroparesis, gastric outlet obstruction, or high aspiration risk | Prolonged mechanical ventilation, malignant gastric outlet obstruction, recurrent aspiration pneumonia |
| Duodenal | Duodenum | Post gastric feeding in the setting of gastroparesis, gastric outlet obstruction or high aspiration risk | Mechanical ventilation, dysphagia, acute aspiration risk |
| Penrose drains | Peritoneal space, small surgical space | Used to maintain surgical tract for adequate drainage | |
| Closed suction drains | Surgical space | Evacuate serous fluid or blood | Mastectomy, ventral hernia repair, plastic surgery flaps, gastrointestinal anastomoses |
| Prevent seroma formation | |||
| Jackson Pratt | Tissue apposition to improve wound healing | ||
| Hemovac | Drain gastrointestinal secretions | ||
| Vacuum-assisted closure device | Open wound | Accelerated wound closure | Open trunk or extremity wound |
|
Types and Uses of Surgical Drains
Chest tubes are placed in the pleural space to evacuate air or fluid. They can be as thin as 20 French or as thick as 38 French and are typically placed between the fourth and fifth intercostal space in the anterior axillary line. However, location may vary according to the type of surgery. The tubes can be straight or angled. Angled tubes are used primarily to collect fluid and are usually placed near the diaphragm.
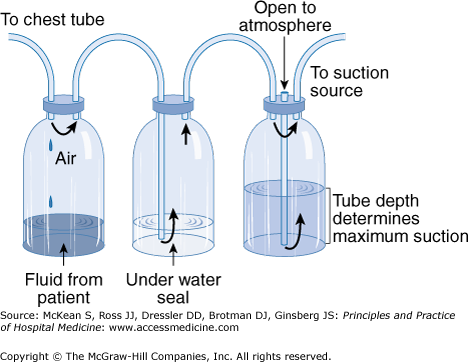
The tubes are connected to a collecting system with a three-way chamber (Figure 47-1). The water chamber holds a tall column of water which prevents air from being sucked into the pleural space with inhalation. The suction chamber can be attached to continuous wall suction to remove air or fluid, or it can be left without suction on water seal. The third chamber is the collection chamber which should be marked at regular intervals to monitor fluid drainage.
Clinical indications for a chest tube include pneumothorax, hemothorax, or a persistent or large pleural effusion. Pneumothorax and hemothorax are emergent indications, but, in the operating room, chest tubes are usually placed after thoracic surgery or when the diaphragm has been violated and air has entered the pleural space. For large, loculated empyemas video-assisted thoracoscopic surgery (VATS) is preferable to chest tube drainage. A chest X-ray should be obtained after any chest tube insertion. Although chest tubes should be well secured, they can migrate, and it is wise to get a daily chest X-ray to document the location of the tube. Chest tubes are equipped with a radiopaque line, which should be visible on chest X-ray. There is a gap in the line on the tube that should be visible in the pleural space on the film. Respiratory variation in the fluid in the collecting tube will be seen if the tube is well placed. If the patient experiences ongoing pain, fever, or inadequate drainage, a chest computed tomographic (CT) scan can identify malpositioning of the tube. There is no indication for prophylactic antibiotics for chest tubes. If a chest tube needs adjustment, it can be pulled out, but it should never be advanced into the cavity. The tube that has been outside the chest is contaminated and poses an increased risk of infection once advanced into the pleural space.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree