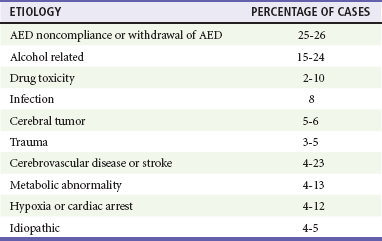
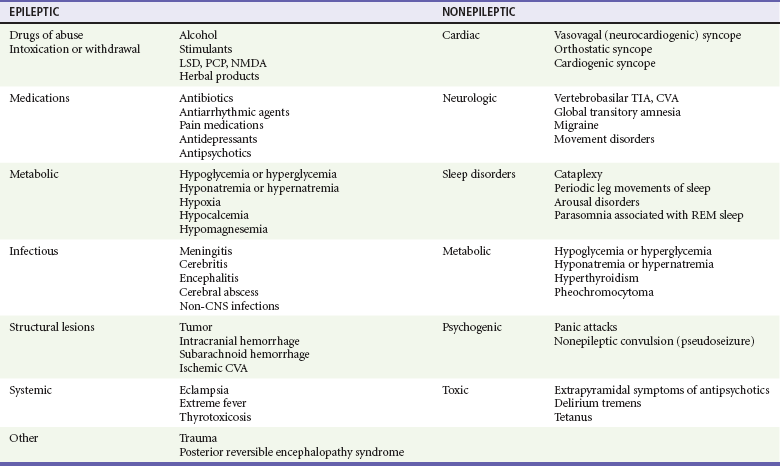
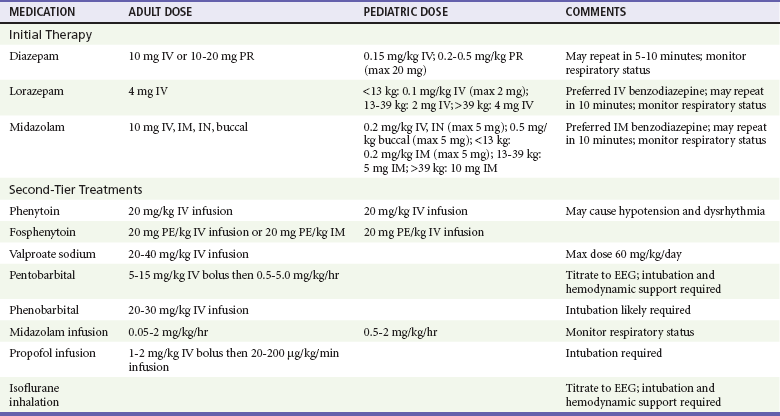
Chapter 18 Seizures are episodes of abnormal neurologic functioning caused by pathologically excessive activation of neurons, either in the cerebral cortex or in the deep limbic system. Epilepsy is defined as recurrent unprovoked seizures caused by a genetically determined or acquired brain disorder1; it is not an appropriate term for seizures that occur intermittently or predictably after a known insult, such as alcohol intoxication and withdrawal. More than 10% of the United States population will experience at least one seizure during their lifetime; however, only 3% will be diagnosed with epilepsy. Seizures account for 3% of transports by emergency medical services, 2% of pediatric ED visits, and 1% of all ED visits. Alcohol and central nervous system pathologies (tumor, stroke, trauma, infection) are common causes in adults. Metabolic derangements and infection more frequently cause seizures in infants than adults, but febrile seizures are the most common type of seizure in infants and young children. Approximately 7% of patients who come to the ED with seizures are in status epilepticus.2 Seizures can be classified based on cause (primary or secondary), effect on mentation (generalized or focal), and motor activity (convulsive or nonconvulsive). Primary seizures are unprovoked and not linked to an inciting event. Secondary seizures may be caused by trauma, illness, intoxications and poisonings, organ failure, other metabolic disturbances, cerebral tumors, pregnancy, and, paradoxically, supratherapeutic levels of some anticonvulsants.3,4 A newer terminology scheme has been developed and may affect communications between emergency physicians and epileptologists or patients. The “partial” classification is now solely “focal,” and the distinctions between “complex partial” and “simple partial” have been eliminated. The terms genetic, structural-metabolic, and unknown have replaced idiopathic, symptomatic, and cryptogenic.3 A generalized seizure is defined as abnormal neuronal activity in both cerebral hemispheres causing an alteration in the level of consciousness. Generalized seizures may be further divided into tonic-clonic, absence, atonic, and myoclonic; some patients may experience only the tonic or clonic phase. Focal seizures usually involve one cerebral hemisphere, thereby preserving consciousness, though these seizures may progress and cause an altered sensorium. Some seizures are impossible to classify because of inadequate or inaccurate description of the ictal activity.3,4 Status epilepticus has been classically defined as at least 30 minutes of persistent seizures or a series of recurrent seizures without intervening return to full consciousness.5 The time criterion has been shortened to 5 minutes with recognition that the duration of seizure activity is related to outcome and that the likelihood of achieving seizure cessation with typical treatments decreases with ictal duration.4,6 Common causes of status epilepticus in adults are shown in Table 18-1.7 Table 18-1 Etiology of Status Epilepticus in Adults Adapted from Bassin S, Smith TL, Bleck TP: Clinical review: Status epilepticus. Crit Care 6:137-142, 2010. Seizures in children follow a different distribution, primarily because of the relatively high incidence of febrile seizures and the inherent limitations of the observational history of possible ictal activity. Febrile seizure is the most common pediatric seizure, occurring in 2 to 5% of children 6 months to 5 years of age; 20 to 30% of those children have at least one recurrence. It is important to differentiate between the febrile seizure, which is typically of short duration, has a limited postictal phase, and is related to the slope of the body temperature rise, and the seizure with fever, which is often more serious and prolonged and indicates more significant underlying infection.8 First-time seizures in infants younger than 6 months may indicate important underlying pathology and necessitate a full assessment.9 Seizures occur when the abnormal increased electrical activity of initiating neurons activates adjacent neurons and propagates until the thalamus and other subcortical structures are similarly stimulated. At a cellular level, the pathophysiology is not well understood, although research in specific epilepsy syndromes is elucidating possible mechanisms. Investigation of rare inherited epilepsy syndromes has identified mutations in neuronal ion channel proteins, limiting intracellular passage of potassium. Given that the potassium current is the primary force behind repolarization of membranes, depolarization is prolonged in these patients, leading to an increase in neuronal hyperexcitability.1 Other studies have found that malformations of cortical