Sudden Unilateral Neuralgiform Pain with Conjunctival Injection and Tearing
Manjit S. Matharu
Peter J. Goadsby
SHORT-LASTING UNILATERAL NEURALGIFORM HEADACHE ATTACKS WITH CONJUNCTIVAL INJECTION AND TEARING
International Headache Society (IHS) code and diagnosis: 3.3 Short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT)
World Health Organization (WHO) code and diagnosis: This syndrome is not recognized in the current edition of the International Classification of Disease (ICD).
Short description: This syndrome is characterized by strictly unilateral, severe, neuralgic attacks centred on the ophthalmic trigeminal distribution that are brief in duration and very often occur in association with prominent lacrimation and redness of the ipsilateral eye.
Previously used terms: None.
EPIDEMIOLOGY
Short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT) syndrome was first described relatively recently in 1978 (64). Since then 82 cases (64 primary or idiopathic, 18 secondary or symptomatic cases) have been reported in the English language literature. The prevalence and incidence of SUNCT are not known, though the extremely low number of reported cases suggests that it is a very rare syndrome. Primary SUNCT has a slight male predominance (35 males, 29 females) with a sex ratio of 1.2:1. In an earlier review of SUNCT syndrome the male predominance among primary cases was greater than that reported here, with a sex ratio of 3.75 (15 males, 4 females) (52). The trend toward decreasing male:female ratios over time probably reflects an ascertainment issue. The typical age of onset is between 35 and 65 years (69% of primary SUNCT cases), though it ranges from 10 to 77 years (mean 50 ± 15 years) (36).
PATHOPHYSIOLOGY
The trigeminal autonomic cephalgias (TACs) are a group of primary headache disorders characterized by unilateral trigeminal distribution pain that occurs in association with ipsilateral cranial autonomic features (17). The group comprises SUNCT, paroxysmal hemicrania (PH), and cluster headache (CH). Any pathophysiologic construct for TACs must account for the two major clinical features characteristic of the various conditions that comprise this group: trigeminal distribution pain and ipsilateral autonomic features. The pain-producing innervation of the cranium projects through branches of the trigeminal and upper cervical nerves to the trigeminocervical complex, from which nociceptive pathways project to higher centers. This implies an integral role for the ipsilateral trigeminal nociceptive pathways in TACs. The ipsilateral autonomic features suggest cranial parasympathetic activation and sympathetic hypofunction. Goadsby and Lipton have suggested that the pathophysiology of the TACs revolves around the disinhibition of the trigeminal-autonomic reflex (17). There is considerable experimental animal literature to document that stimulation of trigeminal afferents can result in cranial autonomic outflow, the trigeminal-autonomic reflex (44). In fact, some degree of cranial autonomic symptomatology is a normal physiologic response to cranial nociceptive input (16,43) and patients with other headache syndromes may report these symptoms (1,3,6). The distinction between the TACs and other headache syndromes is the degree of cranial autonomic activation (18).
Cranial autonomic symptoms are likely to be prominent in the TACs due to a central disinhibition of the
trigeminal-autonomic reflex (18). Supporting evidence is emerging from functional imaging studies: a functional magnetic resonance imaging (fMRI) study in SUNCT (42) (see Fig. 98-1) and a positron emission tomography (PET) study in CH (41) have both demonstrated ipsilateral hypothalamic activation. Hypothalamic activation is specific to these syndromes and is not seen in migraine (2,71) or experimental ophthalmic trigeminal distribution head pain (45). There are direct hypothalamic-trigeminal connections (34) and the hypothalamus is known to have a modulatory role on the nociceptive (10,70) and autonomic pathways (33). Hence, SUNCT is possibly due to an abnormality in the hypothalamus, with subsequent trigeminovascular and cranial autonomic activation.
trigeminal-autonomic reflex (18). Supporting evidence is emerging from functional imaging studies: a functional magnetic resonance imaging (fMRI) study in SUNCT (42) (see Fig. 98-1) and a positron emission tomography (PET) study in CH (41) have both demonstrated ipsilateral hypothalamic activation. Hypothalamic activation is specific to these syndromes and is not seen in migraine (2,71) or experimental ophthalmic trigeminal distribution head pain (45). There are direct hypothalamic-trigeminal connections (34) and the hypothalamus is known to have a modulatory role on the nociceptive (10,70) and autonomic pathways (33). Hence, SUNCT is possibly due to an abnormality in the hypothalamus, with subsequent trigeminovascular and cranial autonomic activation.
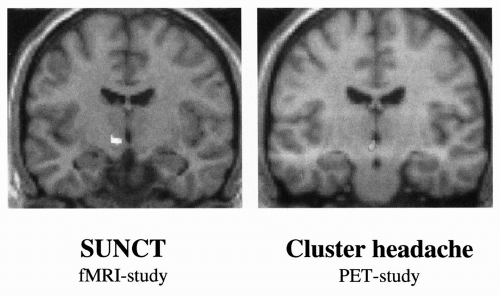 FIGURE 98-1. Blood oxygen level dependent functional magnetic resonance imaging (BOLD fMRI) study demonstrating posterior hypothalamic activation during spontaneous pain attacks in a SUNCT patient. (Reused from May A, Bahra A, Buchel C, et al. Functional magnetic resonance imaging in spontaneous attacks of SUNCT: short-lasting neuralgiform headache with conjunctival injection and tearing. Ann Neurol 1999;46:791-794.) (See color plate) |
Several studies have demonstrated the diverse parasympathetic manifestations of SUNCT. Forehead sweating is usually increased during bouts (28), unlike PH, in which it is normal. Pupillary studies using pupillometry and pharmacologic approaches have revealed no abnormalities (73). Since conjunctival injection occurs during SUNCT, it is not surprising that intraocular pressure and corneal temperatures are elevated during attacks (67), most likely reflecting local vasodilation consequent to the marked parasympathetic activation. Similarly, a report of bradycardia in association with attacks of SUNCT indicates increased parasympathetic outflow (27). Systolic blood pressure is sometimes elevated, although ventilatory function is normal (26).
Orbital phlebography is reported to be abnormal in SUNCT syndrome, with a narrowed superior ophthalmic vein and the cavernous sinus homolateral to the pain (29). This finding leads to the suggestion that SUNCT syndrome may be a form of orbital venous vasculitis (20), although there are similar reports in CH, Tolosa-Hunt syndrome, and PH (17). However, transcranial Doppler and SPECT (single photon emission computed tomography) studies have not demonstrated convincing change in the vasomotor activity (63) or cerebral blood flow during attacks of pain (55). Similarly, no intracranial vessel activation was apparent in an fMRI study (42). The hypothalamic activation and the diverse parasympathetic manifestations taken together with the paucity of evidence for vascular changes favor a central pathogenesis for SUNCT rather than a peripheral vasculitic cause.
CLINICAL FEATURES
Site of Pain
The pain is usually maximal in the ophthalmic distribution of the trigeminal nerve, especially the orbital or retro-orbital regions, forehead, and temple. It may radiate to the other ipsilateral trigeminal divisions and, rarely, even to extratrigeminal regions such as the ear and occiput.
Laterality of Attack
The attacks are typically strictly unilateral and side-locked; however, in four patients the pain was simultaneously experienced on the opposite side (52,60), while three patients reported strictly unilateral but side-alternating attacks (11,12,39). The pain is present more frequently on the right side than the left in patients with side-locked attacks (36).
Severity of Pain
The intensity of the pain is generally severe. The usual pain intensity was described as moderate in 14% of patients, severe or intense in 63% of patients, and very severe or excruciating in 23% of patients (36).
Character of Pain
The pain had a neuralgic character in the majority of patients (85%), being usually described as stabbing, sharp, burning, pricking, piercing, shooting, lancinating, or electric shock-like. The character of pain has also been described as pulsatile or throbbing (6%), steady (4%), spasmodic (2%), staccato (2%), and pressing (2%) (36).
Duration of the Individual Attack
Three different types of pain have been described in SUNCT syndrome: relatively short-lasting attacks; long-lasting attacks; and a continuous or intermittent background ache.
The individual short-lasting attacks are very brief, lasting between 5 and 120 seconds in the majority of patients (84%). The attacks were described as lasting less than
5 seconds in 8% of patients and more than 120 seconds in 8% of patients. The median duration of the usual attack was 40 seconds. The range of the usual attack duration was between 2 seconds and 20 minutes (7,11,36,39). In a study that objectively measured the duration of 348 attacks in 11 patients, the range of duration was 5 to 250 seconds and the mean duration was 49 seconds (50).
5 seconds in 8% of patients and more than 120 seconds in 8% of patients. The median duration of the usual attack was 40 seconds. The range of the usual attack duration was between 2 seconds and 20 minutes (7,11,36,39). In a study that objectively measured the duration of 348 attacks in 11 patients, the range of duration was 5 to 250 seconds and the mean duration was 49 seconds (50).
There are four reported cases of SUNCT syndrome in which prolonged attacks, lasting 1 to 2 hours, are described (37,42,49). In all these patients, the majority of the attacks were short-lasting and were otherwise typical for SUNCT syndrome; the relatively long-lasting attacks were phenotypically similar to the short-lasting attacks except for the duration of the attack.
Most patients are completely pain free between attacks, although there are seven case reports of a dull interictal ipsilateral discomfort over the same site; the interictal discomfort has been reported to be continuous in five cases (7,39,52,60) and intermittent in the other two (62,69). There is also one case report of a bilateral continuous interictal discomfort over the forehead (39). In addition, a burning sensation lasting 2 hours following the attacks has also been reported (57).
