Somatic Blockade of the Head and Neck
Santhanam Suresh
Narasimhan Jagannathan
Regional anesthesia for head and neck procedures have a long and successful history of use and application in dental surgery and otolaryngology. The application of these blocks has now extended into the breadth of plastic surgery (1), neurosurgical procedures (2), and, in addition, to outside the operating room, such as in treatment of chronic pain states. Important advantages of regional techniques include decrease in intraoperative and postoperative opioids use (3) as well as a less stressful perioperative experience. Regional anesthesia for procedures involving the head and neck can potentially provide excellent postoperative analgesia without the adverse effects of opioids (4).
Regional anesthetic techniques involving the head and neck are predominantly sensory nerve blocks, and adverse effects such as nerve damage are rarely reported. Because of the anatomy of the area, and the close relationship of cranial and cervical nerves to many vital structures, meticulous placement of the needle and smaller volumes of the anesthetic agent are required. The landmarks for regional anesthesia in the head and neck are relatively constant, easily located, and mostly predictable. Despite these advantages, nerve blocks to the head and neck remain underutilized in routine clinical practice.
Applied anatomic knowledge is of vital importance for the success of regional anesthesia in general and particularly so in providing regional anesthesia of the head and neck. Cadaveric dissections, reviewing the anatomy with a regional anesthesia atlas, and frequent reference to a model skull is advisable, both while learning how to perform these blocks and prior to such procedures. The availability of these techniques on dedicated regional anesthesia web sites, with video-assisted demonstrations of these blocks, has increased their usage in anesthesia practice.
As more prospective studies are performed and peer-reviewed literature of regional anesthesia for head and neck procedures are made available, the demand and popularity of these techniques may increase. This chapter will elucidate the anatomy, technique, and potential advantages and adverse effects of commonly used peripheral nerve blocks of the head and neck. Regional blockade of the mouth and circumoral structures, as well as the eye, are described in detail in Chapters 18 and 19, respectively. These techniques will be only briefly discussed in the current chapter.
Applied Anatomy
The trigeminal nerve and the cervical plexus primarily provide the cutaneous sensory innervation to the face, head, and neck. In addition, the glossopharyngeal and vagus nerves supply the pharynx and larynx.
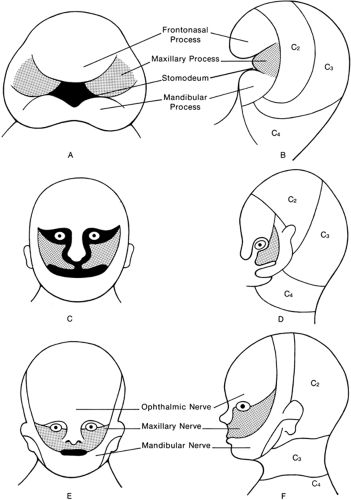
Embryology
The anatomy and complexity of the nerve supply of the head, neck, and face in the adult is perhaps best understood in light of its development in the embryo, as the face forms around the primitive mouth (the stomodeum). Initially, the stomodeum is surrounded caudally by the mandibular arch (which is supplied by the mandibular nerve), laterally on each side by the maxillary processes (which are supplied by the maxillary division of the trigeminal nerve), and rostrally by the forebrain capsule, from which develops the frontonasal process (which is supplied by the first division of the trigeminal nerve, the ophthalmic nerve). The frontonasal process grows down into the primitive stomodeum from the forebrain capsule, and eventually this will form the nose of the mature embryo (Fig. 17-1). The two maxillary processes grow inward from either side and join together below the primitive nose, as shown, and they then form the rostral margin of the primitive mouth. Thus, in the mature face, the forehead, eyebrows, upper eyelids, and nose are supplied by the first ophthalmic division of the trigeminal nerve. The lower eyelid, cheek, and upper lip are supplied by the second division (i.e., the maxillary nerve), and the lower lip, chin, mandibular, and temporal regions are supplied by the third division, mandibular nerve. Because of the disproportionate growth of the cranial cavity in humans, these dermatomal distributions are distorted cranially, with the result that some skin innervated by the cervical plexus is drawn up over the angle of the mandible onto the face and posteriorly over the occipital area and the scalp as far forward as the vertex (Fig. 17-2).
The Trigeminal Nerve
The trigeminal nerve is the predominant sensory nerve of the head and face, and is also the motor supply for the muscles of mastication. It originates from the pons. The sensory fibers derive from the cells of the semilunar temporal bone. As it enters the pons, it divides into upper and lower roots. Three branches arise, the ophthalmic V1, maxillary V2, and the mandibular V3 divisions. Both the ophthalmic and maxillary divisions consist exclusively of sensory fibers, whereas the mandibular nerve also has a motor component (Table 17-1).
The semilunar ganglion, also known as the Gasserian ganglion, lies posteromedially in the middle cranial fossa at the junction of its floor and the cavernous sinus just anterior to the ridge of the petrous temporal bone. The ganglion invaginates the dura and therefore lies in a dural pouch—Meckel’s cave—which contains cerebrospinal fluid (CSF).
Ophthalmic (V1) Division Trigeminal Nerve
In its intracranial course, the trunk of the ophthalmic nerve does not lend itself to regional anesthesia. The intraorbital branches of the nasociliary nerve are blocked by retrobulbar block. The intraorbital branches, anterior ethmoidal and infratrochlear, can also be blocked in the orbit. The terminal divisions in the forehead and nose are suitable for peripheral nerve blocks of the scalp and face (6).
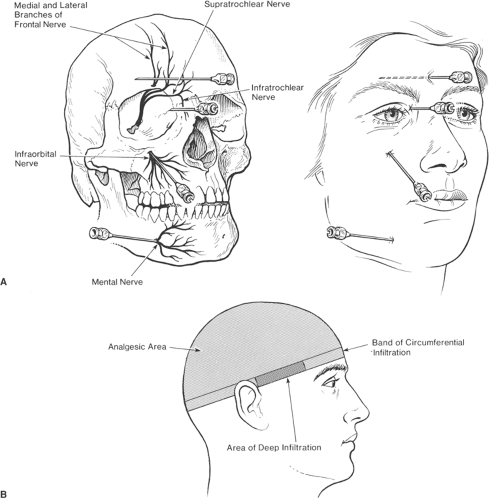
The ophthalmic nerve is the smallest division of the trigeminal nerve. It supplies the cornea, conjunctiva, ciliary body, and the iris. The lacrimal gland; mucous membranes of the nasal cavity; the skin of the eyebrow, eyelids, and forehead; and the nose are also supplied by this division. The frontal nerve is the largest branch and may be regarded as the continuation of the first division of the trigeminal nerve. As it enters the orbit through the superior orbital fissure, it proceeds forward between the levator palpebrae superioris and the periosteum. The two branches, the supraorbital and the supratrochlear nerve supply sensory innervation to the forehead and anterior scalp (Fig. 17-3). The supraorbital nerve and vessels emerge from the supraorbital foramen and continue superiorly on the anterior portion of the forehead and scalp. The supraorbital nerve trunk divides into a deep and a superficial branch. The deep branch courses superiorly and laterally, running parallel to
the superior temporal line of the skull in the loose areolar tissue between the galea and the pericranium. The terminal branches of the deep supraorbital nerve branch pierces the galea near the coronal suture to supply scalp sensation. The superficial division lies medially at its origin and quickly divides into multiple branches that pierce the frontalis muscle. These smaller branches pass cephalad to supply the forehead and up to 3.5 cm of the frontal scalp.
the superior temporal line of the skull in the loose areolar tissue between the galea and the pericranium. The terminal branches of the deep supraorbital nerve branch pierces the galea near the coronal suture to supply scalp sensation. The superficial division lies medially at its origin and quickly divides into multiple branches that pierce the frontalis muscle. These smaller branches pass cephalad to supply the forehead and up to 3.5 cm of the frontal scalp.