development and glial cells may play a role in epileptogenesis.1 Focal seizures may represent a similar pathophysiologic process in which less recruitment occurs and the ictal activity does not cross the midline. Because of the more limited focus of abnormal activity, convulsive motor activity may not be the predominant clinical manifestation.10 Because a diagnosis of seizure has major consequences for the patient in the ED—including loss of driving privileges and exposure to potentially toxic medicines—the first diagnostic task is to determine whether the patient actually experienced a seizure.11,12 Ictal activity can be irrefutably verified only by electroencephalography. Other abnormal movements and states of consciousness, including nonepileptic convulsions (pseudoseizures), can be confused with ictal activity. The differential diagnoses to consider when evaluating for seizure are listed in Table 18-2.12 Table 18-2 Differential Considerations for the Diagnosis of Seizure Adapted from Carreno M: Recognition of nonepileptic events. Semin Neurol 28:297-304, 2008; and Slattery DE, Pollack CV Jr: Seizures as a cause of altered mental status. Emerg Med Clin North Am 28:517-534, 2010. Syncope, whether vasodepressive (vagal syncope), orthostatic, or dysrhythmia related, can be confused with seizures by observers. A sudden loss of consciousness followed by abnormal movements can be ictal or syncopal in origin, hence the consideration “fit versus faint.” One video analysis of 56 brief syncopal episodes showed myoclonic activity in 90% of patients, together with frequent head turns, upward gaze, oral automatisms, and righting movements. These are likely a transient response by the brain to sudden deprivation of blood flow. In general, ictal tonic-clonic movements are more forceful and prolonged than the brief convulsive activity sometimes associated with fainting. In addition, most generalized seizures are characterized by a postictal state that syncope patients do not manifest.13 An important exception to this is an atonic seizure, or “drop attack,” in which the patient experiences a sudden and complete loss of muscle tone associated with altered mentation; in this type of generalized seizure, motor activity is not displayed and a postictal state may not occur.4 The cause of an unwitnessed, unprovoked loss of consciousness with a fall, after which the patient visits the ED, may be difficult to determine. Suggestions of seizure as the cause include retrograde amnesia, loss of continence (which also can occur with vasogenic and other forms of syncope), and evidence of oral trauma such as maceration of the buccal mucosa or bite lacerations of the tongue. Blood drawn soon after a true seizure may demonstrate a lactic acidosis that may resolve by the time a repeat analysis is performed in the ED.14 The patient who arrives with a history of possible seizure activity should be placed in a monitored area of the ED and prepared for prompt physician examination.5 An intravenous line or saline lock catheter should be placed in case anticonvulsants are emergently indicated. Blood glucose is checked at the bedside, and a thorough list of all medications currently being used by the patient is obtained. Hypoglycemia is the most common metabolic cause of seizure activity. The only treatment required for the patient may be administration of intravenous glucose. Prolonged seizure activity may also cause hypoglycemia, so the cause-and-effect relationship may sometimes be reversed; but in either case, glucose therapy is required. If the patient stopped seizing before arrival in the ED, the history, physical examination, and diagnostic course should focus on possible precipitants of the seizure. The patient should be protected from self-injury during this time. Most seizures will terminate without intervention. If a patient begins to seize while under ED observation, it is prudent to administer low-dose benzodiazepines (approximately half of the doses for status epilepticus, Table 18-3). Patients who arrive at the ED with continued seizure activity, experience recurrent seizure without recovering from the postictal period, or experience witnessed convulsions lasting longer than 5 minutes are considered in status epilepticus and treated as indicated in Table 18-3. Table 18-3 Medications and Dosages for Emergency Treatment of Prolonged Seizures and Status Epilepticus Intraosseous administration is an acceptable alternative for intravenous medications. Adapted from Brophy GM, et al: Guidelines for the evaluation and management of status epilepticus. Neurocrit Care 17:3-23, 2012.
Seizures
Perspective
Epidemiology and Classification
Pathophysiology
Diagnostic Approach
Rapid Assessment and Stabilization
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Seizures
Only gold members can continue reading. Log In or Register to continue




