Chapter 38 Skin and Soft Tissue Infections
General Principles
1 If patients with skin or soft tissue infection are seen with signs of systemic toxicity, what laboratory studies should be undertaken?
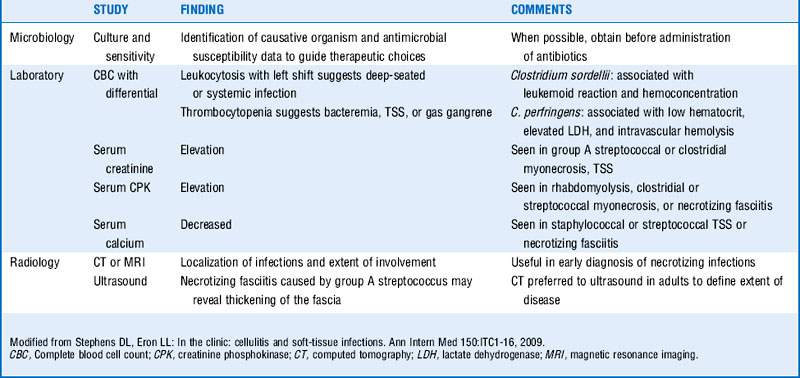
Blood cultures, cultures of drainage from skin infection site, complete blood cell count with differential, and serum creatinine, bicarbonate, creatine phosphokinase, glucose, albumin, and calcium levels should be obtained. (See Table 38-1.)
3 Which common causative organisms have shown emerging antibiotic resistance?
 Staphylococcus aureus (methicillin resistance with resistance to all β-lactams except ceftaroline): Assume resistance because of high prevalence of methicillin-resistant S. aureus (MRSA), both community and hospital acquired.
Staphylococcus aureus (methicillin resistance with resistance to all β-lactams except ceftaroline): Assume resistance because of high prevalence of methicillin-resistant S. aureus (MRSA), both community and hospital acquired.
 Streptococcus pyogenes (erythromycin resistance): Resistance is increasing to macrolides (approximately 7% in the United States, 2% to 32% reported in Europe), although the majority remain susceptible to clindamycin, and all are susceptible to penicillin.
Streptococcus pyogenes (erythromycin resistance): Resistance is increasing to macrolides (approximately 7% in the United States, 2% to 32% reported in Europe), although the majority remain susceptible to clindamycin, and all are susceptible to penicillin.
Cellulitis
6 Lack of response to initial therapy could signify what?
 If a patient does not respond to initial therapy, consider the possibility of resistant strains, atypical organisms, deeper processes such as necrotizing fasciitis or abscess (which may require surgical intervention), as well as underlying conditions such as diabetes, chronic venous insufficiency, or lymphedema (which may slow the clinical response to antimicrobial therapy).
If a patient does not respond to initial therapy, consider the possibility of resistant strains, atypical organisms, deeper processes such as necrotizing fasciitis or abscess (which may require surgical intervention), as well as underlying conditions such as diabetes, chronic venous insufficiency, or lymphedema (which may slow the clinical response to antimicrobial therapy).
 Timely administration of appropriate antibiotic therapy is essential. One study found that each hour of delay between documented hypotension and administration of antibiotics was associated with an average decrease in survival of 7.6% across all sources of infection; subgroup analysis for patients with skin and soft tissue infections demonstrated a significant increase in the adjusted odds ratio of death. This same study found that time to initiation of effective antimicrobial therapy was the strongest predictor of hospital survival. Despite the impact of delayed therapy, the study found that the median time to effective therapy was 6 hours.
Timely administration of appropriate antibiotic therapy is essential. One study found that each hour of delay between documented hypotension and administration of antibiotics was associated with an average decrease in survival of 7.6% across all sources of infection; subgroup analysis for patients with skin and soft tissue infections demonstrated a significant increase in the adjusted odds ratio of death. This same study found that time to initiation of effective antimicrobial therapy was the strongest predictor of hospital survival. Despite the impact of delayed therapy, the study found that the median time to effective therapy was 6 hours.
7 What risk factors predispose individuals to development of cellulitis?
 Previous episodes of cellulitis in the same location (may result in damage to lymphatics)
Previous episodes of cellulitis in the same location (may result in damage to lymphatics)
 Toe-web abnormalities (i.e., maceration, tinea pedis)
Toe-web abnormalities (i.e., maceration, tinea pedis)
 Breach in skin barrier, such as ulcers, trauma, fungal infection, eczema
Breach in skin barrier, such as ulcers, trauma, fungal infection, eczema
 Surgical procedures that affect lymphatic drainage such as radical mastectomy with lymph node dissection or coronary artery bypass graft for which the saphenous vein has been harvested
Surgical procedures that affect lymphatic drainage such as radical mastectomy with lymph node dissection or coronary artery bypass graft for which the saphenous vein has been harvested
 Chronic medical conditions such as diabetes, arterial insufficiency, chronic venous insufficiency, chronic renal disease, neutropenia, cirrhosis, hypogammaglobulinemia
Chronic medical conditions such as diabetes, arterial insufficiency, chronic venous insufficiency, chronic renal disease, neutropenia, cirrhosis, hypogammaglobulinemia
8 What organisms are associated with cellulitis in:
 Cat or dog bites? Pasteurella multocida, Capnocytophaga canimorsus
Cat or dog bites? Pasteurella multocida, Capnocytophaga canimorsus
 Fresh water exposure? Aeromonas hydrophila
Fresh water exposure? Aeromonas hydrophila
 Saltwater exposure? Vibrio vulnificus and other vibrios
Saltwater exposure? Vibrio vulnificus and other vibrios
 Exposure to fish farming and aquaculture? Streptococcus iniae
Exposure to fish farming and aquaculture? Streptococcus iniae
 Exposure to meatpacking or shellfish? Erysipelothrix rhusiopathiae
Exposure to meatpacking or shellfish? Erysipelothrix rhusiopathiae
 Preorbital cellulitis in children? Haemophilus influenzae
Preorbital cellulitis in children? Haemophilus influenzae
 Hosts with deficiencies in cell-mediated immunity? Cryptococcus neoformans
Hosts with deficiencies in cell-mediated immunity? Cryptococcus neoformans
Cutaneous abscesses
9 How are abscesses managed?
 Large abscesses should be incised and drained, with careful attention to the potential for loculated cavities (and the disruption of these cavities through probing of the pus pocket).
Large abscesses should be incised and drained, with careful attention to the potential for loculated cavities (and the disruption of these cavities through probing of the pus pocket).
 Once drained, the lesion can be left packed or unpacked depending on its extent.
Once drained, the lesion can be left packed or unpacked depending on its extent.
 In the absence of multiple lesions, gangrene, impaired host defenses, fever, or systemic signs and symptoms of infection, once a cutaneous abscess is drained, systemic antimicrobial therapy may not be needed.
In the absence of multiple lesions, gangrene, impaired host defenses, fever, or systemic signs and symptoms of infection, once a cutaneous abscess is drained, systemic antimicrobial therapy may not be needed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree