Screening for Skin Cancers
Arthur J. Sober
Peter C. Schalock
Neoplasms of the skin are among the most common cancers in humans and a source of considerable morbidity and mortality, which are largely avoidable by preventive measures and timely diagnosis and treatment. More than 2 million new skin cancers occur annually in the United States, accounting for more than 10,000 deaths. Screening for these tumors is important because they are relatively easy to diagnose in early stages, when cure is possible by simple measures; this is particularly true for melanoma. In the last decade, the incidence of melanoma in the United States has approximately doubled and overall is increasing more rapidly than that of nearly any other cancer.
Basal Cell Carcinomas
Basal cell carcinomas (BCCs) are the most common malignancy in humans. They are distinctly sun related, with the majority occurring on the head and neck, especially the nose and cheeks. Recently an increase in frequency has been seen on the male torso and on the legs of women. Other etiologic factors include a genetically transmitted autosomal dominant disorder—the basal cell nevus syndrome—in which multiple basal cell carcinomas occur in relatively young persons in association with palmar pits, bone cysts, and frontal bossing. Previously identified BCC is also a risk factor.
Once a single basal cell carcinoma has developed, the chance that a second one will develop ranges from 36% to 50%. This observation forms the basis of annual follow-up examinations after basal cell carcinoma has been detected.
Squamous Cell Carcinomas
Most squamous cell carcinomas develop from the precursor lesion—actinic keratosis. Two thirds of these cancers occur on sun-exposed surfaces, with risk proportional to total accumulated sun exposure. Other precipitants include arsenic ingestion, radiation-induced scarring, and thermal burns. Those lesions arising in sun-damaged skin usually behave in a less biologically aggressive fashion than do those that occur on non-sun-exposed or mucosal surfaces and are less likely to metastasize.
Melanoma
Melanoma, although far less common than are basal cell carcinoma and squamous cell carcinoma, accounts for more than 75% of skin cancer deaths. The incidence has been increasing rapidly during the last few decades and currently exceeds that of Hodgkin disease, leukemia, pancreatic cancer, carcinoma of the thyroid, and carcinoma of the pharynx and larynx. The sex ratio for melanoma in the United States is approximately 1:1 with a modest male predominance. A second primary melanoma develops in up to 10% of nonfamilial patients; 10% have affected relatives.
Risk Factors and Precursors
Because of the rapid rise in melanoma incidence, attention has focused on melanoma risk factors and precursors. Persons with fair skin who tan poorly and burn easily are at greatest risk, especially those with a history of episodic, intense sun exposure. Blacks, Asians, and dark-skinned Whites have a much lower risk.
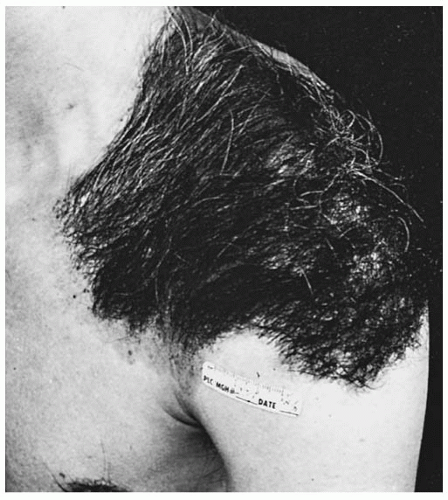
Precursor lesions include congenital nevi and dysplastic nevi (i.e., clinically atypical moles). Although congenital nevi occur in approximately 1% of all newborns, fortunately most of these are small (≤1.5 cm in diameter). Melanoma risk has been most clearly associated with large (>20 cm) nevi. Giant hairy nevus (Fig. 177-1) is a form of congenital nevus associated with malignant degeneration; the overall lifetime risk for malignancy is about 6%. Melanomas may arise in these lesions at any time throughout life, but most often by age 10 years. Melanoma occasionally arises in smaller pigmented congenital nevi, but the exact risk is unknown.
Dysplastic nevi occur in 5% to 10% of light-skinned Whites and usually are recognizable in early adolescence. Lifetime risk for melanoma is elevated severalfold in individuals with dysplastic nevi. An inherited predisposition to dysplastic nevi may contribute to the 8- to 12-fold increase in melanoma risk among first-degree relatives of patients with melanoma. In patients with dysplastic nevi and two or more first-degree relatives with cutaneous melanoma, the lifetime risk exceeds 50%. Patients with a large number (>100) of benign-appearing nevi may also be at increased risk.
Basal Cell Carcinomas
These cancers rarely metastasize or cause death, but they can be locally invasive and disfiguring. Metastasis usually occurs in patients who have delayed therapy for many years and who have large, locally invasive, eroded lesions. The risk for other skin cancers is increased because of their shared risk factors.
