SKIN DISORDERS
SUNBURN
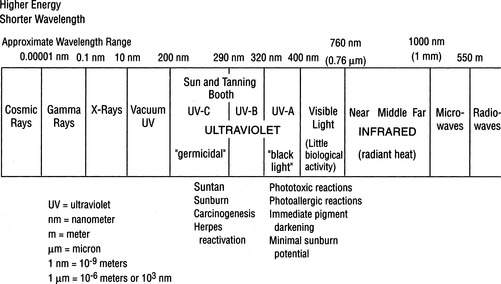
The solar radiation that strikes the earth includes 50% visible light (wavelength 400 to 760 nanometers [nm]), 40% infrared (760 to 1,700 nm), and 10% ultraviolet (UV) (10 to 400 nm) (Figure 119). Energetic rays (e.g., cosmic rays, gamma rays, and x-rays) with wavelengths shorter than 10 nm do not penetrate to the earth’s surface to any significant degree. Sunburn is a cutaneous photosensitivity reaction caused by exposure of the skin to ultraviolet radiation (UVR) from the sun. There are four types of UVR: vacuum UVR is 10 to 200 nm (absorbed by air and unable to penetrate Earth’s atmosphere), UVA is 320 to 400 nm, UVB is 290 to 320 nm, and UVC is 100 to 290 nm. UVC is filtered out by the ozone layer of the atmosphere. UVB is the culprit in the creation of sunburn and cancer. UVA is of less immediate danger but is a serious cause of skin aging, drug-related photosensitivity, and skin cancer. Furthermore, persons taking immunosuppressive agents for medical reasons (e.g., acquired immunodeficiency syndrome [AIDS] or cancer) may be more predisposed to skin cancer caused by UVA.
Wind appears to augment the injury, as do heat, atmospheric moisture, and immersion in water. “Windburn” is not possible without UVR or abrasive sand. Since windburn is due in part to the drying effect of low humidity at high altitudes, it can be helpful to protect the skin with a greasy sunscreen or barrier cream.
If the victim is deep red (“lobster”) without blisters, a stronger antiinflammatory drug, such as prednisone, may be given. A 5-day course of prednisone (80 mg on the first day, 60 mg the second, 40 mg the third, 20 mg the fourth, and 10 mg the fifth) may decrease the discomfort of “sun poisoning,” which is the constellation of low-grade fever, loss of appetite, nausea, and weakness that accompanies a bad total-body sunburn. Corticosteroids should always be taken with the understanding that a rare side effect is serious deterioration of the head (“ball” of the ball-and-socket joint) of the femur, the long bone of the thigh. An extensive nonblistering first-degree sunburn can make the victim nauseated and weak, with low-grade fever and chills. He should be forced to drink enough balanced electrolyte-supplemented liquids to avoid dehydration (see page 208).
With a severe sunburn in which blistering is present, the victim has by definition suffered second-degree burns (see page 108) and should be treated accordingly. Gently clean the burned areas and cover with sterile dressings. Administer appropriate pain medication.
SUNSCREENS
Type I. Always burns easily, never tans. (Fair-skinned people with a high number of moles are at the greatest risk for melanoma.)
Type II. Always burns easily, tans minimally.
Type III. Burns moderately, tans gradually and uniformly (light brown).
Type IV. Burns minimally, always tans well (moderate brown).
Type V. Rarely burns, tans profusely (dark brown).
In all cases it is wise to overestimate the protection necessary and to carry a strong sunscreen. To protect hair from sun damage, wear a hat.
Substantivity refers to the ability of a sunscreen to resist water wash-off. Layering sunscreens doesn’t work well, because the last layer applied usually washes off. Current specialty sunscreens with high substantivity include Bullfrog Water Pro Body Gel, Aloe Gator Total Sun Block Lotion, and Dermatone Ultimate Fisherman’s Sunscreen.
Sunscreens are first applied to cool, dry skin for optimal absorption; wait 10 minutes before water exposure. Reapply them liberally after swimming or heavy perspiration. In general, most sunscreens should be reapplied every 20 minutes to 2 hours. Be aware that the concomitant use of insect repellent containing DEET (see page 390) lowers the effectiveness of the sunscreen by a factor of one-third. Although many sunscreens are designed to bond or adhere to the skin under adverse environmental conditions, there are certain situations in which any sunscreen should be reapplied at a maximum of 3- to 4-hour intervals:
• Continuous sun exposure, particularly between the hours of 10 a.m. and 3 p.m.
