29
Surgical emergencies
Anatomy and physiology of the abdomen
A comprehensive knowledge of the anatomy and physiology of the abdomen is vitally important for the emergency nurse to assist in the rapid assessment and initiation of treatment for patients who present with a surgical emergency. The external and internal anatomy of the abdomen is broadly described in Chapter 9. The anatomy and physiology of specific abdominal organs are outlined throughout this chapter.
Oesophagus
This muscular tube extends from the pharynx to the stomach. It is about 25 cm long and lies in front of the vertebral column and behind the trachea within the mediastinum. The oesophagus transports food from the pharynx, and upper and lower oesophageal sphincters regulate the movement of food into and out of the oesophagus. Lubrication of the food is provided by mucous glands coating the inner surface of the oesophagus (Moore et al. 2009).
Stomach
The stomach is a J-shaped organ lying under the diaphragm in the epigastric, umbilical and left hypochondrial regions of the abdomen. The most superior part of the stomach is called the fundus. The largest part is the body, which has a convex area laterally called the greater curvature and a concave area medially called the lesser curvature. The final part of the stomach is the pylorus, which provides the opening into the first part of the small intestine. The muscular coats of the stomach consist of three layers: a longitudinal outer layer, a middle circular layer and an inner oblique layer of muscle fibres. The lining mucosa of the stomach is arranged into folds called rugae. These folds allow the stomach to stretch, and they disappear as the stomach is filled. The stomach acts as a food blender and reservoir, its chief function is enzymatic digestion. The cells in the stomach produce mucus, hydrochloric acid, intrinsic factor, regulatory hormones and pepsinogen, which is involved in protein digestion. The gastric juice gradually converts a mass of food into a liquid mixture – chyme – that passes fairly quickly into the duodenum (Moore et al. 2009).
The large intestine
The large intestine is responsible for the elimination of food residue and the maintenance of water and electrolyte balance. It consists of the caecum, the appendix, the ascending, transverse, descending colon, the sigmoid colon, the rectum and anal canal. The caecum – the first part of the large intestine that is continuous with the ascending colon – is a blind interstitial pouch. The vermiform (wormlike) appendix, a blind intestinal diverticulum (6–10 cm in length), arises from the caecum. The colon is about 1.8 m long, consisting of ascending, transverse, descending and sigmoid colons. The lining of the large intestine contains many mucus-producing goblet cells and columnar cells which reabsorb water. About 1 L of water enters the large intestine each day, but only about 100 mL is lost in the faeces – the rest is reabsorbed. The circular muscle layer is complete, with an incomplete longitudinal layer of muscle. Contraction of this longitudinal layer gives the colon a pouched appearance called haustra. The rectum is a straight muscular tube running from the sigmoid colon to the anal canal. This canal is about 3 cm long and is the final part of the digestive tract (Moore et al. 2009).
Abdominal wall
The abdominal wall is composed of skin, fascia and four pairs of flat, sheet-like muscles called rectus abdominis, external and internal oblique and transverse abdominis. The linea alba is a tough, fibrous band of tissue that stretches from the sternum to the symphysis pubis and is made up of the aponeurosis of the abdominal muscles. Part of the external oblique muscle forms the inguinal ligament, which runs from the anterior superior iliac pubic tubercule. Just superior to the medial end of this ligament is the superficial inguinal ring which is the outer opening of the inguinal canal. This canal contains the spermatic cord and the ilio-inguinal nerve in males and the round ligament of the uterus and the ilio-inguinal nerve in females. The posterior abdominal wall is composed of the bones of the lumbar spine and the hip bones, along with the psoas, quadratus lumborum and iliacus muscles (Moore et al. 2009).
Nursing assessment of the acute abdomen
The clinical approach to patients with surgical emergencies is the same as that of any emergency presentation. An initial overview is accomplished rapidly to evaluate that the airway is patent and protected, that air exchange is adequate, and that the patient has adequate systemic perfusion. The tools for evaluating abdominal complaints are: patient history, physical examination, imaging studies and laboratory tests. Once airway, breathing and circulation have been assessed and appropriate interventions to correct any abnormalities have been performed, the emergency nurse may proceed to gather the history of the presenting complaint. According to the literature the most common pitfall in evaluating abdominal pain is the failure to obtain a sufficiently detailed and accurate history (Bickley 2007).
History
The essential elements of the history are to determine:
• the nature, onset, location and radiation of the abdominal pain
• the presence and sequence of onset of associated symptoms such as fever, nausea, vomiting, urinary symptoms, and pelvic symptoms (in women)
• pertinent history related to bowel movements, appetite, weight changes, and menstrual history
• previous medical history of similar episodes, prior medical and surgical history, and current medication use. Alcohol intake, tobacco use and known allergies should also be ascertained
• social history related to occupation, family history, activity level, and recent foreign travel.
To establish a full clinical picture, the emergency nurse may further ascertain the following:
• appetite: has there been a recent alteration in dietary habits? Does the patient avoid certain foods for any reason? Is there any difficulty in swallowing; is there any sensation of food sticking in the throat or chest? Has there been any change in the patient’s weight? Do the patient’s clothes still fit? Is the abdomen bloated?
• tongue: the state of the tongue gives some indication of the state of hydration of the body. Patients who have been ill for some time with a gastrointestinal problem frequently have a fluid and electrolyte deficit. A dry brown tongue may be found in any severe illness, uraemia or acute intestinal obstruction. Additional longitudinal furrows may indicate dehydration
• skin: any change in skin colour, bruising or itching may be as a result of liver disease
• bowel habits: is there any constipation, diarrhoea, blood or mucus in the stool?
• energy: are there any feelings of lethargy or changes in mental status?
Pain assessment
The body is programmed to appreciate pain from areas under voluntary control and the skin. We are therefore not able to appreciate the precise location of the source of visceral pain. In pain originating in the heart, for example, impulses pass along the dermatomes of T1–T4, so the patient experiences pain across the chest and down the arms. Pain may therefore be referred to a site far from its origin; for instance, pain from the spleen may be referred to the left shoulder due to irritation of the phrenic nerve. There are several aspects to consider when assessing a patient’s pain, which can be usefully remembered by the mnemonic TROCARS (Box 29.1).
General principles of patient assessment and abdominal examination
Begin the assessment of the gastrointestinal tract by examining the patient’s hands to discover signs of disease (Table 29.1). Next examine the patient’s eyes for pale conjunctiva as this is indicative of anaemia. Enlarged lymph nodes may be found in the supra-clavicular fossa, suggestive of secondaries from a gastric carcinoma.
Table 29.1
| Clinical finding | Cause |
| Pallor | Anaemia |
| Clubbing | Cirrhosis Crohn’s disease Ulcerative colitis |
| Palmar erythema | Liver disease |
| Spoon-shaped nails | Iron deficiency |
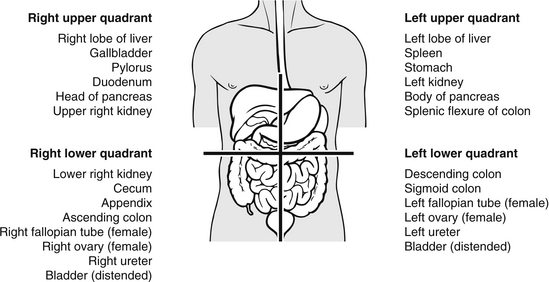
For the purposes of specific examination the abdomen can be divided into four quadrants (Fig. 29.1). To divide the abdomen into quadrants draw an imaginary line from the xiphoid process of the sternum through the umbilicus to the symphysis pubis, draw a second perpendicular line across the abdomen through the umbilicus. This divides the abdomen into quadrants: right upper quadrant, right lower quadrant, left upper quadrant and left lower quadrant and is the most common method of mapping the contents of the abdomen (Douglas et al. 2009).
