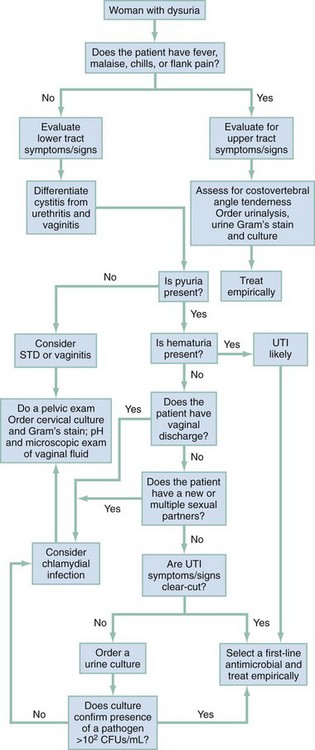
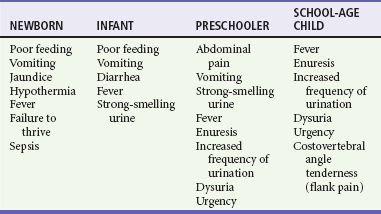
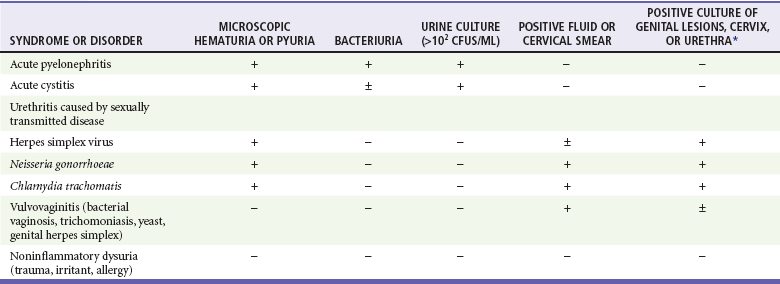
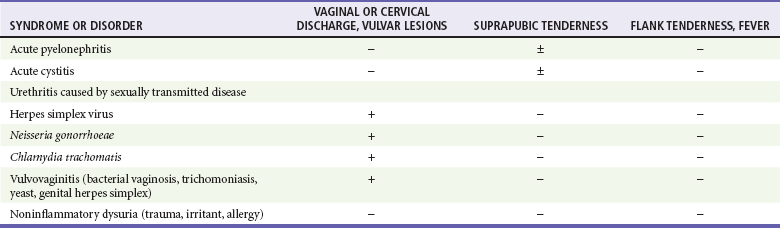
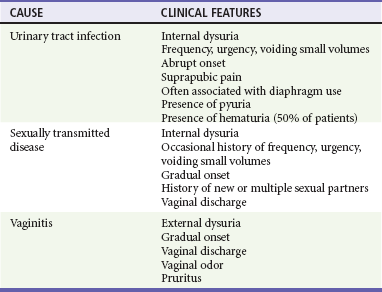
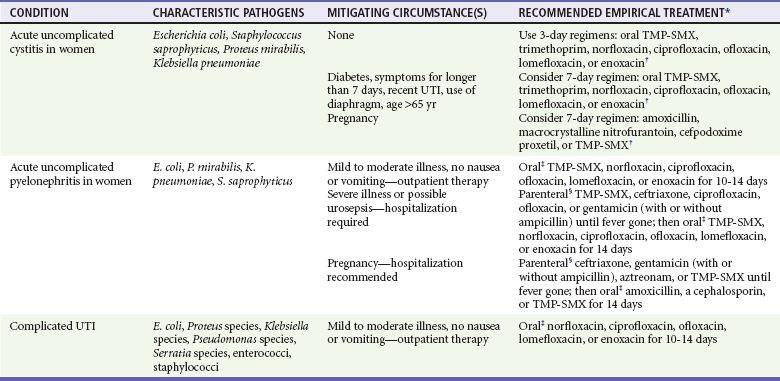
Chapter 99 Urinary tract infection (UTI) describes an inflammatory response of urothelium to microorganisms in the urinary tract, resulting in clinical symptoms including dysuria, frequency, urgency, hematuria, and suprapubic or costovertebral angle discomfort self-reported by the patient or elicited on physical examination. This term does not differentiate between upper and lower tract infections. Traditionally the emphasis has been on distinguishing lower tract from upper tract infections. Although this distinction may seem sensible from an anatomic perspective, it often does not provide additional information for making important management and disposition decisions. Bacteriuria is the presence of bacteria in the urine but is not considered to represent a UTI in the absence of clinical manifestations. Bacteriuria accompanied by symptoms should be treated, whereas bacteriuria in the absence of symptoms should be treated only in select patients (e.g., pregnant women, immunosuppressed patients).1 It is more useful to designate UTIs as being either uncomplicated or complicated, rather than as lower or upper tract infections. An uncomplicated infection is one involving a structurally and functionally normal urinary tract. The causative pathogen generally can be eradicated with a short course of standard antibiotics.2 This type of infection usually occurs in nonpregnant, sexually active, young women who have no evidence of an obstructive process. Complicated infection is that associated with underlying neurologic, structural, or medical problems, all of which may reduce the efficacy of standard antimicrobial therapy. These types of infections often require a prolonged course of antibiotic therapy and a more in-depth approach to testing and anatomic evaluation. UTI is a problem that affects all age groups.3,4 It is considered the most frequently occurring bacterial infection, accounting for 7 to 8 million annual outpatient visits, 1 million annual emergency department (ED) visits, 100,000 annual hospitalizations, and more than one third of all hospital-acquired infections.1,5 These statistics notwithstanding, gauging the actual extent of the disorder is very difficult because it is not a reportable disease in the United States and the definition of a UTI is not exact. Women have a 50% chance of experiencing a UTI during their lifetime.2 The annual incidence of UTIs is 2 to 4% among young, sexually active women and gradually increases to 5 to 10% by the age of 70 years and to approximately 50% by the age of 80 years. UTIs account for 5 to 14% of pediatric ED visits in the United States. UTI is more common in boys during the neonatal period but becomes more common in girls during infancy and thereafter.6 When a UTI is seen in preschool boys, it is almost always associated with congenital anomalies of the urinary tract. The overall risk for all children with unexplained fever having a UTI is 7 to 9%.7 UTIs in adult men are uncommon unless cystoscopy or catheterization has been performed. The prevalence is less than 1% from childhood through middle age but increases to 1 to 3% by the age of 65 years and to 10% by the age of 80 years. Among institutionalized men and women, prevalence rates for bacteriuria and UTI are increased to approximately 25% and 40%, respectively.3 UTIs associated with presence of an indwelling catheter constitute the most common nosocomial infection in the United States, accounting for more than 1 million cases annually.8 The urine is sterile along the entire urinary tract from the glomerulus to the external sphincter in men and to the bladder neck in women. The urinary tract maintains its sterility by means of various defenses. A major mechanism is complete emptying. Free, unobstructed flow of urine within the kidney and down the ureter, coupled with complete evacuation of the bladder, is essential. Abnormal anatomy or physiology or the presence of a foreign body may compromise host defense mechanisms and predispose the patient to infection.5 In women the urethra is short and opens close to the vulvar and perirectal areas. The organisms that cause UTI in women usually arise from the fecal reservoir and initially colonize the vaginal introitus and periurethral area.4 These factors contribute in part to the much higher