• Exposure at altitude of 7,000 ft (2,135 m) or higher
• Exposure within 20 degrees latitude of the equator
• Exposure during May through July in the Northern Hemisphere, and December through February in the Southern Hemisphere
• Frequent water immersion, particularly with toweling off
• Preexisting sunburn or skin irritation
• Ingestion of drugs, such as certain antibiotics, that can cause photosensitization
If you are concerned about jellyfish stings, a useful product is Safe Sea Sunblock with Jellyfish Sting Protective Lotion (www.buysafesea.com), which is both a sunscreen and a jellyfish sting inhibitor.
Although “tanning tablets” or “bronzers” induce a pigmentary change in the skin that resembles a suntan, they provide minimal, if any, true protection from the effects of ultraviolet exposure. Like the sun, indoor tanning machines induce skin changes that lead to premature skin aging and cancer. The best tan derived from the natural sun’s UVB carries an SPF of approximately 2; a tanning bed supplies UVA and therefore no protection.
MELANOMA
Warning signs within a skin lesion include the following:
1. Irregular, ragged, jagged, notched, or blurred border.
2. Asymmetrical appearance (one portion different from the rest, with respect to color, darkness, or texture).
3. Change in appearance or features (size, color, texture, sensation); onset of pain in a lesion; rapid growth of a lesion.
4. Recent growth, bleeding, itching, scaling, or tenderness.
5. Discoloration (black, dark brown, blue, red, white, mottled).
POISON IVY, SUMAC, AND OAK (GENUS TOXICODENDRON)
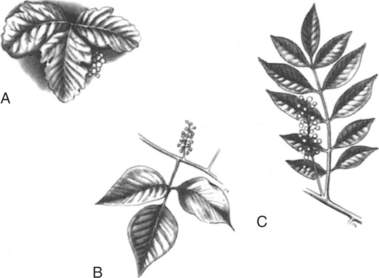
The rashes of poison ivy, poison sumac, and poison oak are caused by a resin (urushiol) found in the resin canals of leaves, stems, vines, berries, and roots (Figure 120). The resin is not found on the surface of the leaves. The potency of the sap does not vary with the seasons. In its natural state, the oil is colorless; on exposure to air, oxidation causes it to turn black. Because the plant parts have to be injured to leak the resin, most cases are reported in spring, when the leaves are most fragile. Dried leaves are less toxic, because the oil has returned to the stem and roots through the resin canals. However, smoke from burning plants carries the residual available resin in small particles and can cause a severe reaction on the skin and in the nose, mouth, throat, and lungs.
The poison oak group does not grow in Alaska or Hawaii, and it rarely grows above 4000 ft (1219 m). Other plants or parts of plants that contain urushiol include the India ink tree, mango rind, cashew nut shell, and Japanese lacquer tree. A smaller number of reactions are caused by the poisonwood tree found in the southern tip of Florida. Because the resin is long lived, it can be spread by contact with tents, clothing, and pet fur.
For treatment of the skin reaction, shake lotions such as calamine are soothing and drying, and they control itching. A good nonsensitizing topical anesthetic is pramoxine hydrochloride 1% (Prax cream or lotion); Caladryl contains calamine and pramoxine. Avoid topical diphenhydramine, benzocaine, and tetracaine. Antihistamines (such as diphenhydramine [Benadryl]) control itching and act as sedatives. Nonsedating antihistamines, such as fexofenadine (Allegra), may also diminish itching. A soothing bath in tepid (not hot) water with half a 1 lb box of baking soda, 2 cups (551 ml) of linnet starch, or 1 cup (275 mL) Aveeno oatmeal is excellent. If Aveeno is not available, a woman’s nylon stuffed with regular (not instant) oatmeal can be thrown in the tub. Soothing aluminum acetate in water (1:20) soaks may help, as might aluminum subacetate (Burow’s solution, Domeboro), which comes as a 5% solution that should be diluted to a 1:40 concentration. When these soaks are used, they should be applied as cotton-soaked wet dressings 3 to 4 times a day for 15 to 30 minutes per application to dry out the weeping rash. Topical steroid creams are generally of little value. Potent topical steroid ointments are not effective unless they are applied before the appearance of blisters and continued for 2 to 3 weeks, so are not recommended. Alcohol applications are painful and do not hasten resolution of the rash. There are new topical agents, such as pimecrolimus (Elidel) 1% cream and tacrolimus (Protopic) 0.03% or 0.1% ointment, which modulate the immune system and are effective without causing skin atrophy, as would be caused by a superpotent topical steroid.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree