Fig. 23.1
Location of the dorsal root ganglion (DRG) as compared to the pedicle
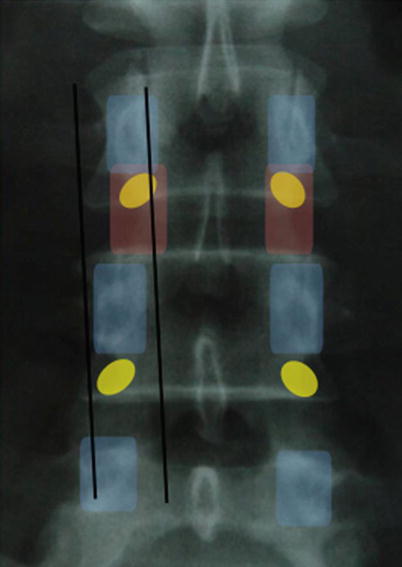
Fig. 23.2
Radiographic of DRG location. Blue indicates pedicle; red indicates neuroforamen; yellow indicates DRG
Using fluoroscopic guidance and loss-of-resistance technique, the epidural space of the spinal canal is punctured with the bevel of the needle (a modified 14G Tuohy) facing towards the targeted DRG at an angle of approximately 30°. Once loss of resistance is achieved, complete insertion into the epidural space can be verified by inserting a guide wire through the needle.
The quadripolar DRG stimulation lead and its delivery system should be prepared at this point. The curved stylet must be inserted into the flexible lead from the back, and the lead must be loaded into a curved sheath from the front. Make sure the stylet is completely inserted into the lead (Fig. 23.3) and that the lead is completely inserted into the sheath. The ball tip end of the lead should be flush against the sheath and tightened down with the lead stabilizer until the lead does not slide within the sheath.
Fig. 23.3
Convergence and divergence of the afferent nociceptive input to the spinal cord can be exploited to provide therapeutic coverage over larger or smaller regions
Prior to placing the sheath, the implanter should determine the length of the lead required to extend from the targeted foraminal level to the site for the internal pulse generator (IPG). Using a 90-cm lead in the lumbar region may cause difficulty in coiling the excess lead, whereas a 50-cm lead used in the upper thoracic region may not be long enough to reach the IPG implantation site, with a potential risk of dislocation. In this situation, a lead extension should be considered to bridge the additional length.
Depending on the puncturing angle, the implanter can choose between a smaller and a larger curved sheath. The steering wing on the sheath lines up with the bend of the sheath and allows later steering. The lead and its delivery system are inserted through the needle into the epidural space and advanced towards the targeted foraminal opening.
As noted above, planning the trajectory of the needle is crucial for delivering the lead. If the approach to the foraminal opening is not adequate, it may be useful to choose a more accurate trajectory, with a new puncture site and angle. When retracting the sheath, the steering wing should be aligned with the bevel of the needle to prevent damaging the sheath.
With the distal end of the sheath in or at the targeted foramen, loosen the lead stabilizer and advance the lead so that it moves into the foramen. Ideally, contacts No. 2 and 3 should be just below the pedicle where the DRG is expected to be (Fig. 23.4).
Correct lead position can be confirmed with a lateral fluoroscope image to show lead placement at the dorsal but not ventral ganglion (Fig. 23.5). Intraoperative testing is helpful to verify the area of paresthesia, as well as the lack of motor artifacts. When the lead is correctly placed, programming is often very straightforward.
Fig. 23.4
AP radiograph demonstrating needle trajectory and lead placement in the superior/posterior portion of the foramen, with created stress relief loop
Fig. 23.5
The lead/stylet/sheath system to deploy the lead into the foramen overlying the DRG
Once the lead is successfully in place, the implanter can retract the sheath to anchor the lead within the spinal canal. Advancing the lead further into the epidural space allows the implanter to place a lasso-shaped strain relief (Fig. 23.4). At this point, the implanter can remove the delivery sheath by gently pulling back the sheath near the needle. A fluoroscopic marker is placed at the tip of the sheath, helping to verify the sheath’s position in respect to the lead and needle. The implanter should hold forward pressure on the lead while retracting the sheath to prevent lead migration, by retracting the stylet beyond the tip of the sheath into the needle. The implanter then should turn away the sheath from the opening of the foramen and advance the lead to create a loop in the epidural space. The trial leads can be placed through a needle and secured to the skin with occlusive dressing, or a staged approach can used. In the staged method, once the leads are in place, a skin incision is made at the insertion site of the electrodes. (The Tuohy needle can be left in place to protect the electrode from the scalpel at this point.) The fascia is prepared towards the insertion site of the leads. The Tuohy needle is removed, and an anchor is placed. The anchor is sutured to the fascia and the lead to minimize the risk of dislocation. See Fig. 23.6