In order to perform the abdominal examination satisfactorily it is essential to have a good light source and the patient should be made as relaxed as possible. Patient privacy and a full explanation of the procedure will assist in making the patient comfortable. The patient should be placed in a supine position with the head resting on a small pillow and the arms resting by the sides. In some cases the patient may be more comfortable with a small pillow under the knees, to help relax the abdominal muscles. Although it is necessary to expose the area from the sternum to the pelvis, the patient should be kept as warm as possible during the procedure, which should be performed quickly and efficiently. The patient should be examined from his right side, in a gentle manner, with warm hands and short fingernails (McGrath 2004, Bickley 2007).
Inspection
The abdomen should move freely with respiration, but this will be diminished or absent in generalized peritonitis (McGrath 2004, Epstein et al. 2008, Turner et al. 2009).
Auscultation
Auscultation should precede palpation as the latter can induce peristalsis artificially. Bowel sounds are regarded as the least helpful element of the abdominal examination because reflex ileus can occur with virtually any painful abdominal condition and might persist for some time, even with intra-abdominal catastrophes (Epstein et al. 2008, Turner et al. 2009). The emergency nurse may gain valuable experience from listening to many normal abdomens to establish a baseline. Initially, it is best to listen using the diaphragm of the stethoscope to the right of the umbilicus. Bowel sounds should be checked for at least 1 minute in all four quadrants, before declaring that they are absent. Absent bowel sounds are a feature of paralytic ileus, late obstruction and generalized peritonitis.
Percussion
Light percussion is performed to determine the presence of masses, enlargement of an organ or abdominal distension. The middle finger of the left hand is placed on the area to be percussed, and the back of its middle phalanx is struck with the tip of the middle finger of the right hand. The percussing finger should be bent, so that when the blow is delivered its terminal phalanx is at right angles to the metacarpal bone it is striking. Tympany is the normal percussion note and is a hollow resonant sound heard over the abdomen, apart from over the solid organs. Dull percussion notes will be heard over dense organs such as the liver and spleen, tumours or over a fluid-filled bladder (Epstein et al. 2008, Turner et al. 2009).
Palpation
Palpation is saved for last and should be performed gently, beginning with the quadrant most remote from the patient’s pain, moving towards the painful area. Deep palpation and the classically described test for rebound tenderness have limited utility and might be misleading (McGrath 2004, Turner et al. 2009). If the patient is not relaxed, the abdominal muscles will tense, making examination impossible. Using a warm hand flat on the abdominal wall, gently palpate all four quadrants. Palpation of specific organs requires practice, and further description is beyond the scope of this chapter. Check for the presence and equality of the femoral pulses, and assess the femoral and inguinal lymph nodes for tenderness or enlargement.
Vomit
The strongest stimuli for vomiting are irritation and distension of the stomach. Nerve impulses are transmitted to the medulla, and returning impulses to the upper gastrointestinal organs, diaphragm and abdominal muscles. The stomach is then squeezed between the diaphragm and the abdominal muscles. Prolonged vomiting will lead to loss of gastric juice and fluid. This can lead to disturbance in fluid and acid–base balance. If bleeding is severe, the vomit may look like pure blood or it may be dark with clots. Bleeding may be altered to a dark brown or black colour by gastric juice. The dark colour is due to the conversion of haemoglobin into haematin. The altered blood is sometimes compared to ‘coffee grounds’. Blood in vomit may have been swallowed from mouth injuries or epistaxis. Vomit may have a faecal odour in advanced intestinal obstruction.