Temporal Profile of the Individual Attack
The short-lasting paroxysms begin abruptly, reaching the maximum intensity within 2 to 3 seconds (52). In the majority of patients, the pain is maintained at the maximum intensity before abating rapidly. However, several temporal patterns for the individual attack, besides the plateau-like pattern, have been described, including a repetitive pattern of spike-like paroxysms; a saw-tooth pattern in which repetitive spike-like paroxysms occur without reaching the pain-free baseline between the individual spikes; and plateau-like plus exacerbations pattern in which a plateau-like attack had superimposed, random, ultrashort exacerbations of 1 to 2 seconds (51) (Figure 98-2).
Frequency and Periodicity of Attacks
Both episodic and chronic forms of SUNCT exist (36). In the majority of patients, SUNCT syndrome presents in an episodic manner; the temporal pattern is quite variable, with the symptomatic periods alternating with remissions in an erratic manner. Symptomatic periods generally last from a few days to several months and occur once or twice annually, although a maximum of 22 bouts per annum have been reported (52). Remissions typically last a few months, though they can range from 1 week to 8.5 years (24). Symptomatic periods appear to increase in frequency and duration over time (52). Circannual periodicity is not typically a feature of SUNCT.
In 28% of patients the disorder is chronic, with the symptomatic period lasting more than 1 year. In these cases the mean duration of the chronic phase was 5.3 ± 5.0 years (range: 1 to 17 years). In the majority of these patients the disorder is chronic from onset (72%), though in some the chronic form develops from the episodic variety (28%) (36). In addition, there are several case reports of SUNCT syndrome in which the chronic phase alternates with the episodic phase (5,20,21,65). Earlier reviews noted that the chronic form of SUNCT was not sufficiently validated (53). The chronic form of SUNCT is now sufficiently validated and, therefore, the subclassification of SUNCT syndrome should include episodic and chronic forms, thereby bringing it in line with that of cluster headache and paroxysmal hemicrania.
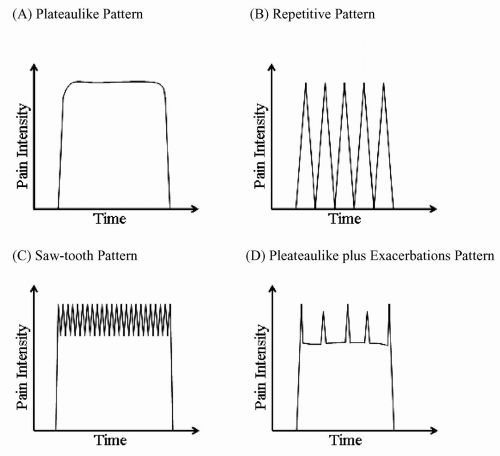 FIGURE 98-2. Temporal profile of SUNCT attacks: (A) plateau-like pattern: rapid onset of pain, which is maintained at maximum intensity before abating rapidly; (B) repetitive pattern of spike-like paroxysms; (C) saw-tooth pattern in which repetitive spike-like paroxysms occur without reaching the pain-free baseline between the individual spikes; and (D) plateau-like plus exacerbations pattern in which a plateau-like attack had superimposed, random exacerbations (adapted from ref. 41). |
The attack frequency during the symptomatic phase varies immensely between sufferers and within an individual sufferer. Attacks may be as infrequent as once a day or less to more than 60 per hour (46). Objective assessment of the frequency of attacks in four patients demonstrated a mean of 16 attacks daily with a range of 1 to 86 attacks daily (50). There are six case reports of a SUNCT-like status, when patients experience severe exacerbations with frequent, easily triggered, high-intensity pain attacks in a repetitive and overlapping fashion for several hours or days at a time (21,46,52).
SUNCT attacks occur either exclusively or predominantly during the daytime. Exclusively diurnal attacks were reported in five (17%) patients. Nocturnal attacks
were reported to occur occasionally in 20 (66%) patients and frequently in 5 (17%) patients. However, these results need to be interpreted cautiously as no data were available in over half of the reported cases (34 patients; 53%). Objective assessment of the timing of 585 attacks in four patients demonstrated that a bimodal distribution occurs with morning and afternoon/evening predominance, with only 1.2% occurring at night; however, given the small number of patients studied these data need to be interpreted cautiously (50).
were reported to occur occasionally in 20 (66%) patients and frequently in 5 (17%) patients. However, these results need to be interpreted cautiously as no data were available in over half of the reported cases (34 patients; 53%). Objective assessment of the timing of 585 attacks in four patients demonstrated that a bimodal distribution occurs with morning and afternoon/evening predominance, with only 1.2% occurring at night; however, given the small number of patients studied these data need to be interpreted cautiously (50).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








