7
Spinal injuries
Introduction
Spinal cord injury (SCI) is one of the most disabling and catastrophic outcomes of injury in a person’s life. The annual incidence of SCI in the UK is about 10–15 per million of the population, with the majority of patients male, usually below the age of 40 years, with a quarter of all cord-injured patients being below the age of 20 (Gallagher 2005). Many of these patients are left with permanent disabilities. The overall physical, emotional and financial consequences of disability are devastating for those injured, and for their families and friends (Zhang et al. 2013). The average Emergency Department (ED) serving a population of 250 000 is likely to receive fewer than four new spinal cord injured patients per year (El Masri 2010). All emergency care clinicians need to be familiar with the initial management of these patients.
Anatomy and physiology
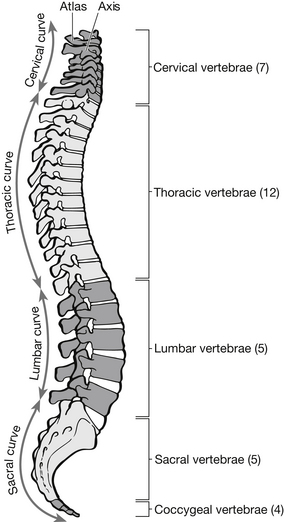
The vertebral column is a series of stacked bones that support the head and trunk and provide the bony encasement for the spinal cord. It comprises 33 vertebrae: 7 cervical (C1–7), 12 thoracic (T1–12), 5 lumbar (L1–5), 5 fused sacral and usually 4 rudimentary coccygeal vertebrae. With the exception of the atlas (C1) and the axis (C2), all vertebrae are anatomically alike but different in size and function (Fig. 7.1).
The spinal cord lies protected within the spinal canal, which is a hollow tunnel extending the length of the vertebral column. The spinal cord descends from the medulla oblongata near the atlas to the level of the second lumbar vertebra. The spinal cord is nearly circular in section and about 1 cm in diameter, with two enlargements. On cross-section, the spinal cord has a grey matter appearing in the form of the letter H. The grey matter consists of nerve cells that act as relay stations for nerve impulses transmitted up and down the spinal cord. White matter surrounds the grey matter and contains longitudinal myelinated fibres organized in tracts or bundles to carry information to and from the brain. Ascending tracts are sensory, and descending tracts are motor (Bickley et al. 2005).
Pathophysiology
The cervical vertebrae are the most mobile part of the spine, so this area is the most frequent site of injury. The rib cage keeps the vertebrae from T1 and T10 stable and relatively immobile. The second most common site of injury is the thoracolumbar junction at T11 to L2. This is a transition area between the rigid thoracolumbar region and the more mobile lumbar region (Semonin-Holleran 2003). Force applied to the cervical spine (c-spine) does not always result in localized vertebral damage, however, because the flexibility of the region and the ability of the neck to move in anteroposterolateral directions, can help transfer the force downwards to the thoracic spine where there is little or no flexibility (Sheerin 2005).
Vertebral column injury, with or without neurological deficits, must always be sought and excluded in a patient with multiple trauma. Any injury above the clavicle should prompt a search for a c-spine injury. Approximately 15 % of patients sustaining such an injury will have an actual c-spine injury. Approximately 55 % of spinal injuries occur in the cervical region, 15 % in the thoracic region, 15 % at the thoracolumbar junction, and 15 % in the lumbosacral area. Approximately 5 % of patients have an associated spinal injury, while 25 % of spinal injury patients have at least a mild head injury (American College of Surgeons 2008).