Shock
The management of the patient who has lost blood or body fluids is the most important aspect of dealing with surgical emergencies. It is vital that the condition is recognized and treated promptly to reduce both morbidity and mortality. Rapid volume repletion is indicated in patients with severe hypovolaemia or hypovolaemic shock; delayed therapy can lead to ischaemic injury and possibly to irreversible shock and multiorgan failure (American College of Surgeons 2008, Smeltzer et al. 2009). The management of the patient with haemorrhage may be surgical, or in certain cases conservative. Clinical symptoms include tachycardia, hypotension, peripheral vasoconstriction, oliguria and a narrowed pulse pressure in the absence of jugular venous distension or pulmonary oedema. Monitoring of vital signs and nursing observations are of vital importance and should be carried out at least quarter-hourly. Accurate measurement of intake and all output including vomiting will assist in assessing adequate tissue perfusion. Hourly urinary output of approximately 1 mL/kg per hour is indicative of effective circulating volume (American College of Surgeons 2008, Smeltzer et al. 2009).
Management principles
• administer supplementary oxygen to maintain oxygen saturation at greater than 95 % on pulse oximetry. Oxygen can be administered through a tight-fitting oxygen reservoir face mask with a flow rate of at least 11 L/min. Other methods, such as nasal cannula, nasal catheter and non-rebreather mask can improve inspired oxygen concentration (American College of Surgeons 2008)
• initiate intravenous fluid replacement by inserting two large-bore cannulas, 14 or 16 gauge (as a minimum). Cannula should be placed in the antecubital fossa and well secured to provide an adequate flow rate. If circumstances prevent the use of peripheral veins, large-caliber, central venous access or cut-down is indicated (American College of Surgeons 2008). As intravenous lines are inserted blood is drawn for baseline laboratory investigations including blood group and cross-match and other appropriate analyses. Arterial blood gas (ABG) analysis is also performed at this time (American College of Surgeons 2008). The choice of replacement fluid depends in part upon the type of fluid that has been lost: as an obvious example blood components are indicated in patients who are bleeding (Scott 2009). In general an initial bolus of 1–2 L of warmed isotonic saline is recommended and is the preferred solution in managing patients with severe volume depletion not due to haemorrhage. Both isotonic saline solutions (crystalloid) and colloid-containing solutions are used to replace extracellular fluid deficit, but research has shown that saline solutions are as safe and effective in expanding the plasma volume as colloid and are much less expensive (American College of Surgeons 2008, Scott 2009). Following the administration of a fluid bolus it is important to assess the patient’s response by rechecking vital signs and assessing the patient’s general condition. The rate of flow is usually slowed as the blood pressure increases: too rapid an increase in blood pressure can cause further bleeding. In extreme cases of haemorrhage or haemorrhagic shock it may be necessary to give the patient O-negative blood (universal donor), while awaiting type-specific blood. Fluids should be given rapidly using a pressure device, but should be warmed to prevent inducing hypothermia. Hypothermia results in decreased tissue extraction of oxygen from haemoglobin and impaired cardiac contraction. Hypothermia also causes problems with blood clotting due to disruption of cellular enzymes and platelets, and increased fibrinolysis. An arterial line should be placed in all patients who fail to respond promptly to initial fluid resuscitation
• administer prescribed analgesia
• gastric distension can lead to vomiting, therefore inserting a gastric tube will allow decompression of the stomach and provide a sample for testing
• inserting a urinary catheter will allow accurate fluid balance and provide evidence of successful fluid volume replacement
• monitor the temperature to determine hypothermia, or pyrexia due to infection
• prepare the patient physically and psychologically for surgery where indicated.