incidence of UTI in women. Vesicoureteral reflux in children plays an important role in the pathogenesis of UTIs, particularly upper tract infections. Reflux caused by congenital abnormalities or by bladder overdistention (as seen in advanced prostatic hypertrophy) also predisposes affected patients to infection. Subgroups of patients who are more susceptible than the normal population to UTIs include diabetic patients, pregnant women, the elderly, patients with spinal cord injury and indwelling urinary catheters, patients with multiple sclerosis, and those with immunodeficiency disorders such as human immunodeficiency virus (HIV) infection.5 In young men, asymptomatic bacteriuria is rare and may signify urinary tract disease. UTIs in men generally begin to appear at 50 years of age (concomitant with the onset of prostatic hypertrophy) and slowly increase in incidence.9 The occurrence of UTIs in men of any age warrants referral to a urologist for further evaluation. The organisms that cause UTIs generally come from enteric flora colonizing the perineum and urethra. Escherichia coli is the dominant pathogen in more than 80% of first infections in women, men, and children, as well as in 50% of nosocomial UTIs.10 Staphylococcus saprophyticus, a coagulase-negative gram-positive organism, is the second most common pathogen in UTI and accounts for approximately 11% of cases.5 This species is present in normal skin flora, including the perineal area, but only in low numbers, and it does not appear to be of fecal origin. Occasionally, it is falsely identified as Staphylococcus albus or Staphylococcus epidermidis. Other, less common bacteria that may be responsible for infection include Proteus, Klebsiella, and Enterobacter.5 Unusual microorganisms may be found in institutionalized or hospitalized populations and with complicated UTIs. Such settings and conditions predispose the patient to alterations in the normal gastrointestinal (GI) flora, leading to complex UTIs. The uropathogens in these patients include more resistant strains of Escherichia, Klebsiella, Proteus, and Enterobacter, as well as Pseudomonas, Enterococcus, Staphylococcus, Providencia, Serratia, Morganella, Citrobacter, Salmonella, Shigella, Haemophilus, Mycobacterium tuberculosis, and fungi. Although not necessary with uncomplicated UTIs, urine culture and sensitivity testing are recommended for all patients with complicated UTIs. Antibiotic therapy based on the most likely pathogen should be initiated immediately. Uropathogenic organisms may elaborate various factors that affect their virulence, including aerobactin, hemolysins, and fimbriae (pili). Fimbriae, also called adhesions, are proteinaceous structures that can attach to specialized receptor sites on host cells. Attachment of bacteria to vaginal and uroepithelial cells ultimately leads to a higher incidence of UTI.11 UTI is suspected in adolescents and adults on the basis of clinical findings, including dysuria, frequency, urgency, and hematuria in the setting of suprapubic or costovertebral angle (CVA) discomfort. Symptoms and signs vary with age. In infants, initial manifestations may include irritability, fever, vomiting, diarrhea, and failure to thrive. Preschool children with UTI have vomiting, diarrhea, generalized abdominal pain, and febrile seizures. History of fever alone is not an adequate indicator of severity of infection in children because it may be historically absent in pediatric patients subsequently found to have significant renal scarring.12 As discussed previously, it is more important to determine if the infection is simple or complex. Simple, uncomplicated infections do not require urine culture, may be treated on an outpatient basis, and may not always necessitate urinalysis when thought to represent isolated cystitis.10 Complicated infections require urine culture with antibiotic sensitivity and also may necessitate inpatient therapy with further diagnostic evaluation.13 Distinction between upper and lower tract infections becomes important for understanding the differences in pathology and the pharmacokinetics of antibiotic delivery. Infection of the bladder generally involves only the superficial mucosa, and high urinary concentrations of antibiotics can easily be achieved with a short course of antibiotic therapy. The kidney, by contrast, tends to become infected in the medullary tissue, where achieving therapeutic concentrations of antimicrobial agents is far more difficult. As a result, parenteral antibiotics and longer courses of therapy are needed. Urine Collection Methods.: The diagnostic value of microscopic examination depends on the quality of the specimen obtained. In neonates and children younger than 6 months, urethral catheterization is the preferred method of urine collection. Aseptic technique ensures a low risk of introducing bacteria. Before catheterization is attempted in these younger patients, an ultrasound or bladder scanner can be used to confirm the presence of urine in the bladder. Suprapubic bladder aspiration is a reliable method if urine is available to be withdrawn, but it is less commonly used owing to the invasiveness of the procedure. For patients 12 months or younger, ultrasound-guided suprapubic bladder aspiration is a useful method and carries an incidence of adverse effects similar to that of urethral catheterization. Plastic bag collection is a reasonably reliable method, but the perineum (in girls) and the glans (in boys) should be properly cleansed before application of the bag. It is the least invasive method but is useful only if culture results are negative, because of high associated contamination rates. A clean-catch urine specimen is preferred in cooperative and continent male patients. Urinalysis.: Urine cultures constitute a majority of cultures performed by microbiology laboratories, and various screening tests have been developed for the purpose of reducing this burden and its attendant costs. The goal of urine screening tests is reliable selection of specimens that will provide negative cultures. This allows the laboratory to focus more appropriately on higher-yield studies. Urine Microscopy.: Urine microscopy is another commonly used method of providing rapid results, thereby reducing the number of urine cultures performed. Up to 96% of infected urine specimens contain 10 or more WBCs per cubic millimeter when counted by a hemocytometer. Various counting chamber methods detect pyuria with an accuracy approaching that of the hemocytometer. Unfortunately, these tests are not widely available, so direct microscopy commonly is used. Although no accepted level of pyuria is diagnostic of UTI, on careful quantitation with a hemocytometer chamber, pyuria will be found in nearly all cases of acute UTI caused by coliforms. In patients with a low-count coliform infection, those with fewer than 8 WBCs/mm3 of urine will have no demonstrable infection. In patients with more than 8 WBCs/mm3, 85% will have documented infection (by the presence of coliforms, staphylococci, or chlamydiae). Despite these controversies and limitations, microscopic examination of urine to identify bacteria remains the most readily available and reliable test for a presumptive diagnosis of UTI in most patient populations.14 Any analysis of a urine sample must be performed immediately after collection. Urine specimens that are allowed to sit for longer than 2 hours become alkaline, with subsequent dissolution of the cellular elements and multiplication of bacteria, thus providing the clinician with markedly unreliable results.15 Urine Culture.: Definitive diagnosis of UTI is based on isolation of significant numbers of bacteria on urine culture. Traditionally, 105 CFUs/mL has been used as the statistically significant number for the presence of UTI. However, use of an absolute number is fraught with limitations. The presence of 105 CFUs/mL of bacteria in cultures from urine is associated with a 95% likelihood of infection, whereas 104 CFUs/mL is associated with a 50% likelihood of infection. It makes best clinical sense to put these results in clinical context regarding the presence of symptoms suggestive of a UTI. The symptom complex of dysuria, frequency, urgency, and suprapubic pain may be caused by a wide variety of infectious organisms in numbers far less than the traditional 105 CFUs/mL. In addition, these same symptoms may represent a significant upper tract infection or may be caused by urethritis. The decision to perform a urine culture should be assessed for its relevance to patient care. Patients with frequency, dysuria, urgency, and suprapubic pain should be treated on the basis of symptoms if the infection is thought to be simple, and a urine culture is not required to guide therapy. For women who have host factors (e.g., structural abnormalities) or comorbid conditions (e.g., compromised immune status, pregnancy) necessitating definitive identification of the organism by culture, both urinalysis and culture are necessary. In general, the list of indications for urine culture (Box 