Hemorrhagic Intra-Cranial & Aneurysms (10%):
Link: Risks | Intraparenchymal / Intracerebral | Hematoma (Subdural / Epidural) | Subarachnoid Hemorrhage & Intracranial aneurysm |
Intracranial hemorrhage (ICH) is from rupture of a vessel anywhere within the cranial cavity. Sudden onset, have a hyperdense mass (blood) on CT, along with N/V, altered MS.
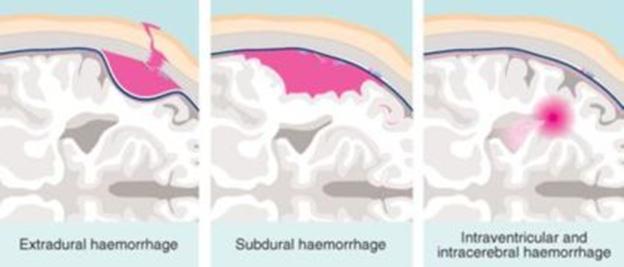
Location: Classify by location (extradural, subdural, subarachnoid, intracerebral, intraventricular) and type of vessel (arterial, capillary, venous).
Intracranial Hematoma:
 For more details see Neurology chapter (strokes). Of pt’s presenting to the emergency department with head injury and a GCS of 15, 6-8% have an intracranial abnormality.
For more details see Neurology chapter (strokes). Of pt’s presenting to the emergency department with head injury and a GCS of 15, 6-8% have an intracranial abnormality.
Subdural/ epidural. All types need prompt surgical evacuation.
Epidural (extradural): Most from minor trauma, usually from a temporal skull fx (80%) rupturing the middle meningeal artery running along the inside of the skull, may cause minimal brain injury. Present after traumatic LOC, then 1-2hr lucid interval, then obtundation (“talk and die”), ipsilateral pupillary dilation. Need urgent operative decompression. Sx’s relieved when clot is evacuated and pressure relieved.
Acute Subdural: Most from severe trauma, usually have marked brain injury from the shearing force that injures the bridging vein or tears a parenchymal vessel in the deep space of the dura. The blood does not cross the sinuses (in contrast with epidural) Can be spontaneous. Mortality is 60% untreated, 30% surgically repaired in <4hrs. Seizure prophylaxis with phenytoin 1g IV. For herniation may need burr hole placement to relieve incr ICP preferably done by neurosurgery or physicians trained in trephination.
Subacute & Chronic Subdural: 72hr-3wks, usually elderly with trivial trauma. Presents with H-A, confusion, language difficulties or TIA-like sx’s.
Intracerebral hematoma: direct rupture of an intrinsic cerebral vessel, bleeds directly beneath the injury or on opposite side if from a contrecoup injury. Not the same as intracerebral hemorrhage from a HTN bleed.
Causes of Intracranial Hemorrhage: Includes Intracerebreal, Subarachnoid, Ventricular and Subdural bleeds.
1. Primary (hypertensive) intracerebral hemorrhage
2. Ruptured saccular aneurysm.
3. Ruptured arteriovenous malformation; less often, venous and dural vascular malformations.
4. Cavernous angioma.
5. Trauma including posttraumatic delayed apoplexy.
6. Hemorrhagic disorders: leukemia, aplastic anemia, thrombocytopenic purpura, liver disease, complication of anticoagulant or thrombolytic therapy, hypofibrinogenemia, hemophilia, Christmas disease, etc.
7. Hemorrhage into primary and secondary brain tumors.
8. Septic embolism, mycotic aneurysm.
9. With hemorrhagic infarction, arterial or venous.
10. With inflammatory and infectious disease of the arteries and veins.
11. With arterial amyloidosis.
12. Miscellaneous rare types: vasopressor drugs, cocaine, moyamoya, herpes simplex encephalitis, vertebral artery dissection, acute necrotizing hemorrhagic.
Intracerebral (75%, most either basal ganglia, pons or cerebellar) or subarachnoid (25%). 40% in the basal ganglia, 25% in the subcortical white matter, 20% in the thalamus, 15% in the cerebellum, 5% in the pons.
• An observational study suggests no difference in seizure rates with invasive (surgery, embolization, or stereotactic radiosurgery) vs. conservative management of AVMs according to a 9-year prospective observational study of 219 patients with brain AVMs (Neurology 2012;79:500). Even among those who had presented with a seizure, the risk for recurrent seizures was not significantly different after invasive versus conservative treatment (67% vs. 72%). Nor did rates differ according to whether the AVM was obliterated.
Risks: 80% are due to HTN & cerebrovascular dz, which causes degeneration of the media of the arterial wall. Aspirin use is not considered a major risk factor. 28% could be prevented if all hypertensive pt’s were to receive tx (Stroke 2004;35:7642), giving a savings of about $2.5 billion/yr in the USA.
• Independent risk factors for intracerebral hemorrhage (ICH) include HTN (adjusted odds ratio 5.71), diabetes (OR, 2.40), menopause (OR, 2.50), and current cigarette smoking (OR, 1.58), >2 alcoholic drinks per day (OR, 2.23), more >5 caffeinated drinks per day (OR, 1.73) (Stroke 2005;36:1881-1885). Regular use of moderate doses of aspirin (median dose 250 mg) preceding the stroke is a significant independent predictor of death in the first 3 mo’s after the event (2.5-fold risk) (Stroke 2006;37:4-5,129-133) (study with 208 pt’s with ICH).
• Analysis of 53,761 person-years in pt’s with a history of TIA or minor ischemic stroke, an increased risk of intracerebral hemorrhage is predicted by older age, high blood pressure, and use of antihypertensive medication (J Neurol Neurosurg Psychiatry 2006;77:92-94).
• Researchers found a significant decline in ICH incidence in pt’s younger than 75 and an insignificant increase in ICH incidence in those 75 or older in the past 20 years (Lancet Neurol 2007;6:757)…..The decline in the younger group was associated with a decreased number of cases related to improvements in the detection and management of hypertension; the increase in the older group was associated with an increased number of cases related to antithrombotic treatment and, probably, from the increased prevalence of cerebral amyloid angiopathy in the elderly….careful consideration of the indications and risk-to-benefit ratio for warfarin use in the elderly might reduce the incidence of ICH in this population. With increasing blood pressure, the risk of both ischemic and hemorrhagic stroke increases, but the most marked effect of high blood pressure is on the risk of nonlobar primary intracerebral hemorrhage (PICH) (Stroke 2007;38:2681-2685).
• A 10 years of follow-up in the ongoing, population-based Rotterdam Study shows that a low GFR is associated with a more than 4-fold increase in risk of hemorrhagic stroke — but not ischemic stroke (Stroke 2007;38:3127-3132) (HR = 4.10)….two possible explanations: may be a marker of cerebral small vessel disease or that low GFR causes platelet dysfunction. In patients with hypertension, brain microbleeds are associated with higher ambulatory blood pressures according to an MRI study (Hypertension 2008;51:62-68).
• The use of antiplatelet medications (aspirin or clopidogrel) at intracerebral hemorrhage onset has no association with increased hemorrhage, enlargement of the area of hemorrhage or on outcome (Neurology 2009;72:1397-1402)…..”should not be considered at higher risk of having a bad outcome, and should not be given platelet transfusions because of the aspirin or clopidogrel.” History of head trauma and hematuria was associated with higher risk for intracranial hemorrhage in children with ITP (Blood 2009;114:4777)……Combining hematuria with head trauma identified 53% of patients with ICH…..Death occurred in 25% of those with ICH, and 33% experienced neurological sequelae (median follow-up, 11 months).
• With Vitamin E supplements lower the risk (10% lower) for ischemic stroke but raise the risk for hemorrhagic stroke (22% higher) and thus widespread use of vitamin E supplements is not recommended according to a meta-analysis of randomised controlled trials (BMJ 2010;341:c5702)…..476 people would need to take vitamin E for at least 1 year to prevent one ischemic stroke, and 1250 people would need to take vitamin E to cause one hemorrhagic stroke.
Infrascanner Model 1000: A bedside hand-held scanner FDA approved in 12/2011 to help diagnose intracranial hematomas. By directing near-infrared light (which can penetrate bone) into the skull, it can detect characteristic differences in optical density that could signal intracranial bleeding. The data are transmitted wirelessly to a hand-held computer. Clinicians can use this information to help determine whether brain imaging is warranted. Compared with CT, the device has a sensitivity of 75% and a specificity of 82% for detecting intracranial blood. This device offers emergency room physicians a noninvasive mechanism to aid in assessing whether an immediate CT scan is needed……may allow physicians to avoid or defer CT for low-risk patients.
CT findings suggestion cause: coagulopathy (multiple compartments, fluid levels in the clot), amyloid angiopathy (superficial location, irregular border, recurrent, white matter hypo densities), tumoral (central or eccentric location of hemorrhage, tumor mass visible, proportionally more white matter edema), AVM (calcifications in the hemorrhage mass, enhancement with contrast media).
Asymptomatic incidental cerebral aneurysms: if small (<10mm), pt w/o prior SAH, no “daughter” sac formation (outpouching) or no FHx, observation may be warranted.
Intraventricular Hemorrhage: unilateral ventricle (caudate or thalamic hemorrhage), biventricular (AVM of ependymal lining or choroid, ependymoma, amphetamines), 4th ventricle only (PICA aneurysm), cavum septum pellucidum (anterior artery complex aneurysm).
SBP >230 or DPB >120 mmHg : Nitroprusside @ 0.5-10 mcg/kg/min or NTG drip @10-20ug/min.
SBP 181-230 or DBP 106-120: Labetalol 10mg IV push, repeat or double q 10-20min to max of 300mg.
HTN relative to pre stroke condition: try and approximate premorbid BP.