Acute abdominal emergencies
Obstruction to the passage of contents may occur in the small or large bowel and is a serious life-threatening condition. Obstruction is one of the most common disorders afflicting the small bowel (Sarraf-Yazdi & Shapiro 2010) and is more common because the ileum is the narrowest segment, and therefore more easily obstructed. Obstruction of the large bowel tends to develop more slowly and is associated with a high mortality rate (Biondo et al. 2004). The most common cause of small bowel obstruction is post-operative adhesions, with hernias being the second most common cause (Baker et al. 2009). Adhesions are bands of scar tissue following inflammation which can constrict the intestine. Other causes of bowel obstruction are:
• volvulus – twisting of bowel more common in the elderly
• intussusception – segment of intestine prolapsed into an adjacent part, usually in infants
• mesenteric embolus – interferes with blood supply, foreign bodies (e.g., drug smugglers swallowing packages), faecal impaction, tumours
• paralytic ileus – peristalsis may be interrupted by disturbance of the nerve supply following peritonitis, pancreatitis, shock, spinal cord lesions, or after abdominal surgery
Pathophysiology
Obstruction of the bowel causes fluid, gas and air to collect near the obstruction site. The bowel tries to force its contents past the obstruction by increasing peristalsis. This causes damage to the intestinal mucosa, which results in further swelling at the site. This increased pressure exceeds venous and capillary pressure, causing reduced blood supply to the bowel. As the bowel wall swells, instead of performing its normal function in this area, it starts to secrete water, sodium and potassium, leading to dehydration. Gas-forming bacteria collect in the area and aggravate distension by fermentation, which produces more gas. If untreated, the interruption of the blood supply to the bowel will lead to gangrene, perforation of the bowel and peritonitis. Patients who develop septicaemia in these cases have a 70 % mortality rate (Herrington 2009).
Assessment
Obstruction of the small bowel is commonly associated with sudden onset of colicky abdominal pain radiating over the whole abdomen. Appendicitis is characterized by a dull pain in the right lower quadrant, accompanied by an elevated temperature. The pain of pancreatitis is constant, not colicky, and the pain of diverticulitis usually occurs in the left lower quadrant and may be accompanied by blood in the faeces (Herrington 2009). In large bowel obstruction, the pain has a more gradual onset. In small bowel obstruction there is vomiting of gastric juice, mucus and bile in high obstructions. If the obstruction is in the ileum or large bowel, the patient may vomit faecal contents. This loss of fluid by vomiting and increased intestinal secretion leads to severe dehydration and electrolyte imbalance. The extravasation of plasma from the capillaries adds to the accumulation of fluid in the intestines, which compresses the veins, reducing venous return and contributing to the shock.
Clinical, laboratory, and radiographic factors should all be considered when making a decision about treatment of small bowel obstruction. The four clinical features, intraperitoneal free fluid, mesenteric oedema, lack of the ‘small bowel faeces sign’ and history of vomiting are predictive of requiring operative intervention (Zielinski et al. 2010). The small bowel faeces sign is a finding that can be observed on CT scan and is defined by the presence of particulate feculent matter mingled with gas bubbles in the lumen of dilated loops of the small intestine.
Investigations
Blood should be sent for full blood count, electrolytes, amylase, glucose and cross-match. A raised white cell count can be an indicator of infection, which can suggest perforation or even ensuing sepsis and possible bacterial translocation as the gut becomes so distended that the bowel contents are able to pass through its membranes. Abdominal radiographs in both the supine and upright positions may reveal bowel distortion and distension, with air or fluid levels, however during the past two decades, computed tomography has become a mainstay in the evaluation of patients with known or suspected small bowel obstruction. Computed tomography scans should be performed and interpreted with attention to establishing the diagnosis of small bowel obstruction, locating the transition point indicating the site of obstruction, and determining the cause of the obstruction (Desser & Gross 2008, Zielinski et al. 2010).
Management
Strategies for the management of small bowel obstructions have changed significantly over the years. Non-operative medical management has become the mainstay of treatment of many small bowel obstructions. However, the key to the management of small bowel obstructions is identifying those patients who need surgical intervention (Trevino 2010). The most life-threatening problem for the patient is fluid volume deficit and therefore the initial priorities are to treat the shock due to the hypovolaemia and to prevent further complications (Diaz et al. 2008
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree