CHAPTER 130
Scaphoid Fracture
Presentation
The patient (usually 14 to 40 years of age) fell on an outstretched hand (FOOSH) with the wrist held rigid and extended and now complains of decreased range of motion and a deep full pain in the wrist, particularly on the dorsal radial side. Physical examination discloses no deformity or ecchymosis but shows pain with motion and palpation and often swelling. Swelling may be seen, especially in the anatomic snuff box, the hollow seen on the radial aspect of the wrist when the thumb is in full extension (between the tendon of the extensor pollicis longus and the tendons of the abductor pollicis longus and extensor pollicis brevis) (Figure 130-1). The pain, which may be mild, is worsened by gripping or squeezing.

Figure 130-1 Examine for swelling or tenderness within the anatomic snuff box.
What To Do:
 For comfort, apply a cold pack and a temporary splint or sling and administer any necessary analgesic.
For comfort, apply a cold pack and a temporary splint or sling and administer any necessary analgesic.
 A thorough history and well-performed physical examination, along with a high index of suspicion, are necessary to make the diagnosis.
A thorough history and well-performed physical examination, along with a high index of suspicion, are necessary to make the diagnosis.
 The classic hallmark of anatomic snuff box tenderness on examination is a highly sensitive (90%) indication of scaphoid fracture, but it is nonspecific (specificity, 40%). Other physical examination maneuvers should be performed. Tenderness of the scaphoid tubercle (i.e., extend the patient’s wrist with one hand and apply pressure to the tuberosity at the proximal wrist crease with the opposite hand [Figure 130-2]) has a sensitivity of 87% but is more specific than snuff box tenderness (57%). Absence of tenderness with these two maneuvers makes a scaphoid fracture highly unlikely.
The classic hallmark of anatomic snuff box tenderness on examination is a highly sensitive (90%) indication of scaphoid fracture, but it is nonspecific (specificity, 40%). Other physical examination maneuvers should be performed. Tenderness of the scaphoid tubercle (i.e., extend the patient’s wrist with one hand and apply pressure to the tuberosity at the proximal wrist crease with the opposite hand [Figure 130-2]) has a sensitivity of 87% but is more specific than snuff box tenderness (57%). Absence of tenderness with these two maneuvers makes a scaphoid fracture highly unlikely.

Figure 130-2 Palpating the scaphoid tubercle while extending the wrist.
 Pain with the scaphoid compression test (applying a longitudinal axial load to the scaphoid via the proximal phalanx of the thumb through to the first metacarpal [Figure 130-3]) may also be helpful in identifying an underlying scaphoid fracture. Another maneuver that suggests fracture of the scaphoid is pain in the snuff box with pronation of the wrist, followed by ulnar deviation (52% positive predictive value, 100% negative predictive value) (Figure 130-4).
Pain with the scaphoid compression test (applying a longitudinal axial load to the scaphoid via the proximal phalanx of the thumb through to the first metacarpal [Figure 130-3]) may also be helpful in identifying an underlying scaphoid fracture. Another maneuver that suggests fracture of the scaphoid is pain in the snuff box with pronation of the wrist, followed by ulnar deviation (52% positive predictive value, 100% negative predictive value) (Figure 130-4).

Figure 130-3 The scaphoid compression test.

Figure 130-4 Pronation of the wrist, followed by ulnar deviation.
 Be vigilant for associated injuries, such as fractures of the distal radius, lunate, or radial head at the elbow, scapholunate dissociation, or median nerve injury.
Be vigilant for associated injuries, such as fractures of the distal radius, lunate, or radial head at the elbow, scapholunate dissociation, or median nerve injury.
 When any clinical suspicion for a scaphoid fracture is raised, obtain radiographs of the wrist that include a scaphoid view (a posteroanterior view in ulnar deviation). Conservative estimates suggest that 10% to 20% of scaphoid fractures are not visible on any view in the acute setting (Figure 130-5). An abnormal scaphoid “fat stripe” or “stripe sign” may appear as an outward bulging radiolucent line in the soft tissue adjacent to the scaphoid, representing bleeding within the joint space, and may indicate the presence of an occult fracture.
When any clinical suspicion for a scaphoid fracture is raised, obtain radiographs of the wrist that include a scaphoid view (a posteroanterior view in ulnar deviation). Conservative estimates suggest that 10% to 20% of scaphoid fractures are not visible on any view in the acute setting (Figure 130-5). An abnormal scaphoid “fat stripe” or “stripe sign” may appear as an outward bulging radiolucent line in the soft tissue adjacent to the scaphoid, representing bleeding within the joint space, and may indicate the presence of an occult fracture.
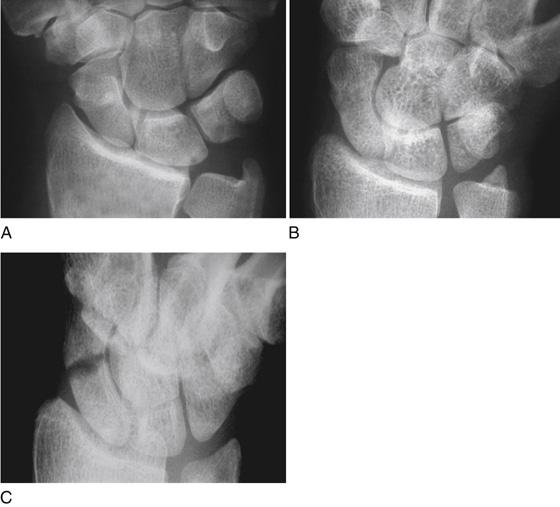
Figure 130-5 A, B, and C, Radiograph of the wrist demonstrating a scaphoid fracture—identified (with certainty) on one projection only. (Adapted from Raby N, Berman L, de Lacey G: Accident and emergency radiology. Philadelphia, 2005, Saunders.)
 When there is scaphoid tenderness or pain elicited by any of the aforementioned diagnostic maneuvers but radiographs are negative, the wrist should still be immobilized in a short-arm thumb-spica splint with the wrist in mild extension and the thumb interphalangeal joint free (Figure 130-6). Follow-up radiographs at 2 weeks may reveal bone resorption adjacent to a fracture site or early callus formation if an occult fracture was present; otherwise, all splinting can be removed. Arrange for follow-up within 5 to 7 days.
When there is scaphoid tenderness or pain elicited by any of the aforementioned diagnostic maneuvers but radiographs are negative, the wrist should still be immobilized in a short-arm thumb-spica splint with the wrist in mild extension and the thumb interphalangeal joint free (Figure 130-6). Follow-up radiographs at 2 weeks may reveal bone resorption adjacent to a fracture site or early callus formation if an occult fracture was present; otherwise, all splinting can be removed. Arrange for follow-up within 5 to 7 days.
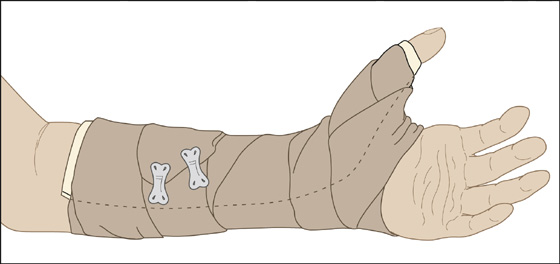
Figure 130-6 Splint or cast the wrist in mild extension, including the thumb but leaving the interphalangeal (IP) joint free.
 When occult fractures are suspected in athletes, individuals opposed to wearing a splint for 2 weeks, or workers who require a more urgent diagnosis, a bone scan, CT, or MRI may be considered for additional imaging. A bone scan may be positive 24 hours after the injury; however, it can take 4 days for abnormal uptake to appear at the fracture site. A normal bone scan 4 days after injury is accurate in excluding scaphoid fracture. MRI is very sensitive and will have an abnormal bone marrow signal 48 hours postfracture; however, it may not clarify fracture displacement. A CT scan gives clearer fracture visualization and is more accurate for determination of displacement.
When occult fractures are suspected in athletes, individuals opposed to wearing a splint for 2 weeks, or workers who require a more urgent diagnosis, a bone scan, CT, or MRI may be considered for additional imaging. A bone scan may be positive 24 hours after the injury; however, it can take 4 days for abnormal uptake to appear at the fracture site. A normal bone scan 4 days after injury is accurate in excluding scaphoid fracture. MRI is very sensitive and will have an abnormal bone marrow signal 48 hours postfracture; however, it may not clarify fracture displacement. A CT scan gives clearer fracture visualization and is more accurate for determination of displacement.
 When initial radiographs demonstrate a scaphoid fracture, the treatment is dictated by the degree of injury. For nondisplaced fractures (<1 mm of fracture separation without any visible step-off on any radiographic view), the treatment of choice is a long-arm thumb-spica splint, with follow-up with a hand surgeon or orthopedist arranged for 5 to 7 days after treatment.
When initial radiographs demonstrate a scaphoid fracture, the treatment is dictated by the degree of injury. For nondisplaced fractures (<1 mm of fracture separation without any visible step-off on any radiographic view), the treatment of choice is a long-arm thumb-spica splint, with follow-up with a hand surgeon or orthopedist arranged for 5 to 7 days after treatment.
 For fractures with significant displacement, angulation, or comminution or for fractures involving the proximal pole of the scaphoid, immediate orthopedic or hand surgeon consultation should be made.
For fractures with significant displacement, angulation, or comminution or for fractures involving the proximal pole of the scaphoid, immediate orthopedic or hand surgeon consultation should be made.
 Patients who are placed in a splint should be given standard cast instructions.
Patients who are placed in a splint should be given standard cast instructions.
 It is very important to explain to the patient the common difficulty of visualizing scaphoid fractures on radiographs, the common difficulty in healing of scaphoid fractures because of variable blood supply, and the resultant necessity of keeping this splint or cast in place until reevaluated by a specialist.
It is very important to explain to the patient the common difficulty of visualizing scaphoid fractures on radiographs, the common difficulty in healing of scaphoid fractures because of variable blood supply, and the resultant necessity of keeping this splint or cast in place until reevaluated by a specialist.
 Provide a sling to keep the elbow flexed at 90 degrees, and prescribe acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), adding narcotics when necessary.
Provide a sling to keep the elbow flexed at 90 degrees, and prescribe acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), adding narcotics when necessary.
 As with any acute injury, have the patient apply ice for 15 to 20 minutes three or four times per day if this provides comfort, and maintain elevation above the level of the heart as much as possible.
As with any acute injury, have the patient apply ice for 15 to 20 minutes three or four times per day if this provides comfort, and maintain elevation above the level of the heart as much as possible.
What Not To Do:
 Do not assume a wrist injury is “just a sprain” when radiographs are negative. Any wrist injury with significant tenderness, pain on range of motion, and swelling should be splinted and referred for further evaluation.
Do not assume a wrist injury is “just a sprain” when radiographs are negative. Any wrist injury with significant tenderness, pain on range of motion, and swelling should be splinted and referred for further evaluation.
Discussion
Of all the wrist injuries encountered in the emergency department, fracture of the scaphoid is one of the most commonly missed. Radiographic findings can be subtle or even absent. Accurate early diagnosis of scaphoid fracture is critical, however, because the morbidity associated with a missed or delayed diagnosis is significant and can result in long-term pain, loss of mobility, decreased function, and litigation.
The scaphoid bone is unique for two reasons. First, it spans both the proximal and distal carpal row, making an intact scaphoid imperative for carpal stability. Second, the scaphoid relies on an interosseous blood supply that enters distal to its middle third and provides the sole blood supply to its proximal pole. Therefore fractures through the proximal third disrupt the blood supply and are prone to osteonecrosis and nonunion.
The location of the scaphoid fracture (proximal, middle, or distal third) depends mostly on the position of the forearm at the time of the injury. Fracture of the middle third is most common (80%), followed by fractures of the proximal third (15%), fractures of the distal third (4%), and fractures of the distal tubercle (1%).
In general, the more proximal, oblique, or displaced the fracture, the greater the risk of interrupting the blood supply. Distal fractures heal most rapidly, often within 6 weeks. In contrast, proximal fractures, because of the tenuous blood supply, may take 6 months. Nonunion complicates up to 20% to 30% of proximal-third fractures and 10% to 20% of middle-third fractures. Nonunion of distal-third fractures is relatively rare. In addition to nonunion, patients are also at risk for the development of avascular necrosis of the scaphoid. This outcome occurs in approximately 10% of proximal-pole fractures and 5% of middle-third fractures.
Open reduction and internal fixation has now become standard for all proximal-pole fractures and is required for unstable fractures. Also consider surgical referral for any athlete or manual laborer, because many surgeons offer percutaneous screw fixation techniques to these patients to decrease the time of cast immobilization.
Distal radius fractures also occur with FOOSH injuries. The patient presents with pain, swelling, ecchymosis, and tenderness about the wrist. A Colles fracture, the most common distal radius fracture, is a closed fracture of the distal radial metaphysis in which the hand and wrist are dorsally displaced.
Stable distal radius fractures may be managed in a short-arm splint or short-arm cast. All others should be referred for reduction and fixation. A stable distal radius fracture is extra-articular, without comminution, and with minimal or no displacement. Certainly, fractures must be referred for orthopedic consultation if there is greater than 20 degrees of dorsal tilt, loss of radial inclination (20 to 30 degrees need to be maintained), articular step-off greater than 2 mm, or radial shortening greater than 5 mm.
Stable distal radius fractures in children (e.g., torus or “buckle” fractures, Salter I or II fractures) may be treated with a short-arm cast for 4 to 6 weeks. One study demonstrated that children with buckle fractures had a good or excellent outcome, regardless of whether they were treated with a cast or splint.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


