Fig. 33.1
SSEP waveforms show P20 and N20 components with phase reversal indicating an electrode overlying the central sulcus signifying the motor and sensory cortex

Fig. 33.2
Draping and planning the incision for the craniotomy approach

Fig. 33.3
Incision for exposure for craniotomy
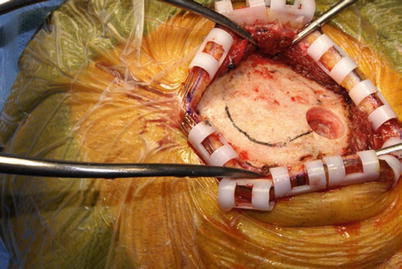
Fig. 33.4
Skull exposure with initiation of craniotomy
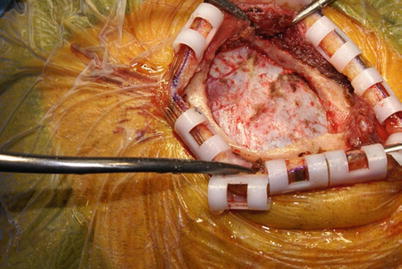
Fig. 33.5
Craniotomy with proper exposure over the central sulcus based on preoperative mapping
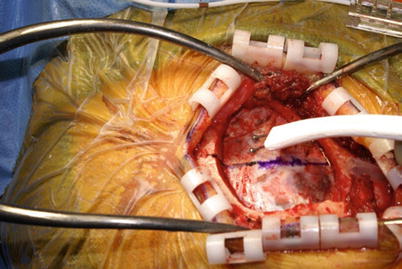
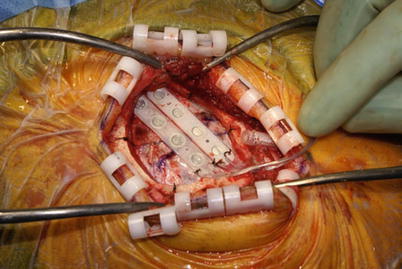
Fig. 33.6
Electrophysiological mapping for lead placement
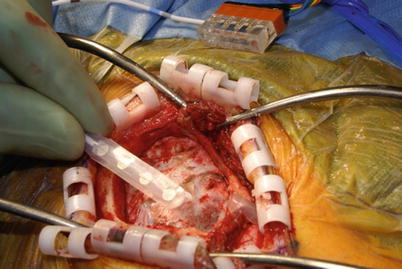
Fig. 33.7
Epidural exposure lead placement
Once the target cortex has been identified using both neuronavigation and electrocortical mapping, two 1 × 4 paddle leads are placed over the previously marked motor and premotor areas that correspond to the contralateral painful area (e.g., face area at the junction of the inferior frontal sulcus and the motor strip). The two leads are placed adjacent to one another and test stimulation is carried out with serial cycling and a slow increase in voltage. Given that no paresthesias are apparent in MCS, one relies on a combination of neurophysiology as well as patient interaction to assess adequate placement of the final electrode position. The patient is awakened from monitored anesthesia. The patient should be able to report good pain relief in the area of pain (e.g., trigeminal distribution on the contralateral side). Stimulation parameters are gradually increased to produce facial twitching and gauge of preseizure threshold, with ice saline available as needed. Once adequate position had been localized over the motor and premotor area, each of the 1 × 4 electrodes is then carefully anchored down with multiple 4-0 Nurolon sutures to the outer layer of the dura. The patient is given further anesthetic to ensure comfort for the remainder of the operation. The leads are tunneled through the posterior bur hole and bone flap is carefully reapplied with titanium plates and screws. Extension wires are then tunneled posteriorly at the level of the parietal boss and attached to two stimulator leads, clearly identifying anterior (premotor) and posterior (motor).
Once the leads are in place, the electrode is connected to trialing cables and an inpatient trial of 3–7 days is carried out. Amplitudes for stimulation vary between 0.5 and 10 V, rate varies from 5 to 130 Hz, and pulse widths vary from 50 to 450 ms. The intensity of stimulation is compared with the motor threshold, with a starting value of 15–20 % of the energy needed to activate the motor components. A typical trial regimen may increase the intensity in 20 % increments up to a maximum level of stimulation that is 80 % of the motor threshold. Because MCS by definition does not elicit paresthesias of the kind commonly perceived in dorsal column or peripheral nerve stimulation, treatment stimulation benefit is tracked through a patient pain diary.
Once the trial is deemed successful, the patient is brought back to the operating room under general anesthesia to undergo generator placement. Most implanters prefer pocketing in the infraclavicular region, although multiple sites are acceptable. A pocket is fashioned for the pulse generator in the plane above the pectoralis fascia. A subcutaneous pouch is made at the area of the parietal boss to accommodate the extension connectors. A tunneling device is used to pass the extension cables in the subcutaneous plane between the parietal incision and the infraclavicular incision. The extension wires are brought through and the motor cortex stimulator leads are connected to the proximal ends of the extensions. Once the connections are secured and tested, both incisions are irrigated copiously and careful closure is performed (Figs. 33.8, 33.9, 33.10, 33.11, and 33.12).