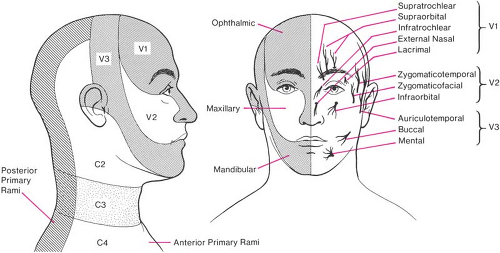 Figure 17-2. Dermatomes and cutaneous nerves of head, neck, and face. Note that the supraorbital, infraorbital, and mental nerves all lie in the same vertical plane as the pupil, with the eye looking straight forward. The external nasal area is innervated by infratrochlear and external nasal (from anterior ethmoidal n.) branches of V1 and the infraorbital branch of V2. The internal nasal cavity is shown in Figure 17-6. |
The supratrochlear nerves exit the orbit at the superior orbital rim through a notch, above the trochlea and medial to the supraorbital notch. At the supraorbital rim, the nerves penetrate the corrugator muscle and the frontalis muscle. The nerves supply cutaneous sensation to a central vertical strip of forehead and to the medial upper eyelid (7).
Table 17-1 Trigeminal nerve distribution | |
|---|---|
|
Maxillary Division (V2) of the Trigeminal Nerve
The maxillary nerve is purely sensory and is called the infraorbital nerve when it reaches the infraorbital fossa. It divides into four branches: the external nasal, the internal nasal, the inferior palpebral, and the superior labial. The nerve can be easily accessed superficially. The posterior superior alveolar branch arises from the trunk of the nerve just before it enters the infraorbital groove. It enters the infratemporal surface of the maxilla communicating with the middle superior alveolar branch, giving off branches to the lining membrane of the maxillary sinus and branches to the molar teeth. The middle superior alveolar branch arises from the nerve in the posterior part of the infraorbital canal and runs downward and forward in a canal along the lateral wall of the maxillary sinus. The anterior superior alveolar nerve branches off just as it exits the infraorbital foramen and descends in a canal in the anterior wall of the maxillary sinus. It communicates with the middle superior alveolar branch, which supplies the mucous membrane of the anterior part of the inferior meatus and the floor of the nasal cavity, communicating with the branches from the sphenopalatine ganglia. The external nasal branches supply the skin of the nose and of the septum mobile nasi and joins with the terminal branches of the nasociliary nerve. The superior labial branches, the largest, descend behind the quadratus labii superioris and are distributed to the skin of the upper lip, the mucous membrane of the mouth, and the labial glands. They are joined, immediately below the orbit by filaments from the facial nerve, forming with them the infraorbital plexus (7). A computed tomography (CT)-guided imaging study demonstrated that the infraorbital foramen is located approximately 2 cm lateral to the midline in most children at the level of the inferior rim of the orbit (8). The superior anterior part of both
septum and lateral wall of the nose receive contributions from the anterior ethmoidal branch of the ophthalmic nerve. The entire hard palate is supplied by the maxillary nerve via the sphenopalatine ganglion.
septum and lateral wall of the nose receive contributions from the anterior ethmoidal branch of the ophthalmic nerve. The entire hard palate is supplied by the maxillary nerve via the sphenopalatine ganglion.
Palatine Nerve
The palatine nerves are distributed to the roof of the mouth, soft palate, tonsil, and lining membrane of the nasal cavity. Most of their branches are derived from the sphenopalatine branches of the maxillary nerve. There are three main branches: the anterior, middle, and posterior branches.
The anterior palatine nerve descends through the pterygopalatine canal and emerges in the hard palate through the greater palatine foramen. It passes in a groove in the hard palate as far as the incisor teeth. It supplies the gums, and the mucous membrane and glands of the hard palate.
The middle palatine nerve emerges through one of the minor palatine foramen and provides the sensory supply to the uvula, tonsils, and the soft palate.
The posterior palatine nerve descends through the pterygopalatine canal and emerges through a special opening behind the greater palatine foramen. It supplies the sensory branches to the soft palate, tonsils, and uvula. The middle and posterior palatine branches join the tonsillar branch of the glossopharyngeal to form a plexus (cirrus tonsillaris) around the tonsils (7).
Mandibular Division (V3) of the Trigeminal Nerve
The mandibular nerve emerges from the cranial cavity through the floor of the middle cranial fossa, via the foramen ovale, to enter the infratemporal fossa. This fossa is a rectangular compartment bounded anteriorly by the posterior wall of the maxilla and posteriorly by the styloid apparatus and carotid sheath. The lateral wall is the ramus of the mandible, and the medial wall is composed anteriorly of the lateral pterygoid plate of the sphenoid bone and posteriorly by the constrictor muscles of the pharynx. It has no floor, but its roof is the floor of the middle cranial fossa. In the infratemporal fossa, the mandibular nerve divides into its terminal branches.
