Figure 18.1 Anatomy of the skin. Normal layers of skin include the epidermis, dermis, subcutaneous, and muscular layers. Artwork created by Emily Evans © Cambridge University Press.
Technique
Transducer selection and preparation
High-frequency (5–10 MHz or higher), linear-array transducers are the best option for the assessment of superficial structures. These transducers have excellent resolution for superficial areas, but are limited in penetration. If there is a need for deeper assessment, a transducer with a lower frequency should be utilized. Alternatively, a curvilinear or endocavitary transducer may be substituted for the assessment of superficial areas. These have the advantage of having a rounded footprint, which might have better skin contact with concave skin surfaces such as webspaces or intergluteal folds.
It is crucial to clean the transducer with an appropriate disinfectant to avoid any possible transmission of pathogens. The transducer needs to be cleaned before and after its use. If the skin is not intact, for example in the case of an open wound or draining lesion, the transducer should be prepared in a sterile fashion (Figures S3.5–7).
Patient position and preparation
Imaging should be acquired prior to the irrigation of the wound, as the introduction of air bubbles could obscure the image. Skin infections and wounds with concern for retained foreign bodies are usually painful, so it is important to take all measures to minimize the patient’s discomfort during the ultrasound examination. This will also help in acquiring optimal images. The region of interest might be prepared with topical anesthetic so that the contact with the transducer is better tolerated. When appropriate, the use of a water bath or stand-off pad can also minimize pressure on the affected area. Having the region of interest fully exposed and easily accessible to the ultrasonographer will facilitate complete scanning. Preparing the (normal) contralateral side is also helpful, as it can be used as a control, and subtle changes will become more noticeable.
Ultrasound imaging
The transducer should be held perpendicular to the skin. The depth should be adjusted, so that the region of interest is in the center of the ultrasound image. A minimal amount of pressure should be used in order to avoid possible collapse of an overlying blood vessel.
The region of interest should always be scanned in two orthogonal planes in order to appropriately assess the size and shape of the area of interest and surrounding structures. It is useful to start to scan from unaffected tissue and more towards the affected tissue. Additionally, if applicable, the affected area should be compared to the corresponding normal contralateral part of the body, to appreciate differences between the healthy tissue and the affected side. This is especially important in subtle cases.
On ultrasound, soft tissue has a very organized pattern on ultrasound (Figure 18.1b). The dermis and epidermis appear as a single echogenic and bright layer relative to the subcutaneous tissue, which is mainly comprised of fat. Subcutaneous fat appears hypoechoic, in a reticular pattern. Some thin echogenic tracts of connective tissue can usually be seen crossing the subcutaneous tissue. The thickness of this layer varies greatly depending on the region of the body and the body habitus of the person.
Deeper structures are also visible on ultrasound, and are important to identify so as to avoid them during incision and drainage (Figure 18.2). Muscular fascia appears as thin, bright, hyperechoic layers superficial to the muscular planes. When viewed in the long-axis, muscles have a characteristic striated appearance. When viewed in the short-axis, muscles have a characteristic speckled appearance. In addition, tendons may be visualized, and appear echogenic, finely striated, and can be observed to move when the patient moves the corresponding joint. Further, blood vessels appear as anechoic, linear or circular structures, depending on probe orientation. It is important to use minimal pressure when assessing the area of incision, as overlying veins could collapse and go unnoticed. Arteries have thicker walls, are pulsatile, and require a larger force to be compressed. Finally, depending on the area that has been scanned and the depth that is required, bone might be also visualized. It has a characteristic bright, echogenic cortex, with posterior shadowing.
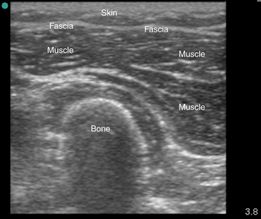
Figure 18.2 Normal soft tissue layers on ultrasonography. The skin and fascia can be visualized superficially. The muscle is seen as striated, with hyperechoic connective tissue running among the fibers. Deep to these layers, a bone is seen, with its characteristic posterior shadowing.
Specific scanning techniques
Cellulitis vs. abscess
Cellulitis is an infection of the skin and subcutaneous tissues. There is a spectrum of sonographic appearances, and findings that are nonspecific. Sonographic findings arise from the accumulation of fluid and swelling of the subcutaneous tissue. When compared to the normal contralateral side (Figure 18.3a), there is initial thickening of the subcutaneous tissue layer visualized on ultrasound (Figure 18.3b). As it progresses, there is disruption of the normal soft tissue architecture and develops disarray in the subcutaneous tissue (Figure 18.4a). On ultrasound, the intracellular edema appears as hypoechoic or anechoic strands which randomly traverse the subcutaneous fat and cause increased separation of the fat globules (Figure 18.4b). This is called “cobblestoning,” as its pattern resembles that of a cobblestoned street (Figure 18.4c). There is also some posterior enhancement artifact as ultrasound passes through the fluid, which makes the fat appear hyperechoic when compared to the contralateral side. As cellulitis progresses, there is extravasation of inflammatory fluid from the vessels, and occasionally a layer of pre-fascial fluid will accumulate. A thick layer of pre-fascial fluid of greater than 4 mm has been described in necrotizing fasciitis, and if seen should raise the suspicion for this disease.
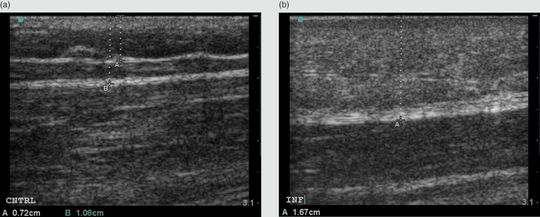
Figure 18.3 Cellulitis. (a) Normal soft tissue thickness is measured from the skin surface to the pre-muscular fascia; here it is measured at 1.08 cm. (b) In early cellulitis, the thickness of the soft tissue is increased and hyperechoic, measured here at 1.67 cm. It is thicker than the normal, contralateral side.
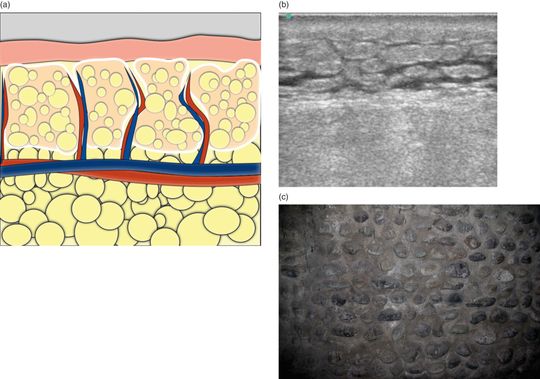
Figure 18.4 Cellulitis. (a) Illustration of the development of lobules and intracellular edema seen in cellulitis. (b) Ultrasound image of cellulitis demonstrates this classic “cobblestoning” pattern, in which subcutaneous edema is seen as hypoechoic stranding within the soft tissue and surrounding the fat globules. (c) Resemblance to cobblestones.
Abscesses have a highly variable appearance on ultrasound (Figure 18.5). Their usual sonographic appearance is an anechoic or hypoechoic spherical or elliptical-shaped collection of fluid. The margins may be outlined by an echogenic rim or blend in with the surrounding tissue, with posterior acoustic enhancement. The surrounding tissues may appear hyperechoic. Within the abscess, there are variable amounts of internal echoes, ranging from none to a frankly heterogeneic collection of fluid. The ability to induce visible motion of abscess contents with gentle compression of the transducer will also help with the diagnosis. This is especially helpful when the suspected fluid is isoechoic or hyperechoic to the surrounding tissue. When compression causes movement of this material, it is called a positive “squish sign,” which means that the material is likely to be fluid and therefore susceptible to drainage (Figure 18.6). If available, color flow or Doppler may also be used to confirm that the structure is not vascular, as no color flow or Doppler waveform should be seen in an abscess. This can also be helpful in differentiating a lymph node from an abscess, as flow within a central vessel of a lymph node can sometimes be seen.
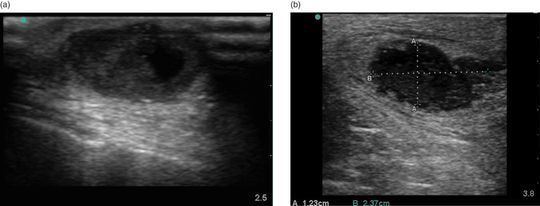
Figure 18.5 Abscesses. (a) An abscess with both anechoic fluid and isoechoic debris. Note also its extension to the surface that is often seen. This is an optimal location for incision and drainage. (b) An abscess with hypoechoic debris, and thick isoechoic walls.
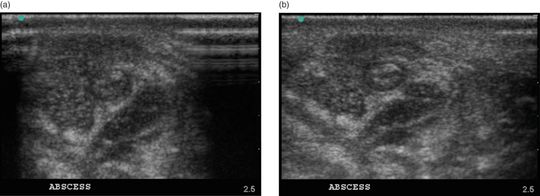
Figure 18.6 The “squish sign.” (a) A superficial abscess in the antecubital fossa of an intravenous drug user. In the center is a clotted vein, consistent with superficial thrombophlebitis. Surrounding the vein anteriorly and medially (to the left of the screen) is an isoechoic fluid collection. It is not obvious that this is fluid until (b) the abscess is compressed and the size and shape of the fluid changes. This is known as a positive “squish sign.”
Foreign-body detection
The sonographic appearance of foreign bodies varies greatly by material, size, and duration of time they have been embedded in the soft tissue. Generally, foreign bodies are hyperechoic and interrupt the well-organized structure of the soft tissue. Wood, glass, plastic, metal, and gravel will all appear hyperechoic when compared with the surrounding tissue (Figure 18.7). If ever in doubt, the normal contralateral side of the body can be scanned for comparison.
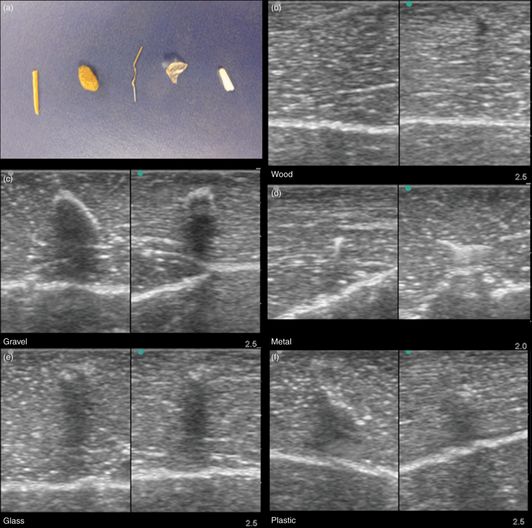
Figure 18.7 Foreign bodies. (a) From left to right: wood, gravel, metal, glass, and plastic. For size comparison, the metal object is a paper staple. These were inserted into a chicken thigh and scanned in two planes. (b) The wooden object is the most difficult to detect in this case, as it casts only a small shadow in one view and none in the other. (c) The gravel has a characteristic shadowing artifact, as do the glass (e) and plastic (f) to a lesser degree. (d) The metal has a classic reverberation artifact, detected as multiple parallel hyperechoic lines inferior to the object.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








