Key Clinical Questions
Introduction
A seizure is defined as a sudden attack of involuntary behavior or experiences resulting from abnormal cortical neuronal activity. About 5% of the population of the United States will experience one at some point during their lifetime. Epilepsy, the chronic disease defined by the occurrence of two or more unprovoked seizures, is seen in approximately 2 million to 4 million people in the United States alone. The World Health Organization (WHO) reports that in primary care settings worldwide, epilepsy is the second most common neurologic condition, after headache.
Triage and Hospital Admission
Epilepsy and seizures are also common in the inpatient setting. In a large multicenter study in both community and academic hospital emergency departments, 1.2% of 31,508 patient visits were related to seizures. Overall, 27% of these patients were admitted. Of those patients suspected of having new-onset seizures, 63% were admitted. Reasons for admission for patients with seizures include diagnostic evaluation (especially when the diagnosis of seizure is unclear), uncontrolled seizures, toxicity from antiepileptic drugs (AEDs), and injuries sustained during a seizure.
Classification and Clinical Findings
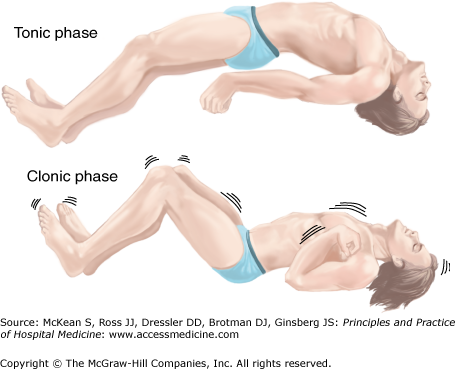
Seizures are classified into two broad categories: primary generalized and partial (Table 212-1). Generalized seizures by definition are characterized by loss of consciousness. Absence seizures are typically brief staring spells, lasting seconds. These usually begin in early childhood and remit in adolescence in childhood, but they may persist into adulthood. Patients with myoclonic epilepsy have quick jerking movements, most often in the morning after awakening. They are often not diagnosed until a generalized tonic-clonic seizure occurs. Generalized tonic-clonic seizures, also known as convulsions, are recognized by tonic extension of the extremities, followed by clonic jerking (Figure 212-1). Variations of these include generalized seizures with either a primarily tonic or clonic component. Atonic seizures are characterized by sudden loss of tone. These patients are especially prone to injuries as a result of falling without warning.
Figure 212-1
Generalized tonic-clonic seizure. In the tonic phase (top), lasting 10 to 30 seconds, the patient has tonic muscle contractions leading to flexion, then extension, of the neck and trunk. The vocal muscles contract, and the patient may cry out and become cyanosed. Jaw contraction may lead to tongue injury. This is followed by the clonic phase (bottom), with symmetric muscle contraction and relaxation that produces limb jerking. The clonic phase diminishes in intensity and usually ends after approximately one minute. (Reproduced, with permission, from Simon RP, Greenberg DA, Aminoff MJ. Clinical Neurology. 7th ed. New York: McGraw-Hill, 2009. Fig. 8-2.)
Partial seizures start with abnormal neuronal discharges in a limited area of the cerebral cortex. The site of the ictal focus dictates the clinical symptoms during the seizure. Any partial seizure can progress into a generalized seizure if the epileptic activity spreads to involve both hemispheres. Partial seizures are subclassified into simple and complex. During a complex partial seizure, the patient loses awareness of his or her surroundings. Typical symptoms in temporal lobe seizures include staring, walking aimlessly, and automatisms such as lip smacking or picking at clothes or bedsheets. Patients may experience epigastric rising or nausea, anxiety, déjà vu, visual distortion, or olfactory hallucinations. Seizures are typically one to three minutes in duration and are almost always less than 30 minutes long. Conversely, a patient with a simple partial seizure is awake and aware throughout the event. Clinical features may include hemibody clonic movements, déjà vu, or visual or olfactory hallucinations.
Did This Patient Have an Epileptic Seizure?
When called upon to care for a patient with a seizure, the first question the hospitalist must ask is whether the “seizure” was epileptic or not. Many types of physiologic events are characterized by episodes of loss of consciousness or awareness. Common conditions that can mimic seizures are listed in Table 212-2. Answering this crucial first question begins with obtaining a clinical history. Vital points of the history include:
Was the event paroxysmal? Epileptic seizures are always sudden in onset. This is also true of some, but not all, of the mimickers of seizures, so that this information alone cannot distinguish epileptic seizures from nonepileptic spells.
Was the episode provoked? Common triggers for epileptic seizures include sleep deprivation, concomitant systemic illness, drug intoxication or withdrawal, and flashing lights. Syncope often follows a change in posture, micturition, or a sudden fright.
Was there a clinical prodrome? A seizure may begin with an aura of focal neurologic symptoms or signs. The aura may consist of obvious behavior changes, such as focal motor jerking or staring off with oral automatisms. It may also be a purely internal experience for the patient, including visual or olfactory hallucinations, focal sensory changes, déjà vu, or a subjective “feeling” that the patient cannot describe well. An epileptic aura is stereotypic for any given patient. It is typically short in duration, lasting seconds to one to two minutes. Conversely, if present, a prodrome to nonepileptic events is usually described as lightheadedness or just not feeling well. This can last minutes and sometimes even hours.
What were the clinical features of the event? The appearance and actions of the patient during the event are critical pieces of information. Certain clinical features can help differentiate epileptic seizures from nonepileptic events, as noted in Table 212-3. Some are more specific than others. For example, tonic posturing is often seen in focal seizures emanating from the frontal lobe, but it is rare in nonepileptic events. Tongue biting, traditionally considered a reliable sign of a generalized seizure, occurs in less than 30% of convulsions, but may also occur in psychogenic spells. Similarly, urinary incontinence is not specific to epileptic seizures. Bizarre behavior, such as flailing or thrashing movements, is often labeled psychogenic. However, this can also be seen in physiologic events, including frontal lobe epileptic seizures and some sleep disorders, as listed in Table 212–2. Fear or anxiety, the hallmark of panic disorder, is common in complex partial seizures emanating from the amygdala. Hallucinations, especially visual, are common in migraine, but they are also common auras in temporal lobe complex partial seizures. Unresponsiveness is common after both epileptic seizures and nonepileptic attacks. The duration may be helpful in making the distinction. Postevent unresponsiveness is typically shortest (seconds to one minute) with syncope, is longer in epileptic seizures (up to 30–60 minutes), and longest with psychogenic events where “unresponsiveness” can last hours. However, with prolonged unresponsiveness, subclinical status epilepticus must always be ruled out.
When trying to decide whether a spell is a seizure or nonepileptic event, remember that not all that shakes or jerks is epileptic. Myoclonus, characterized by quick, sudden jerks, is common after cerebral hypoxia and anoxia, as well as in metabolic disorders, such as hepatic and renal dysfunction. Myoclonus is seldom epileptic and should not be mistaken for primary epileptic seizures.
What is the patient’s medical history? A history of diabetes, renal failure, or liver disease should raise the clinician’s suspicion that the event in question was a seizure provoked by a systemic metabolic disturbance. A patient with cancer who has an episode of altered awareness should be evaluated for brain metastases causing a focal or generalized seizure. Cardiac or vascular disease favors the diagnosis of syncope. In patients with psychiatric disease, it should not be assumed that the presenting “seizure” is psychogenic in origin. Adult patients with mood disorders are 1.7 to 7 times more likely to develop epilepsy than those without a psychiatric history. In addition, some antidepressants and antipsychotic medications can provoke seizures. Thus, it is incumbent on the hospitalist to exclude all other physiologic conditions before a diagnosis of pseudoseizure is made.
The value of an accurate history and description of a seizurelike event cannot be overestimated. This information is often elusive when a patient is cognitively impaired or postictal. The hospitalist must be dogged in the pursuit of history from family or witnesses to the event in order to avoid a misdiagnosis.
|
| Clinical Sign or Symptom | Epileptic | Nonepileptic |
|---|---|---|
| Appearance | Flushed or cyanotic | Pale, diaphoretci |
| Motor movements | Rhythmic tonic-clonic jerks | Complex tonic posturing |
| Tonic extension | Myoclonus | |
Sudden onset flailing/thrashing Repetitive rocking | Nonrhythmic jerking | |
| Lip smacking | ||
| Nonpurposeful picking/slapping | Non-sudden onset flailing/thrashing | |
| Head turning | ||
| Eye deviation | ||
| Fencing posture | ||
| Subjective experience | Stereotypical olfactory, gustatory, | Tunnel vision |
| visual, or aural (rare) hallucination | Light-headedness | |
| Rising in stomach | Palpitations | |
| Déjà vu | ||
| Fear or anxiety | ||
| Tongue biting | Can occur but < 50% | Rare but can occur |
| Urinary incontinence | Can occur | Can occur |
| Sensory changes | Positive feeling (ie, paresthesias, dysesthesias) | Negative feeling (ie, numbness) |
| Postevent state | Confusion | Unresponsive < 5 min |
| Agitation | (prolonged unresponsiveness sometimes seen in psychogenic seizures) | |
| Unresponsiveness usually < 1 h | ||
| Headache | ||
| Extreme fatigue |
|
When evaluating a patient with a spell, the physical examination is most helpful during or immediately after the event. Ongoing subtle motor movements should lead to consideration of nonconvulsive status epilepticus. Elevated blood pressure or increased heart rate is common not only in convulsions but also in partial seizures. An irregular pulse more likely reflects a cardiovascular syncopal event, although autonomic dysfunction can also be seen with seizures. Focal neurologic deficits such as hemiparesis and hemiparesthesias are typical in focal cerebral ischemia, such as a transient ischemic attack (TIA). However, these deficits can also be seen after a partial seizure (postictal Todd paralysis). Thus, although the physical examination by itself is seldom diagnostic, in combination with the clinical history, it can help distinguish epileptic from nonepileptic spells.
|
Electroencephalography (EEG) is still the gold standard used to distinguish epileptic seizures from nonepileptic events. However, it is only definitive if the patient has an event during EEG recording. Only approximately 30% of patients with chronic unprovoked seizures show epileptiform activity on routine EEG. If done within 24 to 48 hours of a seizure, some studies have shown that the yield increases to up to 70%. About 2% to 3% of healthy adults have a false-positive EEG. Overall, a positive EEG may be helpful in ascertaining whether an event was epileptic, especially if done within 24 to 48 hours of the spell. A negative study is not helpful.
Perhaps the most vexing diagnostic problem for the hospitalist faced with a patient with an attack of altered consciousness is distinguishing a syncopal attack from an epileptic seizure. Overall, syncope is much more common than seizures, especially in elderly patients, who comprise a large portion of the hospitalist’s practice. A thorough history of the paroxysmal event provides the most reliable data in differentiating seizures from syncope. Clinical features useful in making the distinction between these two types of episodes are presented in Table 212-4. Findings on physical exam may help in the differential diagnosis, with abnormal cardiac findings suggesting syncope and focal neurologic signs more likely associated with seizures. Beyond the history and physical, diagnostic tests are surprisingly of little yield. An electrocardiogram (ECG) is abnormal in only approximately 7% of patients who present to the emergency department with syncope. Despite this statistically low yield, it is recommended that all adult patients who present with an episode of altered consciousness have an ECG.
| Favors Syncope | Favors Seizures |
|---|---|
| Pallor, diaphoresis | Flushed, cyanotic |
| Lightheadedness, dizziness | Head turning |
| Chest pain | Unusual posturing |
| Palpitations | Unusual behavior |
| Vertigo | Tongue biting |
| Nausea | Limb jerking |