Oxford Help pillow.
What will be your anaesthetic technique?
Thorough preoperative assessment is required. A cardiorespiratory referral and investigations or continuous positive airway pressure (CPAP) for obstructive sleep apnoea (OSA) may be needed. Routine bloods and a preoperative ECG should be requested. Difficult intubation may be encountered although obesity alone is not a predictor for this; other signs, e.g. large neck circumference, and a Mallampati score ≥3 are also required. A supine position may lead to airway obstruction and desaturation so awake intubation in a sitting position may be better tolerated in some patients. Minimize the time between induction and ventilation to avoid desaturation. Tracheal intubation is required and positive end-expiratory pressure (PEEP) should be used. A reverse Trendelenburg position is safe as long as patients are carefully secured to the table. This position may also improve respiratory compliance. Use calf compression devices for thromboprophylaxis. Antibiotic prophylaxis is important as post-operative wound infection is more common in obese patients. Consider using prokinetics and antacids. Short-acting anaesthetic agents, e.g. remifentanil, sevoflurane or desflurane, help achieve rapid recovery and minimize post-operative hypoxaemia and hypoventilation. Reversal of neuromuscular block is essential; extubation and recovery should be in a head-up position. Pharmacokinetics are significantly affected by obesity. Drug dosing can be based on lean, ideal (height in cm minus 100 for men and 105 for women) or actual body weight. The Society for Obesity and Bariatric Anaesthesia (SOBA) have produced guidelines to assist drug dosage, which are part of their incredibly helpful single sheet guide, which can be found in Figure 20.2.
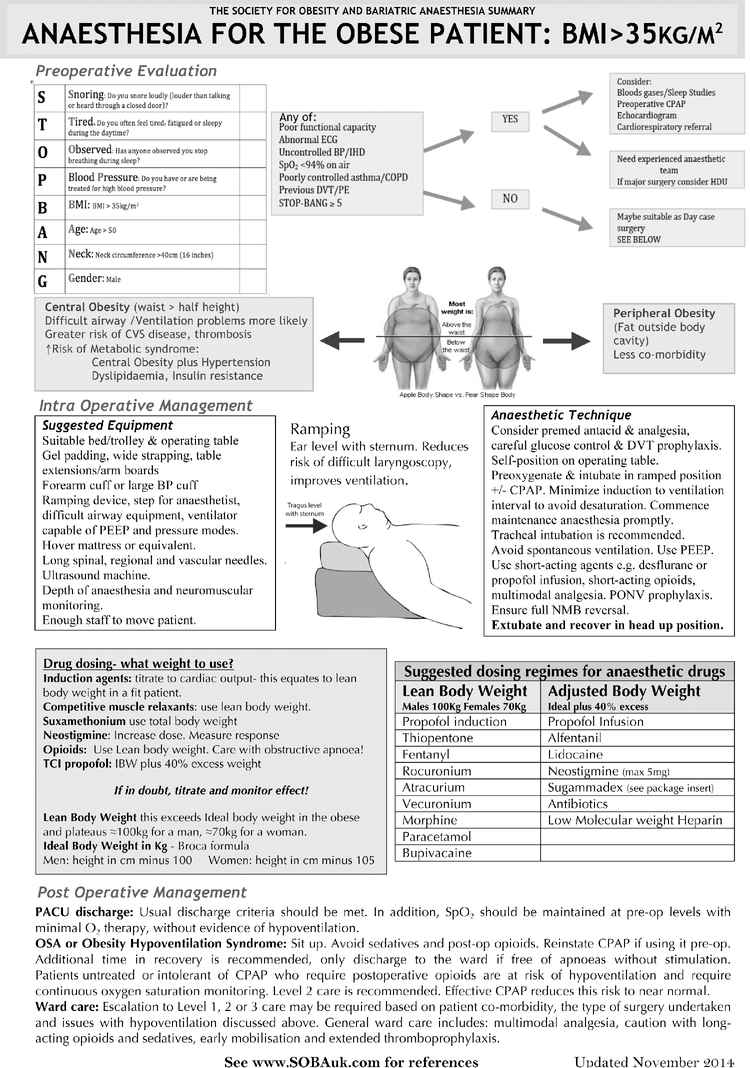
SOBA Single Sheet Summary; Anaesthesia for the Obese Patient.
What are the post-operative considerations?
Patients with obesity-related co-morbidities have a greater risk of perioperative complications. Early mobilization reduces atelectasis and thromboembolism. Thromboprophylaxis should be started and continued post-operatively. This patient may require level 2 care in view of his co-morbidities. Adopt a multimodal approach to analgesia and avoid long-acting opioids where possible. If OSA is diagnosed he may require post-operative CPAP or continuous oxygen saturation monitoring.
Further reading
Cardiothoracics: double lumen tube (DLT) management
You are anaesthetizing a patient for a right-sided upper lobectomy using a left-sided DLT. The patient is in the left lateral position. A few minutes after commencing surgery the patient’s oxygen saturations fall to 88%.
What are the indications for use of a DLT?
Indications for use of a double lumen tube
| Absolute | Relative |
|---|---|
Lung isolation to avoid contamination:
| Non-thoracic surgical access:
|
Control of distribution of ventilation:
| Surgical access:
|
Unilateral bronchopulmonary lavage:
| Severe hypoxaemia due to unilateral lung disease |
Most modern DLTs are based on Robertshaw’s design (39–41Fr or medium/large for men and 35–37Fr or small/medium for women). A left-sided DLT is used more commonly because of the lower risk of obstructing the right upper lobe bronchus. The bronchial cuff of a right-sided DLT incorporates a side window for ventilating the right upper lobe.
The correct position of the DLT is confirmed by visual inspection, auscultation and fibre-optic bronchoscopy:
1. Inflate tracheal cuff and confirm ventilation of both lungs.
2. Usual insertion depth is 29 cm at teeth for patient of 170 cm height (+/−1 cm for every 10 cm change in height).
3. Confirm one-lung ventilation (OLV) via the bronchial lumen and inflate bronchial cuff. (If requires >4 ml air the DLT is malpositioned or too small.)
4. Confirm OLV via the tracheal lumen.
5. Confirm positioning of bronchial cuff (blue) just below level of carina with a bronchoscope.
6. If using a right-sided DLT confirm that side window of bronchial lumen is aligned with right upper lobe bronchus.
7. If moving patient to lateral position reconfirm adequacy of OLV and position of DLT bronchoscopically once positioned.
How would you manage hypoxaemia during one-lung ventilation (OLV)?
Ventilate patient’s lungs with 100% oxygen prior to OLV. Then ask yourself the following questions.
1. Is there a problem with oxygen delivery?
Check anaesthetic machine and breathing circuit.
Ventilate with 100% oxygen.
2. Is the airway pressure high or has it increased?
Check the position of the DLT with bronchoscope.
Suction to remove any sputum or blood.
Signs of bronchospasm? Give bronchodilators if needed.
Adequate paralysis?
Is there air trapping and hyperinflation? Decompress by disconnecting breathing circuit from DLT.
Is there a pneumothorax of the ventilated lung? Decompress with surgical assistance if required.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