Several effective forms of therapy exist, all yielding a cure rate of approximately 95%: surgical excision, radiation therapy,
electrodesiccation and curettage, and cryotherapy with liquid nitrogen applied by special spray apparatus. Treatment of the 5% that recur presents a greater challenge. The cure rate of a recurrent basal cell carcinoma is about 66% when the four traditional modalities just listed are applied. A special form of micrographic surgery, Mohs surgery, is used for difficult, recurrent, or infiltrative basal cell carcinomas. In Mohs surgery, the excised tissue is examined microscopically by frozen section to determine whether the tumor has been completely removed. Additional sections of skin are removed until all the borders are histopathologically clear of tumor. With Mohs technique, cure rates of recurrent tumors exceed 90%, and those for primary tumors are better than 98%.
electrodesiccation and curettage, and cryotherapy with liquid nitrogen applied by special spray apparatus. Treatment of the 5% that recur presents a greater challenge. The cure rate of a recurrent basal cell carcinoma is about 66% when the four traditional modalities just listed are applied. A special form of micrographic surgery, Mohs surgery, is used for difficult, recurrent, or infiltrative basal cell carcinomas. In Mohs surgery, the excised tissue is examined microscopically by frozen section to determine whether the tumor has been completely removed. Additional sections of skin are removed until all the borders are histopathologically clear of tumor. With Mohs technique, cure rates of recurrent tumors exceed 90%, and those for primary tumors are better than 98%.
The use of 5-fluorouracil (5-FU) and imiquimod topically has been advocated by some physicians for the treatment of superficial basal cell carcinoma. These agents may have some role in patients with multiple superficial lesions in whom other techniques cannot easily be employed.
Squamous Cell Carcinomas
Squamous cell carcinomas may begin as actinic keratoses, of which perhaps 1 in 1,000 annually undergoes malignant change. Bowen disease represents carcinoma in situ, which may progress to a more advanced lesion if untreated.
Actinic Keratoses
Application of 5-FU cream or solution twice daily for 2 to 4 weeks or imiquimod two times weekly for 16 weeks usually results in the destruction of these lesions. Some clinically inapparent lesions will also be destroyed by this therapy when applied to a field of lesions. The patient must be warned about the impressive inflammation that occurs when 5-FU or imiquimod is used. Because 5-FU is also a photosensitizing agent, treatment in late fall or winter, when solar exposure is diminished, is preferred. Imiquimod may result in local loss of pigmentation. Other effective modalities include cryotherapy with liquid nitrogen and light desiccation. Cryotherapy may also result in local decrease in pigmentation. Promising results have been noted with Ingenol mebuate gel applied for 2 to 3 days to a field of actinic lesions, offering the advantage of short-duration treatment, which enhances compliance. Adverse effects of itching and skin irritation are usually modest. If a cutaneous horn is present, biopsy of the lesion may be warranted to rule out the presence of a squamous cell carcinoma at the base. Actinic keratoses are extremely common and usually present no great threat to life.
Bowen Disease
Bowen disease (squamous cell carcinoma in situ) represents the next grade of neoplasia in the keratinocytic line; it is substantially less common than actinic keratoses. Surgical removal of the lesions of Bowen disease is probably the most effective treatment. Alternatively, this tumor can be treated satisfactorily by cryotherapy with liquid nitrogen or electrodesiccation and curettage.
More-Advanced Squamous Cell Carcinomas
More-advanced squamous cell carcinomas are treated with surgical excision, Mohs, or radiation; the latter is usually reserved for people older than 60 years.
Melanomas
Melanomas can be divided into four histopathologic categories, each with a characteristic natural history and clinical course.
Superficial Spreading Melanoma
Superficial spreading melanoma is the most common type in the United States, representing 70% of all melanomas diagnosed. The early lesion exists for 1 to 7 years before a papule or nodule develops, which indicates that deeper penetration has occurred. Before penetration, the lesion grows superficially, and its removal during this time is associated with a 5-year survival rate approaching 100%.
Nodular Melanoma
Nodular melanoma has a poorer prognosis. It may arise de novo or within a nevus as an invasive tumor from the onset. Even when the lesion is removed soon after it becomes clinically evident, metastasis may already have occurred in a substantial proportion of patients. This type of tumor can occur on any cutaneous surface, as can superficial spreading melanoma. Nodular melanoma represents about 15% of all melanomas. Prognosis is especially poor for those lesions found on the head and neck, particularly among older men with ulcerated lesions.
Lentigo Maligna Melanoma
Lentigo maligna melanoma, the third type, accounts for about 5% of melanomas and occurs on sun-damaged skin of older patients. It is the least aggressive of the melanomas and may be present for five or more years before dermal invasion develops. Prior to invasion, the lesion is termed lentigo maligna. Local excision with 5 to 10 mm margins is usually satisfactory for the treatment of lentigo maligna. In lentigo maligna melanoma, excision with 1 cm or wider margins is advocated. Surgical outcome in this type of tumor is usually favorable, although local recurrence is sometimes seen. It is unusual for a patient to die of disseminated lentigo maligna melanoma.
Acral Lentiginous Melanoma
Acral lentiginous melanoma occurs on palms, soles, subungual areas, and mucous membranes. This is the most common type to affect Blacks and East Asians, but it may also occur in Whites. The lesion begins as a flat, pigmented lesion that may be irregular in its border and pigment pattern. Early biopsy is essential to achieving cure before metastasis has occurred.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree