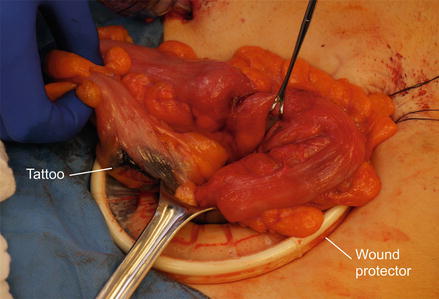
Figure 23.1
Mobilization of the sigmoid colon can be performed in a lateral to medial fashion by incising the white line of Toldt and separating the sigmoid mesentery from the retroperitoneum. Here is the sigmoid colon after complete mobilization
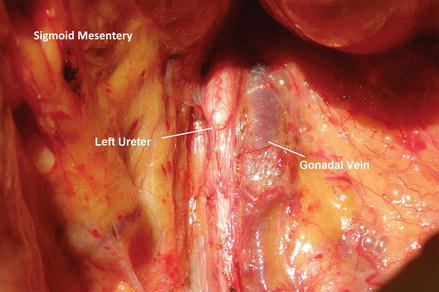
Figure 23.2
Care should be taken to avoid injuring the structures in the retroperitoneum during mobilization, in particular the ureter and the gonadal vessels
The bowel can then be divided proximally using a linear stapling device or sharply with a scalpel between two non-crushing bowel clamps. The distal bowel is divided at the rectosigmoid junction (or more distal if necessary to achieve adequate margins) using either a non-cutting or a linear stapler. The mesentery is then divided using a bipolar energy device, such as the LigaSure™ (Covidien, Mansfield MA). Alternatively, sections of mesentery can be clamped and sharply divided between absorbable ties for vascular ligation. If the resection is being performed for malignancy, the mesenteric resection should occur proximally at the root of the mesentery where the inferior mesenteric artery (IMA) and vein (IMV) are identified. The peritoneum is scored on either side of the IMA and the vessel completely dissected to allow safe transection. A LigaSure™ device (Covidien, Mansfield MA) or suture ligation can be used to ligate this vessel. The IMV is identified lateral to the IMA, near the ligament of Treitz and is divided separately. After completion of the sigmoid resection, the specimen should be opened off the field to ensure the presence of the expected lesion and confirm margins.
The bowel anastomosis is generally performed using a stapled technique, which is faster than hand-sewn and associated with equivalent rates of clinically evident leakage, morbidity, and post-operative mortality [16]. The proximal bowel is elevated and a purse-string suture is placed circumferentially. The bowel is then opened and the anvil of an end-to-end circular stapler is placed inside the bowel lumen. The purse-string suture is closed tightly around the shaft of the anvil and tied. It is important to ensure good apposition of the bowel to the anvil shaft circumferentially. Care should also be taken to exclude epiploica, colonic fat, or diverticula from the surface of the anvil at the chosen anastomotic location as these can inhibit the creation of an intact staple line. One of the operating surgeons then inserts an end-to-end circular stapler trans-anally and gently maneuvers it in place so that the spike is deployed near the center of the distal staple line. The shaft of the anvil is secured to the circular stapler spike and the stapler is then closed and fired. The proper alignment of the descending colon and the absence of tension should be confirmed prior to completing the anastomosis. The stapler is then opened and slowly removed using small twisting movements, until the luminal anvil has traversed the new anastomosis. The anastomotic rings are inspected on the back table to ensure a full circumferential anastomosis. We typically perform a leak test to inspect our anastomosis. The proximal colon is digitally occluded, the anastomosis submerged with warm normal saline irrigation, and the rectum and distal colon insufflated with air using a rigid proctoscope. The anastomosis is carefully observed for any evidence of air bubbles. With the anastomosis complete, the abdomen is then inspected for hemostasis, warm irrigation can be performed, and the retractors removed. All laparotomy pads are removed and a count confirmed prior to closure. The fascia is closed using a running monofilament absorbable suture and the skin closed.
Laparoscopic-Assisted Sigmoid Colectomy
A sigmoid colectomy can be safely and effectively performed laparoscopically with improved post-operative recovery, length of stay, and pain control [8]. We perform sigmoid colectomies with a lap-assisted technique using a small lower midline, transverse Pfannenstiel or vertical peri-umbilical incision to extract the specimen and exteriorize the proximal bowel limb for anvil placement. Hand-assisted techniques also exist for sigmoid colectomy. Entry to the abdomen is obtained by either the Hassan technique or a Veress needle at the umbilicus. Two additional ports are placed, often in the suprapubic (5 mm) and right lower quadrant (12 mm) locations. A fourth port can be placed as needed to aid retraction either in the left lower quadrant or the right upper quadrant, depending on patient habitus and anatomy (Fig. 23.3). After the ports are placed, a 30° camera is introduced into the abdomen and the bowel underlying the ports is examined for iatrogenic injury.
Figure 23.3
Port placement for a laparoscopic sigmoid colectomy. In this case, we chose use the Hassan technique to enter the abdomen at the umbilicus. Three additional 5 mm ports are placed in the suprapubic midline, the right lower quadrant and the right upper quadrant. We have additionally marked the patient’s lower midline prior to insufflation
There are two approaches for a laparoscopic sigmoid colectomy: lateral-to-medial and medial-to-lateral dissection. In the lateral-to-medial approach, atraumatic graspers are used to retract the sigmoid colon medially and a scissors cautery or LigaSure™ (Covidien, Mansfield MA) device are used to take down the lateral peritoneal attachments (Fig. 23.4). The left ureter and gonadal vessels are identified and preserved lateral to the dissection plane. The dissection proceeds superiorly as described previously and the splenic flexure attachments mobilized if necessary (Fig. 23.5). Once the colon has been sufficiently mobilized, the IMA is identified near its take-off from the aorta and the mesenteric peritoneum scored on either side of the vessel. The IMA is then ligated using a linear stapling device with a vascular load or the LigaSure™ (Covidien, Mansfield MA) bipolar device. If additional security is desired, metal clips can be placed on the proximal IMA prior to transection. The IMV is then identified laterally and also transected. The mesentery is then sequentially divided inferiorly toward the rectosigmoid junction. In the medial-to-lateral approach, the IMA and IMV are identified and transected prior to mobilization of the colon. With the mesentery divided, the rectosigmoid or proximal rectum is divided intra-corporeally with an endo-GIA stapler placed via the right lower quadrant port.
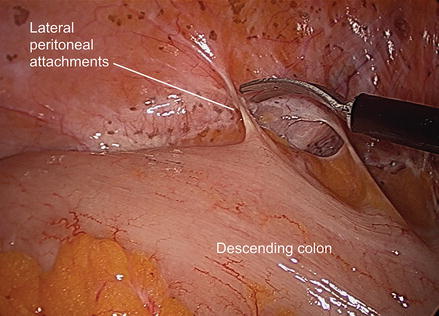
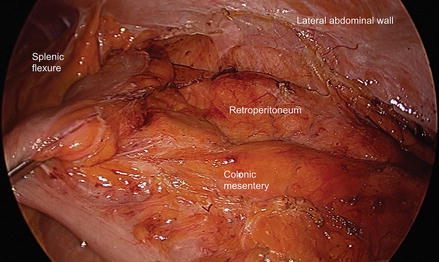
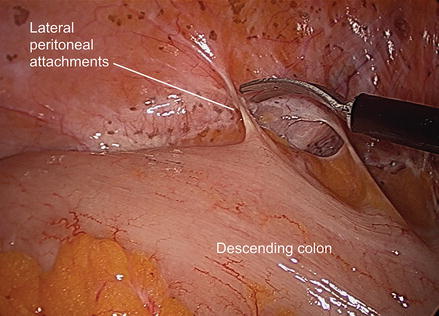
Figure 23.4
The lateral-to-medial dissection begins laparoscopically with division of the lateral peritoneal attachments of the descending colon to the left lateral abdominal wall
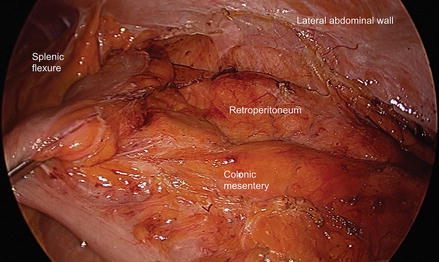
Figure 23.5
The descending colon is completely mobilized medially as the plane between the colonic mesentery and the retroperitoneum is developed. The splenic flexure can be mobilized as needed to gain additional length on the remaining colon in order to complete the anastomosis
A small access incision can now be made in either a transverse or vertical midline suprapubic or peri-umbilical location. A small wound protector is placed and the sigmoid specimen delivered from the abdomen (Fig. 23.6). The proximal colon is divided with a linear cutting stapler or transected after placing a non-crushing bowel clamp followed by purse string suture and anvil placement (Fig. 23.7). If the distal anastomosis is not divided intra-corporeally, it can be transected via the suprapubic incision with a non-cutting stapler (Fig. 23.8). The specimen is again examined off the field to confirm lesion location and margins. The anastomosis can now be completed as described above (Figs. 23.9, 23.10, and 23.11) or by placing the colon back into the abdomen with re-insufflation. A stapled intra-corporeal anastomosis is then performed with the circular end-to-end anastomosis stapler. The abdomen is inspected for hemostasis and irrigated as needed. The access incision is closed with a running absorbable monofilament suture as is the 12 mm port site using an endo-close needle technique. The skin of all port sites and the access incision can be closed with subcuticular absorbable sutures.