99-1) defines high-risk groups. In vitro sensitivity testing contributes little to the general management of patients with uncomplicated UTI. Correlation between the therapeutic response and in vitro testing results often is poor. Culture also represents an additional cost with minimal contribution to the therapeutic plan for most outpatients. Imaging.: The majority of patients with acute cystitis or pyelonephritis do not need emergency imaging of the urinary tract. In certain clinical settings, however, emergency imaging is indicated. Patients with either unusually severe signs and symptoms or an atypical clinical presentation are candidates for genitourinary imaging. For example, a patient with the classic signs and symptoms of pyelonephritis but unremarkable urinalysis findings may have an obstructive process that has prevented the leukocytes and bacteria from reaching the bladder. Another example is that of a patient with a known history of UTI, currently receiving antibiotic therapy, who has persistent fever, chills, and general toxicity. Perhaps one of the most sensitive predictors of a complicated infection (e.g., abscess) is the persistence of fever beyond 72 hours after the institution of antimicrobial therapy. Pyelonephritis with obstruction from any cause can rapidly lead to abscess formation with resultant deterioration of renal function and sepsis. Emergency imaging is indicated to rule out this condition or to identify a suspected renal stone serving as a nidus for infection. Several imaging studies may be useful in these patients. Historically, intravenous or excretory urography—typically, intravenous pyelography (IVP)—was used because such studies provide both structural and functional information about the upper urinary tract. Recent work has focused on obtaining this information through safer, less invasive, and less costly methods.16 Ultrasonography compares favorably with IVP but is inferior to computed tomography (CT).17 Radionuclide cystograms compare favorably with voiding cystourethrograms in the diagnosis of vesicoureteral reflux and give less ionizing radiation to the gonads by a factor of 50 to 100. Voiding cystourethrography is the traditional method for initial evaluation of the genitourinary tract. CT scan is exceptional for diagnosing upper tract complications such as various degrees of pyelonephritis, abscesses, pyonephrosis, granulomatous infections, and infected cysts. As with IVP, its disadvantages include higher cost, radiation exposure, and potential for contrast-induced reactions. Ultrasonography.: Ultrasonography is useful in the evaluation of patients with potential urinary obstruction. It is a sensitive tool for detecting intrarenal and perinephric abscess and the presence of hydroureter and hydronephrosis. It is less accurate in determining the presence of a partially obstructing ureteral stone. Ultrasound examination also can detect the presence of pyelonephritis and congenital anomalies. Regardless of patient age group, this procedure is relatively inexpensive and avoids the hazards of contrast and radiation exposure. Intravenous Pyelography.: IVP, previously considered one of the mainstays in the evaluation of the genitourinary tract, has been nearly replaced by helical CT scanning and ultrasonography. IVP has higher sensitivity and specificity for determining the presence of obstruction than ultrasound examination but is inferior to CT scanning, and it is not sensitive for detecting the presence of pyelonephritis and renal abscess.18 Radionuclide Scans.: Radionuclide scans also are gaining popularity for the early evaluation of UTI. A dimercaptosuccinic acid scan is the most sensitive method of identifying pyelonephritis and is the imaging study of choice in infant girls with UTI and fever. Computed Tomography of the Abdomen.: A contrast-enhanced CT scan of the abdomen is perhaps the best test for assessing the kidneys, ureters, and bladder. It has the highest sensitivity for detecting abscess, obstruction, and acute inflammation.17 Its disadvantages include cost, radiation exposure, and potential for contrast-induced reactions and radiocontrast agent–induced acute kidney injury, which occurs infrequently in patients with a serum creatinine less than 1.5 mg/dL and can be further avoided by intravenous hydration with normal saline. CT without contrast can be performed in patients with renal insufficiency and is the preferred study in patients with clinical concern for urolithiasis. UTI during pregnancy represents a special