Approximately 8–10 % of patients with a vertebral fracture have a secondary fracture of another vertebra, often at a distant site. These secondary fractures are usually associated with more violent mechanisms of injury, such as ejection or rollover. Owing to the mechanism of injury, many patients with spinal injury often have other associated injuries, including head, intrathoracic or intra-abdominal injuries, which may alter priorities in management (Lowery et al. 2001). Falls account for 46 %, road traffic accidents (RTAs) account for 34 % and sports-related incidents account for 10 % of spinal injuries in the UK (Harrison 2004). The forces involved in RTAs can cause such severe damage to vertebrae C1 and C2 that the cord is affected, so that the person involved cannot self-ventilate. In such circumstances, death is the most common outcome (Greaves & Porter 2007).
The majority of spinal cord injuries are closed. Table 7.1 outlines the specific categories of movement that may result in spinal cord injury.
Table 7.1
Categories of movement that may result in spinal cord injury
| Category | Mechanism of injury |
| Hyperextension | The head is forced back and the vertebrae of the cervical region are placed in an over-extended position |
| Hyperflexion | The head is forced forward and the vertebrae are placed in an over-flexion position |
| Axial loading | A severe blow to the top of the head causes a blunt downward force on the vertebral column |
| Compression | Forces from above and below compress the vertebrae |
| Lateral bend | The head and neck are bent to one side, beyond the normal range of motion |
| Over-rotation and distraction | The head turns to one side and the cervical vertebrae are forced beyond normal limits |
(After Semonin-Holleran R (2003) Spinal trauma. In: Newberry L, ed. Sheehy’s Emergency Nursing: Principles and Practice, 5th edn. St Louis: Mosby.)
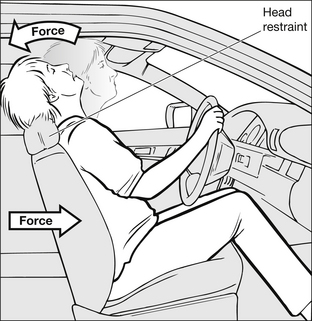
The most common type of injury mechanism is excessive flexion. This usually occurs following RTAs when the patient’s head strikes the steering wheel or windscreen and the spine is forced into hyperflexion with the chin thrown forward to the chest. Rupture of the posterior ligaments results in forward dislocation of the spine (Fig. 7.2).
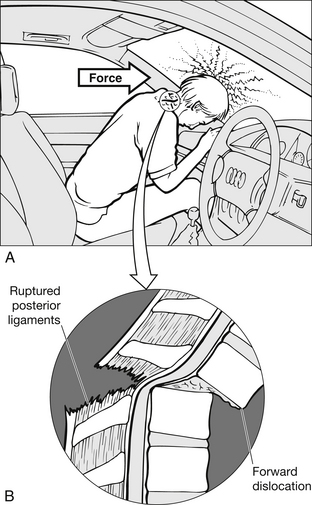
Figure 7.2 Spinal flexion injury. (After Jaworski MA, Wirtz KM (1995) Spinal trauma. In: Kitt S, Selfridge-Thomas J, Proehl JA, Kaiser J, eds. Emergency Nursing: A Physiological and Clinical Perspective. Philadelphia: WB Saunders.)
Axial loading or compression-type injuries can occur when the head strikes an object and the weight of the still-moving body bears against the now stationary head, such as when the head of an unrestrained car passenger is flung into the windscreen or during a dive into shallow water. Vertebral bodies are wedged and compressed, and the burst vertebral fragments enter the spinal canal, piercing the cord (Jaworski & Wirtz 1995) (Fig. 7.3).
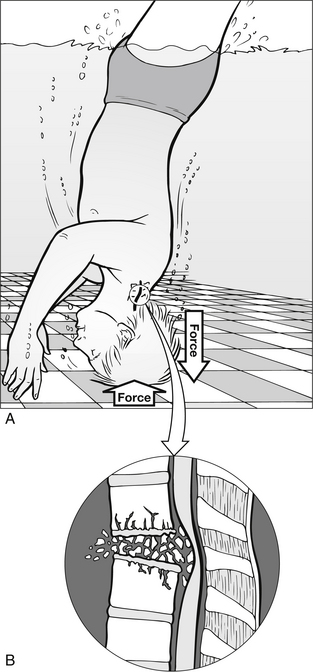
Figure 7.3 Spinal compression injury. (After Jaworski MA, Wirtz KM (1995) Spinal trauma. In: Kitt S, Selfridge-Thomas J, Proehl JA, Kaiser J, eds. Emergency Nursing: A Physiological and Clinical Perspective. Philadelphia: WB Saunders.)
Rotational injuries (Fig. 7.4) can result from a number of causes. Disruption of the entire ligamentous structure, fracture and fracture-dislocation of spinal facets may occur. Flexion-rotation injuries are highly unstable fractures.
Distraction, or over-elongation of the spine, occurs when one part of the spine is stable and the rest is in longitudinal motion. This ‘pulling apart’ of the spine can easily cause stretching and tearing of the cord. It is a common mechanism of injury in children’s playground accidents and in hangings (Pre-Hospital Trauma Life Support Committee 2006).
Patient assessment
The importance of obtaining the patient’s history and establishing the mechanism of injury cannot be overemphasized. Obtaining an accurate history represents 90 % of the diagnosis (American College of Surgeons 2008). A fully documented pre-hospital history should be obtained from the ambulance personnel, police officers and others involved in the pre-hospital phase of patient care. If the patient has been injured as the result of an RTA, digital pictures of the incident scene and the damage sustained to vehicles can provide valuable information about the mechanisms involved. If taken, these photographs should be printed off and included in the patient’s hospital notes (Greaves et al. 2005).
A high index of suspicion is needed if patients are to be managed correctly (Caroline 2007).
SCI should be suspected with any of the following:
• a history of significant trauma and altered mental status from intoxication
• a history of seizure activity since the accident
• any complaint of neck pain or altered sensation in the upper extremities
• a complaint of midline neck tenderness
• a history of loss of consciousness
• an injury above the clavicle
• a fall greater than three times the patient’s height
• a fall that results in a fracture of the heels
• an unrestrained (no seat belt) person with a facial injury
• significant injuries in a RTA that result in chest and intra-abdominal injuries.
The patient may complain of a feeling of ‘electric shock’ or ‘hot water’ running down his back. A history of incontinence before arrival in the ED may be reported (Semonin-Holleran 2003). Failure to suspect a spinal injury will lead to failure in its detection, with potentially devastating consequences for the patient.
The patient’s ability to walk should not be a factor in determining whether he needs to be treated for spine injury. Not all patients will have a dramatic entrance into the ED; in one North American study 17 % of patients who required surgical repair of unstable spine injuries were found ‘walking around’ at the incident scene or walked into the ED in the local hospital (McSwain 1992). A nod of the head or a sneeze in such patients could easily push an unstable fragment of vertebra against the spinal cord. Therefore an unstable spine can only be ruled out by careful physical assessment, radiographic imaging or a lack of any potential mechanism.
Spine immobilization
Once the patient is on the trauma trolley, protection of the c-spine should be given the same priority as the airway (American College of Surgeons 2008). All emergency personnel involved in caring for the patient must be continuously aware that imprudent movement of the spine has the potential to cause secondary injury. The patient must have the c-spine immobilized in a semi-rigid well-fitting cervical collar, have sandbags either side for lateral stabilization and have the forehead taped to the trauma trolley. Collars do reduce movement of the neck, but even correctly fitted ones allow over 30° of flexion, extension and rotation, this is improved by the use of sandbags and tape, which on their own provide better cervical protection than a collar alone (James et al. 2004). Cervical spine injury should be suspected in the presence of head injury, but cervical collars significantly increase intracranial pressure (Ho et al. 2002).
It should also be noted that in children the head is large and the posterior musculature is not well developed. If placed on a rigid board or trolley, a child’s head is typically moved to severe flexion. When immobilizing children, significant padding under the torso is usually necessary to maintain the immobilization (Pre-Hospital Trauma Life Support Committee 2006).