Supraventricular Tachycardia
John L. Sapp Jr
Laurence M. Epstein
I. BACKGROUND
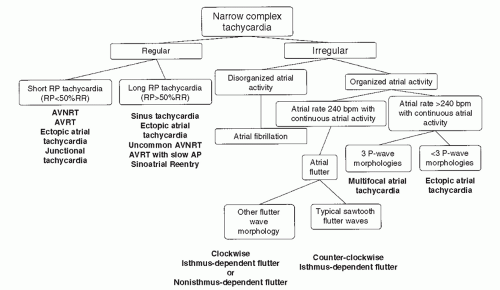
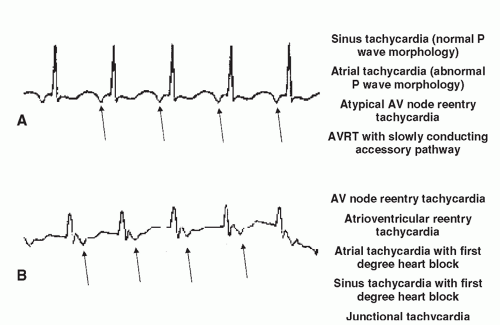
A. Definition: Supraventricular tachycardias are those arrhythmias that require involvement of the atrioventricular (AV) node or atria for their perpetuation. They are usually described by mechanism or by their electrocardiographic appearance (Figs. 36-1 and 36-2).
II. MECHANISMS: There are two main mechanisms underlying supraventricular tachycardias.
A. Focal Arrhythmias: for example, inappropriate sinus tachycardia, ectopic atrial tachycardia, atrial premature beats, multifocal atrial tachycardia.
B. Reentry: for example, atrioventricular reentrant tachycardia (AVRT), atrioventricular nodal reentrant tachycardia (AVNRT), atrial flutter.
III. RECOGNITION AND DIAGNOSIS (see Figs. 36-1 and 36-2). It should be noted that rate or hemodynamic stability does not predict the tachycardia mechanism. Rapid, poorly tolerated rhythms can be SVT, and slower, well-tolerated rhythms can be ventricular tachycardia (VT).
A. QRS is >120 ms (wide complex tachycardia).
1. Supraventricular activation with aberrancy or preexcitation (over an accessory AV pathway) will result in a wide complex tachycardia. This must be distinguished from ventricular tachycardia.
2. The presence of a history of significant structural heart disease or a QRS morphology atypical for bundle branch block increases the likelihood of VT. Consultation should be sought.
B. QRS duration <120 ms in all surface leads: likely supraventricular.
C. Irregularly irregular QRS complexes most commonly signify atrial fibrillation (multifocal atrial tachycardia is distinguished by the presence of P waves with at least three different morphologies).
D. Irregularly irregular rhythm with wide/varying QRS width may suggest atrial fibrillation with ventricular preexcitation over an accessory pathway (AP) (this is uncommon).
E. Atrial activity.
1. The P waves may be buried in the QRS-T complex. If possible, compare to sinus rhythm tracings to look for subtle manifestations of atrial activation (r′ in lead V1 or small S wave in inferior leads).
2. Organized continuous atrial activity >240 beats/min is classified as atrial flutter. Typical atrial flutter: downsloping flutter waves in the inferior leads followed by a rapid upstroke, short positive P waves in V1, and an atrial rate of approximately 300 beats/min. Atypical flutter circuit or ectopic atrial tachycardia may have a different morphology or atrial rate.
3. If every P wave is not associated with a QRS (i.e., AV block is present), the tachycardia is unlikely to depend on the AV node. Differential diagnosis: ectopic atrial tachycardia, atrial flutter, can very rarely be seen with AVNRT.
4. Is there a 1:1 relationship between P and QRS deflections? (See Fig. 36-2.) Is there a long RP (RP > PR) tachycardia (differential diagnosis: ectopic atrial tachycardia, sinus tachycardia, less commonly AVRT utilizing a slowly conducting bypass tract or atypical AVNRT) or a short RP tachycardia (RP < PR; differential diagnosis: AVNRT, AVRT, junctional tachycardia, or ectopic atrial tachycardia)?
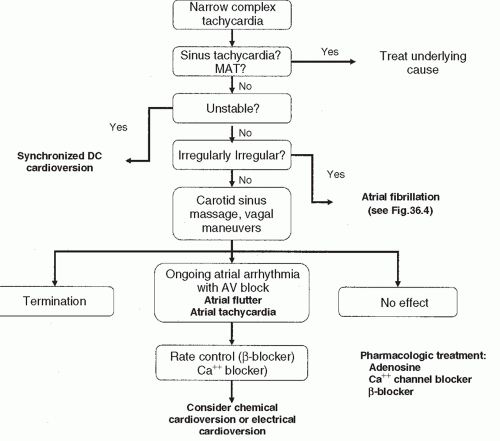
IV. GENERAL MANAGEMENT OF SUPRAVENTRICULAR TACHYCARDIAS: A general approach to the evaluation and management of supraventricular tachycardias is outlined in Figure 36-3.
A. Assess patient stability.
B. Identify sinus tachycardia or multifocal atrial tachycardia if present: Treat the underlying causes and control heart rate.
C. If unstable: Prompt direct current (DC) cardioversion.
1. Electrical cardioversion should be synchronized. Atrial flutter and other SVTs are usually terminable with a single 50- to 100-J countershock. Atrial fibrillation often requires 200 to 360 J.
D. Stable patients.
1. Vagal maneuvers: carotid sinus massage or a Valsalva maneuver (can also be diagnostic by causing transient AV block unmasking P or flutter waves).
2. Adenosine: 6 to 12 mg, rapid IV push, followed by immediate saline flush. Carbamazepine and dipyridamole potentiate the actions of adenosine and may prolong its action causing angina or bronchospasm. Methylxanthines (caffeine, theophyllines) antagonize the effects of adenosine and may render it ineffective. Consider lower dose if administered centrally or in heart transplant recipients.
3. IV verapamil, diltiazem, or β-blockers may be used (Table 36-1). Vagal maneuvers may be repeated in the presence of drug therapy and may act synergistically.
4. Atrial flutter, atrial tachycardia, and atrial fibrillation are unlikely to terminate with these measures, although flutter waves or ectopic P waves may be unmasked, facilitating diagnosis.
5. Type I or type III antiarrhythmic agents may be used for conversion alone or in combination with DC cardioversion.
V. SPECIFIC ARRHYTHMIAS AND THERAPIES
A. Atrial fibrillation.
1. Atrial fibrillation is the most common supraventricular tachycardia and has chaotic activation of the atria (Fig. 36-4F).
2. Acute treatment (Fig. 36-5).
a. Is the patient stable?
b. Unstable: Synchronized direct current cardioversion is the treatment of choice. Atrial fibrillation may be difficult to convert and require higher energies than other arrhythmias.
c. Stable: pharmacologic rate control.
i. β1-Selective adrenergic receptor antagonists remain first-line therapy in nonasthmatic patients.
ii. Non-dihydropyridine calcium channel blockers (e.g., verapamil, diltiazem).
iii. Digitalis may be used with relative safety in patients with poor ventricular function but provides only modest control of ventricular rate. It is ineffective in patients with high adrenergic tone or when very prompt rate control is required.
TABLE 36-1 Drugs for Supraventricular Tachycardias | ||||||||
|---|---|---|---|---|---|---|---|---|
|