situation. The incidence of UTI in pregnancy is approximately 2 to 7%.19 Maternal complications include acute pyelonephritis, increased incidence of postpartum chronic pyelonephritis, preterm delivery, and low newborn birth weight. The physiologic changes that occur within the urinary tract of pregnant women include ureteral and renal pelvis dilation, as well as reduced peristalsis throughout the collecting system. During the last trimester, minimal ureteral contractions occur in many patients. Diabetic patients with bacteriuria also have an increased risk for the development of pyelonephritis, but treatment of asymptomatic bacteriuria has not been proved to be beneficial and should not be standard therapy at this time.20 Papillary necrosis, perinephric and renal abscess formation, and emphysematous cystitis represent grave complications for this patient group. Manifestations of these complications may include altered vital signs, systemic signs and symptoms such as nausea and vomiting with dehydration, and a toxic appearance suggesting bacteremia and sepsis. These patients require aggressive fluid resuscitation, intravenous antibiotics, and a thorough diagnostic investigation including CT scanning. The prevention of catheter-associated urinary tract infections (CAUTIs) has become an area of recent interest in the hospital setting since the Centers for Medicare and Medicaid Services (CMS) identified this condition as one of the six unacceptable diagnoses for payment if UTI was not present on admission.21 CAUTIs are responsible for more than 80% of nosocomial UTIs and 40% of all nosocomial infections. Less than half of urinary catheters placed in hospitalized elderly patients have been found to be clinically indicated.22 The most effective strategy for addressing CAUTIs is to prevent the infection from occurring by placing urinary catheters only when indicated and considering the use of intermittent catheterization and condom catheters when appropriate. Bacterial UTI is the most common cause of dysuria with low-count infections. It is important, however, to consider the possibility of acute urethritis or acute vaginitis in these patients, as well as mechanical trauma or irritation (Tables 99-1 to 99-3; Fig. 99-1). Urethritis caused by Chlamydia may be seen in patients with acute dysuria; in fact, C. trachomatis may be present in up to 20% of women with dysuria. In general, if historical information includes contact with multiple sexual partners, a recent change in sexual partners, or a sexual partner with dysuria or discharge, C. trachomatis infection should be strongly considered. A pelvic examination should be performed, and culture specimens should be obtained to detect C. trachomatis and N. gonorrhoeae. Other causes of acute dysuria include infections with Trichomonas vaginalis and herpes simplex virus. Table 99-1 Differential Diagnosis of Dysuria Syndromes: Laboratory Findings *Positive for herpes simplex virus, Neisseria gonorrhoeae, or Chlamydia trachomatis. From Stamm WE: Protocol for diagnosis of urinary tract: Reconsidering the criterion for significant bacteriuria. Urology 32(Suppl 2):6, 1988. Table 99-2 Differential Diagnosis of Dysuria Syndromes: Physical Examination From Stamm W: Protocol for diagnosis of urinary tract: Reconsidering the criterion for significant bacteriuria. Urology 32(Suppl 2):6, 1988. Table 99-3 Clinical Differentiation among Major Causes of Dysuria From Stamm W: Protocol for diagnosis of urinary tract: Reconsidering the criterion for significant bacteriuria. Urology 32(Suppl 2):6, 1988. Simple Urinary Tract Infection Options for treating uncomplicated lower UTI include single-dose therapy, short-course therapy (3-5 days), and the more traditional 7- to 10-day course of therapy (Table 99-4). E. coli remains the most common urinary tract pathogen and is susceptible to many antibiotic regimens. Emerging resistance to TMP-SMX has been noted in 15 to 32% of organisms.23 In some areas of Europe, resistance to TMP-SMX is approaching 50%.24 Risk factors for UTI from TMP-SMX–resistant E. coli include recent use of antibiotics (especially TMP-SMX), recent travel to areas with a high prevalence of resistance, and age younger than 3 years with daycare attendance. Table 99-4 Treatment Regimens for Bacterial Urinary Tract Infections (UTIs) TMP-SMX, trimethoprim-sulfamethoxazole. *Treatments listed are those to be prescribed before the causative agent is known (Gram staining can be helpful); they can be modified once the agent has been identified. These recommendations are limited to drugs currently approved by the U.S. Food and Drug Administration, although not all of the regimens listed are approved for these indications. Fluoroquinolones should not be used in pregnancy. TMP-SMX, although not approved for use in pregnancy, has been widely used. Gentamicin should be used with caution in pregnancy because of its possible toxicity to eighth nerve development in the fetus. †Multiday oral regimens for cystitis are as follows: TMP-SMX 160-800 mg every 12 hr; trimethoprim 100 mg every 12 hr; norfloxacin 400 mg every 12 hr; ciprofloxacin 250 mg every 12 hr; ofloxacin 200 mg every 12 hr; lomefloxacin 400 mg every day; enoxacin 400 mg every 12 hr; macrocrystalline nitrofurantoin 100 mg four times a day; amoxicillin 250 mg every 8 hr; and cefpodoxime proxetil 100 mg every 12 hr. ‡Oral regimens for pyelonephritis and complicated UTI are as follows: TMP-SMX 160-800 mg every 12 hr; norfloxacin 400 mg every 12 hr; ciprofloxacin 500 mg every 12 hr; ofloxacin 200-300 mg every 12 hr; lomefloxacin 400 mg every day; enoxacin 400 mg every 12 hr; amoxicillin 500 mg every 8 hr; and cefpodoxime proxetil 200 mg every 12 hr. §Parenteral regimens are as follows: TMP-SMX 160-800 mg every 12 hr; ciprofloxacin 200-400 mg every 12 hr; ofloxacin 200-400 mg every 12 hr; gentamicin 1 mg/kg of body weight every 8 hr; ceftriaxone 1-2 g every day; ampicillin 1 g every 6 hr; imipenem-cilastatin 250-500 mg every 6-8 hr; ticarcillin-clavulanate 3.2 g every 8 hr; and aztreonam 1 g every 8-12 hr. Adapted from Stamm W, Hooton TM: Management of urinary tract infections in adults. N Engl J Med 329:1328, 1993. Three days of therapy is more effective than single-dose therapy.25 Three days of therapy have the advantages of improved compliance, lower cost, and reduced side effects. It currently is the recommended regimen for treatment of uncomplicated lower UTI. Despite emerging resistance, TMP-SMX remains the best first-line agent for 3-day regimens when compared with other commonly used antibacterials, owing to its low cost and effectiveness. Short-course 3-day therapy also is effective for asymptomatic bacteriuria in pregnancy. It is unclear whether this regimen can be used for symptomatic lower UTIs in pregnancy, so longer-course therapy is recommended. A regimen of 7- to 10-day therapy generally offers no benefit over shorter courses in uncomplicated UTIs; however, it remains the standard of care in complicated infections (in patients with pregnancy, diabetes, or sickle cell anemia) for which cure rates are lower with shorter regimens. The fluoroquinolones are considered first-line agents in regions in which the incidence of TMP-SMX resistance has approached 10 to 20%. Ciprofloxacin is the most commonly used drug and requires twice-daily dosing. Although more expensive than ciprofloxacin, gatifloxacin and levofloxacin offer once-daily administration, have the broadest activity, and have same-dose bioequivalence between oral and parenteral administration. Fluoroquinolones damage developing cartilage in animal studies and should be avoided in children.26 Mild-to-moderate pyelonephritis can be safely treated on an outpatient basis with a fluoroquinolone for 10 to 14 days (first-line agent) or TMP-SMX (second-line agent) as long as the patient is able to eat and drink, has achieved adequate pain control, and has appropriate social support in the home. In many clinical centers, observation units have evolved to offer a short-stay (less than 24 hours) option for moderate cases in which immediate discharge for outpatient therapy may not be the optimal approach to management.20 UTI is a major bacterial disease of childhood; it is estimated that 0.8 to 1.5% of children have bacteriuria. The risk for development of UTI before 11 years of age is 3% in girls and 1% in boys.6 The incidence of UTI in the neonatal period is higher in boys, but the infection becomes more prominent in girls during infancy and thereafter. In children aged 1 to 3 months, UTI is associated with a high incidence of sepsis (30%).7 After the age of 3 months, the incidence of sepsis associated with UTI decreases (to 5%). Vesicoureteral reflux is a common risk factor for UTI and renal scarring in children.12 Data suggest that the incidence of scar formation after acute pyelonephritis may be as high as 37%. As in adults, E. coli is the predominant pathogen.6 Age-related differences are recognized: In older boys Proteus often is isolated during UTI, whereas in newborn children, Klebsiella is more often the causative agent. The route of infection also is age related. It is thought that in the newborn period the bacteria are blood-borne (and often associated with generalized sepsis). In the older age group, as in adults, the ascending urethral route is primarily responsible for generating infection of the urinary tract. UTI often is overlooked in children because of inappropriate emphasis on classic signs and symptoms, with little regard to age variables. Nonspecific findings should be considered the rule and not the exception (Table 99-5). Pyelonephritis may be present without overt symptoms. A UTI in a febrile patient usually indicates pyelonephritis. An elevated blood urea nitrogen (BUN) level or hypertension in a child older than 2 months strongly suggests bilateral hydronephrosis or advanced renal parenchymal disease. Generalized septicemia often is the major manifestation of neonatal UTI.12 Classically, feeding difficulties, irritability, and sluggishness are seen in this age group. Bacteremia is present in nearly 50% of cases.6 Laboratory studies useful for diagnosing an infection of the urinary tract as previously described also apply to children. However, presumptive treatment may be indicated in high-risk patients based on clinical predictors and screening tests, as shown in Figure 99-2. Additional studies are dictated by the clinical setting and include renal function studies, a complete blood count, serum electrolyte panel, CT scan, voiding cystourethrography, and ultrasonography. Renal cortical scintigraphy is the most sensitive method of detecting pyelonephritis. As in adults, many therapeutic options are available for children with UTI. Sulfonamides, nitrofurantoin, TMP-SMX, cephalosporins, and aminopenicillins are effective.6 Newborns and young infants should be treated with ampicillin and gentamicin on an inpatient basis. Sulfonamides and fluoroquinolones should be avoided in pediatric patients. Traditionally, inpatient treatment with parenteral antibiotics has been the standard of care for young children with suspected pyelonephritis. Oral therapy is acceptable in children with uncomplicated infections. These patients should be managed conservatively, and hospital admission is advised for children who are dehydrated, severely ill, or not tolerating oral fluids and for those with underlying structural abnormalities of the genitourinary system. In addition, family dynamics, which could affect compliance with medication, should be taken into consideration. Cystitis is rare in male patients in the absence of blunt trauma, prostate pathology, or instrumentation.3 Chronic prostatitis, prostatic hyperplasia with obstruction, and previous instrumentation are the most common predisposing factors. Lack of circumcision and homosexuality are other recognized risk factors. Commonly, men with cystitis have symptoms of urinary urgency, frequency, dysuria, nocturia, suprapubic pain, and often low back pain. Gross hematuria occasionally occurs, but fever, chills, and flank pain generally are absent. On physical examination, suprapubic tenderness to palpation may be elicited. Pneumaturia may be present and is indicative of an infection with gas-forming bacteria. It also may indicate the presence of a vesicoenteric fistula, which often is caused by diverticulitis, although rectosigmoid carcinoma and regional enteritis are associated diseases as well. If fever and chills are present in association with irritative symptoms and difficulty voiding, acute bacterial prostatitis should be strongly considered. The most common pathogens found in men with cystitis are E. coli, Proteus, and Providencia. Three qualifying factors should be addressed in dealing with UTIs in men: 1. Obstruction. It is imperative that urinary obstruction be ruled out as a pathogenic mechanism. Infection and obstruction together can be catastrophic and lead to sepsis. Obstruction at the level of the prostate in older men is common and should be considered. Catheterization or bedside ultrasound examination may help to rule out retention. Suggestion of obstruction of the upper tracts based on lack of response to medical therapy necessitates performance of an abdominal noncontrast CT scan or ultrasound. 2. Genitourinary tract anomalies. UTIs in men may be secondary to underlying diseases of the genitourinary tract. Therefore all of these patients should be referred to a urologist for diagnostic studies. 3. Catheterization. Urethral catheterization should not be used to collect a urine specimen in men unless they are experiencing urinary retention. An inability to produce a specimen in the presence of infectious symptoms should be a major clue regarding the cause of the infection. If retention is suspected, catheterization for collection of residual urine is indicated. Referral for urologic consultation is recommended and hospital admission is prudent for a majority of these patients. Antimicrobial therapy has been shown to be beneficial and is recommended.27 In patients without signs of systemic toxicity, a prolonged course of an antibiotic for 4 to 6 weeks is required. This may need to be repeated if only partial success is achieved. The following list represents an appropriate selection of drugs for nontoxic prostatitis: 1. Ciprofloxacin 500 mg orally (PO) twice daily; norfloxacin 400 mg PO twice daily; ofloxacin 400 mg PO twice daily or enoxacin 400 mg PO twice daily for 30 days 2. Trimethoprim with sulfamethoxazole (Bactrim), one double-strength tablet PO twice daily for 30 days 1. Ciprofloxacin 400 mg intravenously (IV) every 12 hours, or levofloxacin 500 mg IV every 24 hours 2. Ceftriaxone 2 g IV every 24 hours with or without gentamicin 3 to 5 mg/kg/day Some experts have recommended alpha-blocker therapy because the bladder neck and prostate are rich in these receptors and alpha-blockade may improve outflow obstruction and diminish prostatic reflux. Although this may facilitate the patient’s recovery course, clinical trials are ongoing and this is not considered standard of care.28 Patients with chronic prostatitis typically visit the ED when they experience an acute exacerbation of the disease. Clinical manifestations vary widely, but most patients report some degree of irritative voiding symptoms (frequency, urgency, dysuria), low back and perineal pain, and occasionally myalgias.27 Fever and chills are uncommon except during an acute exacerbation of the chronic infection. A history of previous episodes of acute prostatitis may be absent. Findings on the physical examination, including examination of the prostate, often are unremarkable. The hallmark of chronic bacterial prostatitis is relapsing UTI caused by the same organism. Chronic bacterial prostatitis is the most common cause of recurrent UTI in men. Antimicrobial therapy is recommended for the treatment of chronic prostatitis.29 Most antimicrobials diffuse poorly from plasma into prostatic fluid. The fluoroquinolones achieve the highest concentrations in the prostate and are the drugs of choice, with cure rates of approximately 64%. The recommended dosages are as follows: ciprofloxacin 500 mg twice daily for 30 days; norfloxacin 400 mg twice daily for 30 days; enoxacin 400 mg twice daily for 30 days; or ofloxacin 300 mg twice daily for 6 weeks. TMP-SMX also is useful, with cure rates of 44 to 50%. The dosage is one double-strength tablet twice daily, but the optimal duration of therapy is unclear and may range from 4 to 16 weeks. Urolithiasis constitutes a common clinical problem seen in the ED and affects 5 to 15% of the population worldwide, and recurrence rates are close to 50%.30 From 1994 through 2000, presentations for urolithiasis nearly doubled, and all indicators point to a rise in the incidence of kidney stones in the general population.31 Renal calculi are seen commonly in young adults and middle-aged men, with nearly 70% of all ureteral calculi occurring in individuals aged 20 to 50 years. Most ureteral calculi originate in the kidney and then pass into the collecting system. Various clinical syndromes involve metabolic alterations and are therefore associated with an increased likelihood of stone formation32 (Box 99-2). Risk factors include age, male gender, and family history. In the United States, prevalence rates for renal calculi are 10% in men and 5% in women.33
Selected Urologic Problems
Urinary Tract Infections
Background
Epidemiology
Principles of Disease
Pathophysiology
Bacteriology
Clinical Features
Diagnostic Strategies
Complicated Urinary Tract Infection in High-Risk Populations
Diabetes and Sickle Cell Disease
Indwelling and Temporary Urinary Catheters
Differential Considerations
Management
Complex Urinary Tract Infection
Urinary Tract Infection in Children
Principles of Disease
Clinical Features
Neonates
Diagnostic Strategies
Management and Disposition
Urinary Tract Infection in Men
Specific Disorders
Prostatitis
Chronic Prostatitis
Renal Calculi
Background
Epidemiology
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Anesthesia Key
Fastest Anesthesia & Intensive Care & Emergency Medicine Insight Engine