Glossopharyngeal Nerve
The glossopharyngeal nerve supplies the posterior third of the tongue and the oropharynx from its junction with the nasopharynx at the level of the hard palate. It supplies the pharyngeal surfaces of the soft palate and the epiglottis, and the pharyngeal wall, as far down as the pharyngoesophageal junction at the level of the cricoid cartilage (C6).
Vagus Nerve
The vagus nerve supplies sensation to the larynx. The undersurface of the epiglottis and the laryngeal inlet down to the vocal folds are supplied by the internal laryngeal branch of the vagus. This nerve reaches the larynx by piercing the thyrohyoid membrane, which joins the thyroid to the hyoid cartilages. Below the cords, the larynx and trachea are supplied by the recurrent branch of the vagus that ascends in the neck, in the groove between the trachea and esophagus. The recurrent laryngeal nerve also supplies motor function to all the intrinsic muscles of the larynx (except the cricothyroid muscle), and bilateral motor block produces loss of phonation and loss of ability to close the glottis.
Cervical Plexus
The cervical plexus contributes to the supply of both the deep and the superficial structures of the neck. The first cervical nerve, C1, is a motor nerve to the muscles of the suboccipital triangle and has no sensory distribution to skin. The skin of the neck is supplied in a sequential dermatomal pattern (like the trunk) by the cutaneous branches of C2–C4 by both anterior and posterior primary rami. The cervical plexus is formed by the ventral rami of the upper four cervical nerves. Their dorsal and ventral roots combine to form spinal nerves as they exit through the intervertebral foramen. The anterior rami of C2 through C4 form the cervical plexus. The cervical plexus lies behind the clavicular head of the sternocleidomastoid, giving out both the superficial and deep branches. The superficial cervical plexus wraps around the belly of the clavicular head of the sternocleidomastoid to form four branches: (a) the lesser occipital, (b) the great auricular, (c) the transverse cervical, and (d) the supraclavicular nerves. The great auricular nerve is the largest of the ascending branches. It arises from the second and third cervical nerve roots, winds around the posterior border of the sternocleidomastoid and, after perforating the deep fascia, ascends behind the clavicular head of the sternocleidomastoid beneath the platysma to the parotid gland, where it divides into an anterior and posterior branch. The anterior branch (ramus anterior; facial branch) is distributed to the skin of the face over the parotid gland and communicates in the substance of the gland with the facial nerve. The posterior branch (ramus posterior; mastoid branch) supplies the skin over the mastoid process and on the back of the auricle, except at its upper part; a filament pierces the auricle to reach its lateral surface, where it is distributed to the lobule and the lower part of the concha. The posterior branch communicates with the smaller lesser occipital, the auricular branch of the vagus, and the posterior auricular branch of the facial nerve (7).
In the region of the scalp, the nerves of supply have long superficial upward courses. Four sensory nerves pass in front of the ear to the scalp (supratrochlear and supraorbital from V1, zygomaticotemporal from V2, auriculotemporal from V3), and four pass behind the ear (great auricular and greater, lesser, and least occipital nerves from cervical plexus) (Figs. 17-2 and 17-3).
Trigeminal Nerve Block
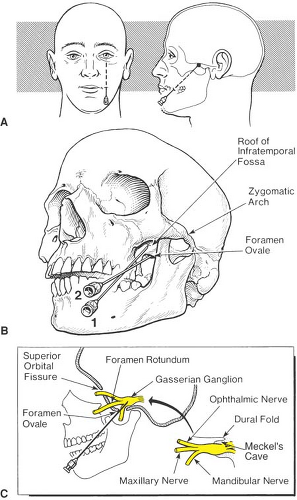
Gasserian Ganglion Block
Indications
Gasserian ganglion block results in extensive anesthesia of the ipsilateral face, over the area shown in Figure 17-4. It was once used solely for surgery of the head and neck. With the advent of endotracheal intubation and more sophisticated techniques for general anesthesia, its appeal as a primary surgical anesthetic declined. However, it is still used diagnostically and therapeutically for neuralgias of the trigeminal system. It has merit as a diagnostic block, a permanent neurolytic block, and as a means
of introducing heated probes for the newer techniques of thermogangliolysis (11) (Chapters 42 and 45).
of introducing heated probes for the newer techniques of thermogangliolysis (11) (Chapters 42 and 45).
The Gasserian ganglion is reached with a needle by traversing the infratemporal fossa and entering the middle cranial fossa by way of the foramen ovale. Medially, the Gasserian ganglion is bounded by the cavernous venous sinus, which contains the carotid artery, and the third, fourth, and sixth cranial nerves. Superiorly, it is the inferior surface of the temporal lobe of the brain, and posterior to the ganglion lies the brainstem. Any of these structures might be damaged by the introduction of the needle through the foramen ovale. The ganglion is partially bathed in CSF, hence injections into the area might spread into the spinal fluid (Fig. 17-4).
Technique
An 8- to 10-cm, 22-gauge needle is required for Gasserian ganglion block. The point of introduction of the needle is approximately one finger’s breadth posterior to the lateral margin of the mouth, next to the medial border of the masseter muscle (Table 17-2). In edentulous patients, this landmark may not permit a sufficient angle of approach to enter the foramen ovale, and therefore a point of insertion more caudad is needed. The direction of the needle is both rostral and medial, to a point that coincides with the midpoint of the zygomatic arch when viewed from the lateral aspect, and the pupil from the anterior view (with the eyes looking straight forward), as in Figure 17-4. It is important to keep a guiding finger in the oral cavity, palpating the cheek to ensure that the needle does not enter the mouth, which might, potentially, introduce contaminating bacteria into deeper structures. Such an approach usually causes the needle to impinge on the roof of the infratemporal fossa (i.e., the base of the skull, which is also the floor of the middle cranial fossa). The needle is then adjusted until it slips through the foramen ovale; usually, just prior to this, a mandibular nerve paresthesia is obtained in the lower jaw or lip. This maneuver is optimally (but not necessarily) performed under radiographic control, so that the needle and its path through the foramen ovale can be visualized (5). After the foramen ovale is entered, the needle should not be advanced more than 1 cm, and usually its advance is guided by the appropriate paresthesia.
Initially, there will be a third-division mandibular paresthesia, but this can occur while the needle is still in the infratemporal fossa. A second-division maxillary paresthesia must be obtained, or a first-division paresthesia to the upper jaw or frontal area of the face, respectively, to confirm that the needle
is in fact in the immediate vicinity of the Gasserian ganglion. A stimulating device may be used to confirm the position of the needle in patients who are unable to locate the paresthesia accurately. This, being a painful procedure, would require some intravenous (IV) analgesics or sedation prior to performance of the block. For diagnostic blocks, however, it is better not to alter the sensorium with any analgesics in order to obtain a more accurate assessment of the block.
is in fact in the immediate vicinity of the Gasserian ganglion. A stimulating device may be used to confirm the position of the needle in patients who are unable to locate the paresthesia accurately. This, being a painful procedure, would require some intravenous (IV) analgesics or sedation prior to performance of the block. For diagnostic blocks, however, it is better not to alter the sensorium with any analgesics in order to obtain a more accurate assessment of the block.
Table 17-2 Gasserian ganglion block | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Prior to injection, aspiration tests are mandatory to ensure that the needle has not entered a blood vessel or, in a more likely outcome, the Meckel cave, with its CSF contents. If these aspiration tests are negative, then the anesthetizing agent, either a local anesthetic (1% lidocaine or the equivalent) or a neurolytic agent, is injected in small aliquots (e.g., 0.25 mL at a time) until the desired analgesic effect is obtained. If injection affords evidence of analgesia in only one of the divisions, then adjustment of the needle sometimes can affect spread to the other divisions—in patients in whom the needle is in the same vertical axis as the ganglion. However, there appear to be some patients in whom the ganglion lies at a more horizontal axis, and in these patients it is sometimes difficult, if not impossible, to obtain a first-division paresthesia.
Complications
Depending upon the manipulations needed to produce satisfactory block, the patient’s face quite frequently will be painful for few days following the block, and there is often bruising at the injection site. This usually responds well to treatment with mild oral analgesics. Probably the most serious side effect is injection of local anesthetic or neurolytic agent into the CSF contained within the Meckel cave and its resulting spread into the circulating CSF of the cranial cavity. Injections of as little as 0.25 mL of 1% lidocaine have resulted in unconsciousness and profound paralysis of the ipsilateral cranial nerve system, albeit temporary, with the patient needing cardiorespiratory support for a brief period (10 minutes). If a hyperbaric solution is used (e.g., lidocaine with epinephrine or phenol in glycerine), then the drug that emerges from the Meckel cavity will tend to flow over the free margin of the tentorium cerebelli to affect, immediately, cranial nerves VI, VIII, IX, X, XI, and XII, and usually the patient loses consciousness. If hypobaric solutions are used (e.g., lidocaine without epinephrine, or alcohol), then the flow will tend to be cephalad, probably involving the trochlear and oculomotor nerves initially, and almost certainly affecting consciousness to a variable extent.
Clinical Application of Gasserian Ganglion Blockade in Pain States
Local anesthetics injected into the ganglion can produce profound analgesia in certain pain states, such as tic douloureux (but only for short periods), and neurolytic blocks with alcohol were used in the past by some therapists for this condition (5,12,13). The pain relief is obtained at the price of hemifacial and corneal analgesia, with saliva often dribbling out of the ipsilateral, numb side of the mouth. Such blocks, for long-term pain relief, are rarely performed by pain specialists today (Chapters 42 and 45).
Gangliolysis, or thermogangliolysis, has great therapeutic implications because of its proven results (14). For gangliolysis, an insulated needle is placed through the foramen ovale. Electrical stimuli are delivered, and the needle tip is adjusted until paresthesias are elicited in the area of pain and a radiofrequency lesion is made, using a thermistor. This appears to be a successful maneuver in those 30% of tic douloureux patients who do not benefit from carbamazepine or other medication therapy, and approximately 80% will get at least 1 year’s relief of pain. An alternative to thermal coagulation for tic douloureux is provided by “bathing” the trigeminal ganglion in glycerol (0.1–0.3 mL) (15). Proponents of this technique claim the relief is as satisfactory as thermal coagulation, with a greater degree of safety with regard to the production of excessive neural damage. However, it is claimed that glycerol gangliolysis is less likely to produce corneal anesthesia than are radiofrequency lesions of the first division, and so it may have some advantages (16). Gangliolysis has improved success over neurolytic block, surgical neurectomy, and rhizotomy therapies. However, which of the gangliolysis methods is superior is still debated among the proponents of the different techniques.
Blockade of Ophthalmic Nerve Branches: Supraorbital, Supratrochlear, Anterior Ethmoidal Nerves
Indications
Supraorbital and supratrochlear nerve analgesia is a simple block that can produce excellent analgesia of the forehead and scalp back from eyebrows to the vertex (6).
These techniques can be utilized for surgery performed on the scalp, repair to lacerations, removal of cysts, frontal craniotomies, midline dermoid excisions, frontal ventriculoperitoneal shunts, Omaya reservoir placement in neonates (2), and nevus excisions on the anterior portion of the scalp (6) (Table 17-3).
Technique (Supraorbital Block)
The supraorbital foramen is palpated at the roof of the orbital rim, approximately at the level of the pupil in most patients. A 30-gauge needle is utilized. The insertion of the needle is at the level of the eyebrow, at the mid-pupillary line (Fig. 17-3). A subcutaneous wheal of local anesthetic solution is injected with the needle directed parallel to the eyebrow at the site of the needle insertion in a subcutaneous plane. Care should be exercised to avoid placing the needle directly into the foramen. One to 1.5 mL of volume is sufficient for analgesia. Firm pressure should be applied to the area after the needle is withdrawn, preventing the formation of a hematoma.
Table 17-3 Supraorbital/supratrochlear blocks | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Complications
Hematoma formation, intravascular injection, intraneural injection may occur.
Technique (Combined Infratrochlear and Anterior Ethmoidal Block)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree